The basis for successful digitization is not software, but good organization. Lean management involves all employees in order to optimize work processes.
Today, digitization is often seen as a panacea. But when implementing digitization projects, the correct sequence is crucial. Existing processes must first be checked for problems and simplified. This ensures that bad or superfluous processes are not unnecessarily digitized. Lean management as an established optimization philosophy helps to master this first step.
Digitalization as a beacon of hope
Patients’ expectations of their physicians have risen in recent years. Today’s patients are informed, self-directed and expect high-quality advice and treatment. This includes professional practice management that enables efficient workflows. In order to meet these expectations, high hopes are being placed in the “digital medical practice”. It is hoped to increase efficiency, improve networking between practices and save costs.
But digital solutions often do not have the desired effect. This may be because existing analog processes are digitized unchanged. In order for the benefits of a digital process to take hold, the sequence of implementation of digitization projects is crucial. First and foremost, the following credo should be kept in mind: “Organization before software”. In other words, before a practice starts to look at digitizing processes, it needs to look at existing processes. Current analog or semi-digital processes and structures will be broken up, combed through and put to the test. Because: A bad process remains a bad process, even if it is digitized.
The EVA principle (EVA=eliminate, simplify, automate) helps with implementation: After identifying the most important problem areas, completely superfluous activities (e.g. duplications) are eliminated from the process. If this is not possible, the processes are designed to be as simple as possible. This can be done, for example, through standardization of forms, visual management or process guides. This can already avoid many errors, queries and unnecessary walking. Only when these two steps have been carried out cleanly can the automation and digitization of the process begin. Adhering to this sequence is critical to success, as the most sophisticated software is of little use if it was developed for poor processes.
| Implementation tip The best way to learn Lean is to try the approach iteratively. A project should be chosen that can be clearly delineated, is not too extensive, and is still useful, e.g., improving incoming mail management or optimizing medication ordering. These initial successes help to understand how Lean works and to foster motivation for further projects. |
Performance goals – When is a practice successful?
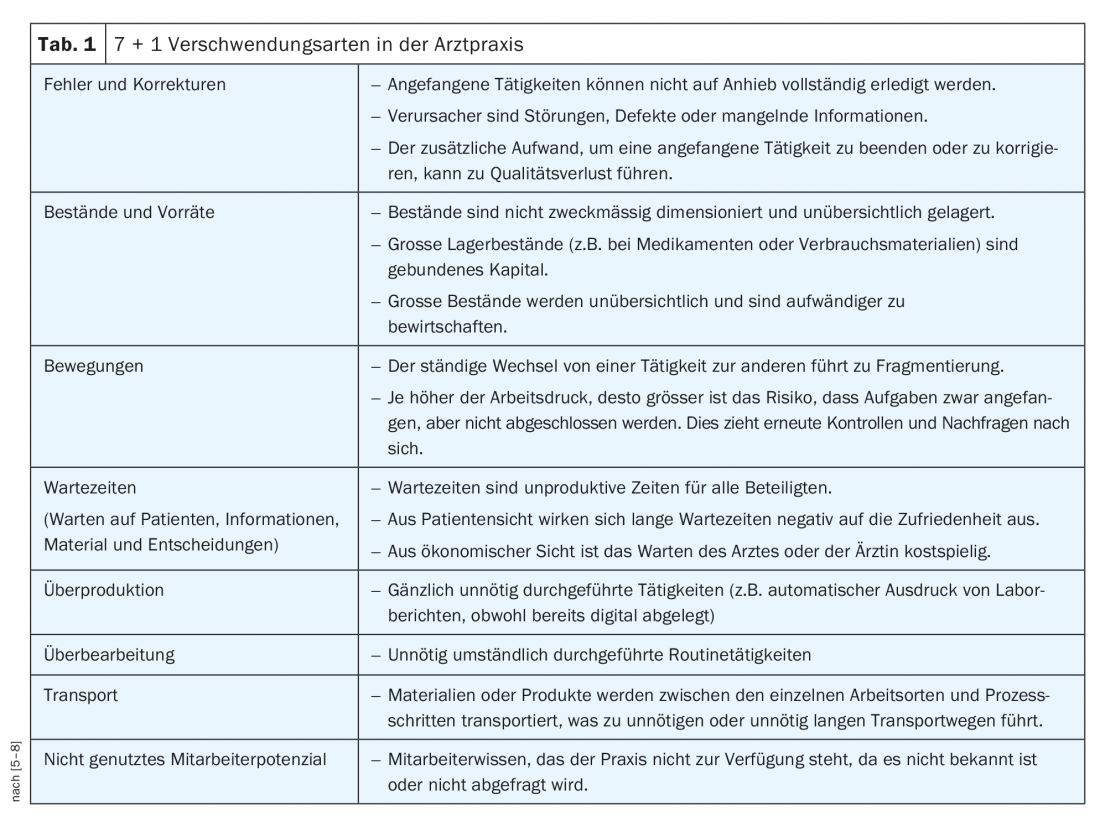
Inefficient processes can be a problem in medical practices. In lean management, this is referred to as “muda” (waste). This includes all activities that do not contribute directly to value creation (Tab. 1) and thus lead, among other things, to waiting times and hectic activity for staff. Many physicians follow fixed guidelines for diagnosis and therapy for certain diseases. If a similarly clear structure for the daily (e.g. non-medical) work is missing, a lot of time and therefore money is lost due to inefficiency.
The formula for eliminating this waste from work processes is the management method Lean Management, which originated in Japan. The optimization philosophy has also become established in the healthcare sector over the past 20 years. So far, lean management has mainly been practiced in hospitals. However, medical practices in particular are very well suited for the consistent implementation of the philosophy due to their organizational-structural framework conditions [1].
Lean management is essentially about identifying problems in the process, implementing optimization potential and avoiding waste. Lean puts the well-being of the patient first. The following applies: Quality is defined by the patient. This is especially difficult in a doctor’s office because the patient can often only subjectively judge the quality of a doctor’s treatment. However, studies show that short waiting times, friendly interaction and a pleasant atmosphere have an equally high influence on patient satisfaction as the perceived quality of the medical service [2].
Procedure and practical implementation
Changing a practice entirely to Lean is a years-long effort. Because that means a real culture change, and culture changes always take years. There are two basic approaches to introducing change: Process Reengineering and “Kaizen” [3] (Fig. 1) . Process reengineering (also called the “big bang” approach) uses a high level of resources to try to radically rethink and redesign processes in a relatively short time. While this approach has a lot of potential for change, it also carries high risks. In practice, this approach is found rather rarely and only in organizations where the pressure to change – e.g. due to cost pressure – is very high.
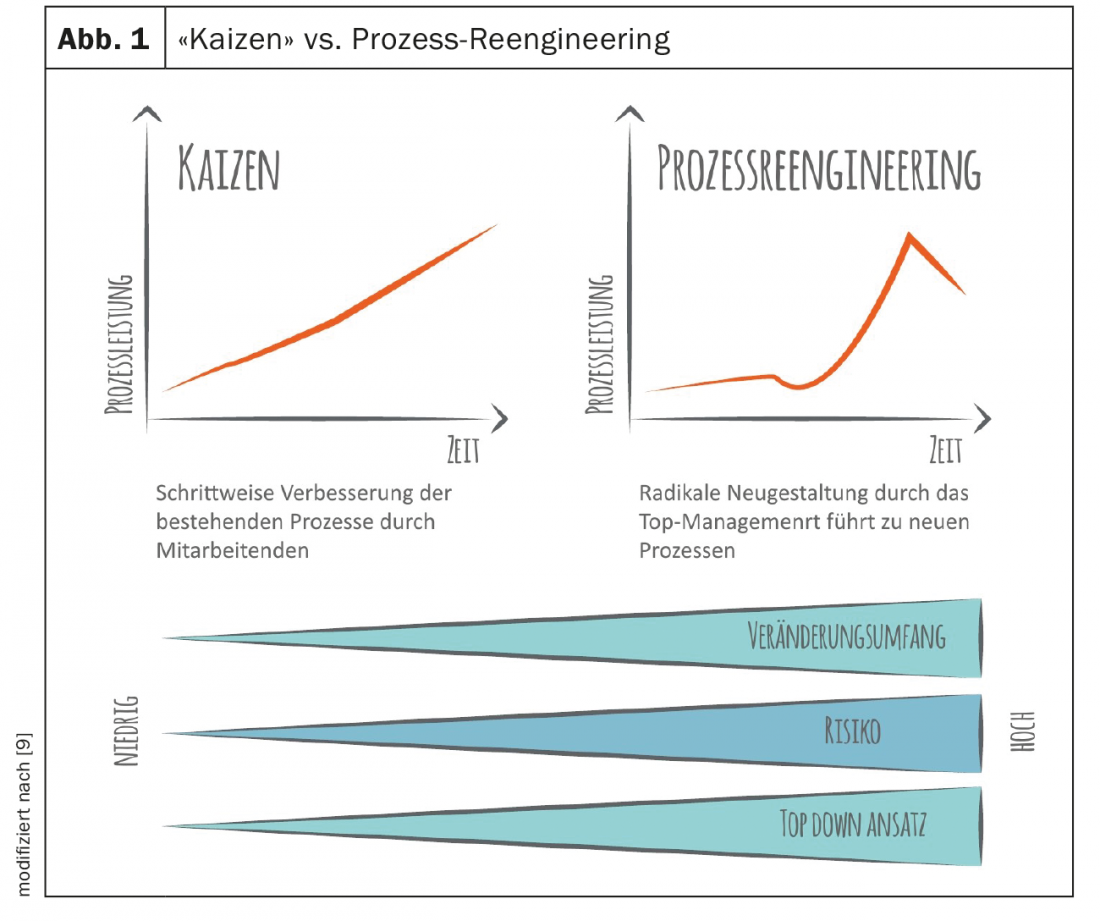
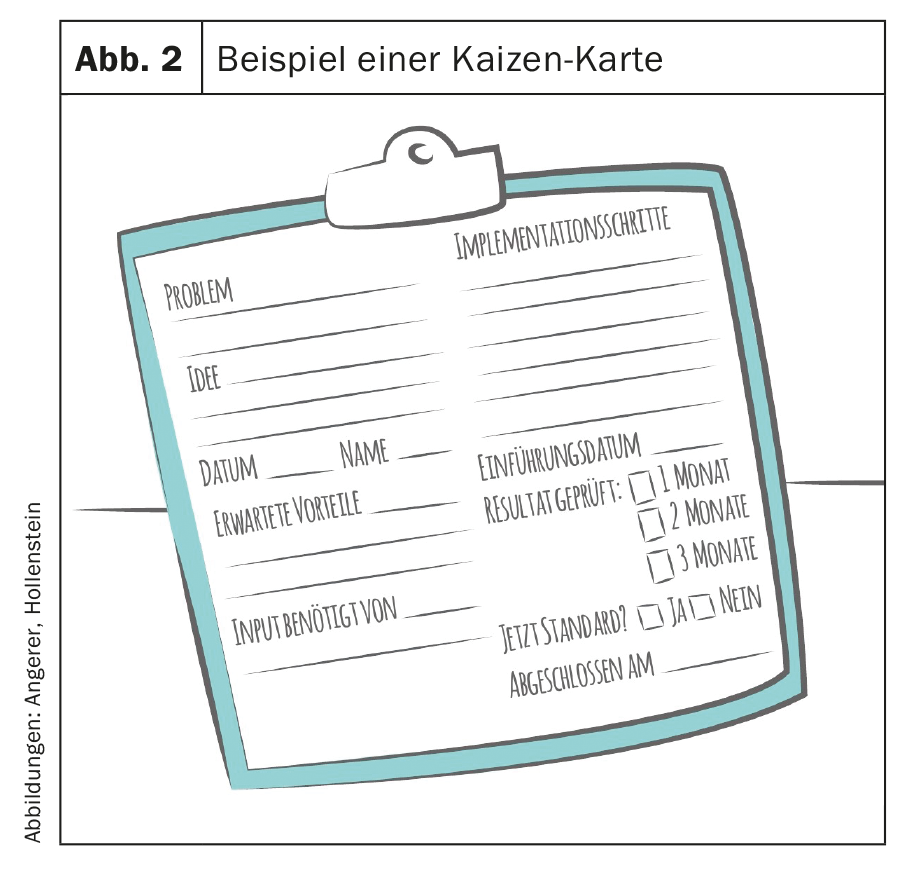
For most practices, a less radical approach is recommended. “Kaizen” (Japanese for “change for the better”) is the methodology of small steps. The three core pillars of the approach are: a) Involve all employees, b) change in small steps and c) never stop improving yourself. One useful tool is white boards, called “kaizen boards,” on which employees’ ideas are systematically promoted [4]. During the week, all employees are encouraged to write down their ideas on small cards and post them on the Kaizen board. In a weekly meeting, these ideas are discussed for five minutes and jointly evaluated by the team (Fig. 2).
Implementation of lean tools in medical practices
Standardize treatment rooms: The layout of the equipment in each treatment room should be uniform. Shelves and drawers in each room are assigned defined accessories and materials. In the storage area, each drawer is labeled with the name of the items located there. The outlines of important, frequently used devices can be traced with shadow boards in the respective places. To maintain this ideal state, a checklist is used.
Use treatment rooms variably: Instead of assigning treatment rooms to different activities, use them variably. Such spaces increase flexibility and reduce the downtime involved in reserving them for specific people and activities. Traditional medical practices often have fixed room assignments (waiting room, consultation room, ECG room, blood collection room, etc.). This allocation leads to bottlenecks when the corresponding room is occupied, which means unnecessary trips and room changes for the patient. It is recommended that medical measures are consistently carried out in the treatment room, which the patient enters immediately upon arrival and leaves the practice with all necessary information (incl. follow-up appointment, etc.). All actions on the patient are performed in this room. In lean management, the service always comes to the patient, not the other way around [1].
Sensible time buffers: after every third or fourth patient, a short open slot is set in the schedule. This buffer may be necessary because patient-generated variance usually cannot be completely eliminated. The physician uses this time to complete documentation, return phone calls, answer questions from office staff, or perform other short tasks. Work to be completed during the time buffer should be clearly delineated and prioritized.
Take-Home Messages
- The goal of a good medical practice is to do a good job for patients. In addition to high medical quality, efficient processes are also crucial for this.
- To achieve this, work processes must be systematically reviewed and improved with the active participation of employees.
- Lean management as a philosophy involves all employees, because only together can this improvement be shaped. Various methods and tools, such as the Kaizen board, support the practice in this regard.
- Once the processes have reached a good level, digitization can begin according to the EVA principle. The foundation for successful digitization is not software, but good organization.
Literature:
- Bagattini MF: Lean management – also beneficial in medical practice! SAEZ 2018; 98(10): 322-323.
- Angerer A, Liberatore F: Management in health care: Switzerland. Berlin: MWV Medizinisch Wissenschaftliche Verlagsgesellschaft, 2018.
- Angerer A, Vetterli C: The Transformation Master Plan (TMP). In: Angerer A, ed: LHT-BOK Lean Healthcare Transformation Body of Knowledge, Edition 2018-2019. Zurich: CreateSpace Independent Publishing Platform, 2018.
- Angerer A, Schmidt R: Kaizen. In: Angerer A, ed: LHT-BOK Lean Healthcare Transformation Body of Knowledge, Edition 2018-2019. Zurich: CreateSpace Independent Publishing Platform, 2018.
- Angerer A, et al: LHT-BOK Lean Healthcare Transformation Body of Knowledge Edition 2018-2019. Zurich: CreateSpace Independent Publishing Platform, 2018.
- Ehbets R: Lean Management. Waste factors in medical practice. http://mpa-community.ch/lean-management-verschwendungfaktoren-in-der-arztpraxis, last accessed 07.03.19.
- Endsley S, Magill MK, Godfrey MM: Creating a lean practice. Fam Pract Manag 2006; 13(4): 34-38.
- Thill KD: The easy way to perfect organization in the medical practice. A practical guide to self-optimization with tips from doctors for doctors. Kindle Edition, 2016.
- Becker T: Optimizing processes in production and supply chain. Berlin: Springer, 2008.
FAMILY PRACTICE 2019; 14(4): 8-10











