“Red eye” is a symptom that is common in family practice. The underlying causes can be very diverse. Depending on the clinical picture, treatment by the general practitioner is possible or a referral to the ophthalmologist is necessary. At Medidays in early September, practical examples were used to explain in which cases such a referral is indicated.
“Red eye” is a symptom that is common in family practice. The underlying causes can be very diverse. Depending on the clinical picture, treatment by the general practitioner is possible or a referral to the ophthalmologist is necessary (Tab. 1). Especially in the case of eye complaints in the context of systemic diseases, interdisciplinary cooperation is something very important. Regarding diagnostics, it is important to distinguish between hyposphagma (bleeding under the conjunctiva) and red eyes due to a dilated vessel, and in the case of the latter, it is important to clarify whether the symptoms are infectious or non-infectious.

Cases that can be cared for by the primary care physician are, for example, when there is a red eye due to hyposphagmia with otherwise bland findings (painless, visual acuity normal). As therapy, tear substitutes (e.g. eye drops with hyaluronic acid) and a caring eye ointment should be sufficient. However, if there is evidence of infection, referral to the ophthalmologist should be made. Infectious keratoconjunctivitis may involve viral, bacterial, mycotic, or parasitic agents. The history can give an indication of viral conjunctivitis: typically, one eye is affected first and, with some delay, the other eye as well. If the etiology is unclear, Karin Küper, MD, senior physician at the Eye Clinic of the University Hospital Zurich, advises against “blind” local steroid administration and recommends referral to an ophthalmologist. She points out that, for example, in the case of massive purulent changes, examination by an ophthalmologist is very important to diagnose and treat the infection in time to prevent corneal melting (possible within hours with purulent secretions).
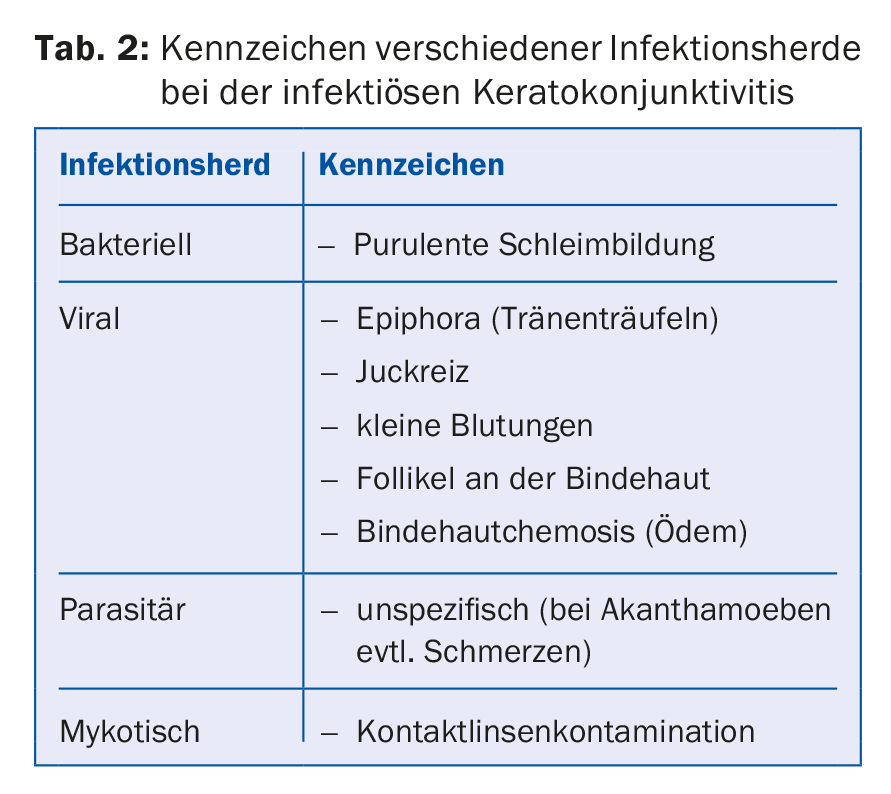
One of the most important decision criteria for referral to an ophthalmologist is the presence of corneal involvement, according to Prof. Dr. Dr. med. Jens Funk, Deputy Clinic Director and Chief Physician at the Eye Clinic of the University Hospital Zurich. In cases of keratitis or keratoconjunctivitis (Tab. 2), referral to an ophthalmologist should be made as soon as possible. A diagnostic feature here is that the reflex image of the cornea is not smooth but torn. For example, pseudomonas keratitis with lytic keratitis is a case where referral to an ophthalmologist should be made as soon as possible. The same applies if a fungal infection is suspected (e.g. Fusarium keratitis).
Differential diagnosis: diseases with eye involvement
To elicit etiologic factors, a careful history in the primary care physician’s office is critical [1]. Among various other factors, contact lens history and stays in areas with precarious hygienic conditions can provide information about possible causes of infection. The course of symptoms may also provide clues to the nature of the underlying problem (e.g., fungal infections: prolonged course; viral infections: first one eye and, with some delay, the other eye affected).
“A big chapter is allergic eye diseases,” Dr. Küper said. The prevalence is very high at 40% in the Western world. If acute allergic rhinoconjunctivitis is present, local and systemic treatment with mast cell stabilizers, antihistamines, or “dual action” preparations (e.g., olopatadine, ketotifen) can be used. If pain occurs in the further course or there is no improvement, a referral to the ophthalmologist is advisable. Referral to an ophthalmologist is indicated, especially in chronic cases, contact lens wearers, atopic patients, children, and patients with pain.
Sicca syndrome is one of the most common conditions seen in ophthalmology. Keratoconjunctivitis sicca is characterized by reduction of tear production. “One in five patients in an ophthalmologist’s office has dry eye,” Dr. Küper said. As treatment by the general practitioner, in such cases with proven rosacea disease or chronic posterior blepharitis with meibomstasis, systemic therapy with tetracyclines can be given for a period of two to three months. In case of therapy resistance or pain, referral to an ophthalmologist is indicated.
Other diseases in which eye damage often occurs:
- Graft-versus-host disease (eye involvement is present in 50-80% of cases).
- Peripheral corneal ulceration (as an isolated corneal problem vs. in the context of a systemic disease).
- Ocular pemphigoid (heterogeneous group of autoimmune diseases with ocular involvement in 60-77% of cases).
- Steven-Johnson syndrome (a mostly drug-induced mucosal reaction with ocular involvement in 69-82% of cases).
- Intraocular inflammation – uveitis (50% of cases idiopathic, 50% of cases in the context of various diseases. In case of pain and reduction of visual acuity: immediate referral to an ophthalmologist).
- Arterio-venous sinus cavernosus fistula
- Conjunctival tumors (benign and malignant).
Eye damage caused by modern technologies: Are computer games and laser pointers harmful?
There are controversial findings on the question of whether computer games have a harmful effect on the eyes. For example, there are studies that showed that computer games can lead to an increase in myopia development [2] and tear film instability [3]. On the other hand, there are also computer games which are used for therapeutic purposes, e.g. for brain damage with visual field loss.
According to Prof. Dr. med. Funk, laser pointers are not dangerous per se if the manufacturers observe the prescribed limits. Unfortunately, this is often not the case, he said, and even an exposure of 0.25 sec from a laser pointer of 10 milliwatts instead of the prescribed upper limit of 1 milliwatt of power can lead to permanent anatomical damage. There are models on the market with up to 2000 milliwatts of power.
Eye damage from psychotropic drugs and yoga
There are cases in which topipramate (anticonvulsant) can cause a glaucoma attack, although this is a rare side effect of this medication. To reduce this risk, a measurement of the eye pressure should be performed in addition to a careful medical history before and after prescribing psychotropic drugs. In addition, he said, it is important to educate patients about the potential risks and side effects of psychotropic drugs (e.g., pain, nausea, vomiting, vision deterioration). Certain yoga exercises (e.g., head down) can also be dangerous for glaucoma patients, as the risk for a change in ocular chamber pressure increases.
Source: Medidays Zurich, September 4-8, 2017, Zurich
Literature:
- Frings A, Gerling G, Schargus M: Red Eye: A Guide for Non-specialists. Deutsches Ärzteblatt 2017; 114 (17): 302-312.
- Deng L, Gwiazda J, Thorn F: Children’s refractions and visual activities in the school year and summer. Optometry and Vision Science 2010; 87(6): 406-413.
- Cardona G, et al: Blink rate, blink amplitude and tear film integrity during dynamic visual display terminal tasks. Current Eye Research 2011; 36 (3): 190-197.
HAUSARZT PRAXIS 2017; 12(10): 39-41











