Although dementia is not one of the most common neurological diseases, it is already a relevant problem today and will become much more important due to demographic developments.
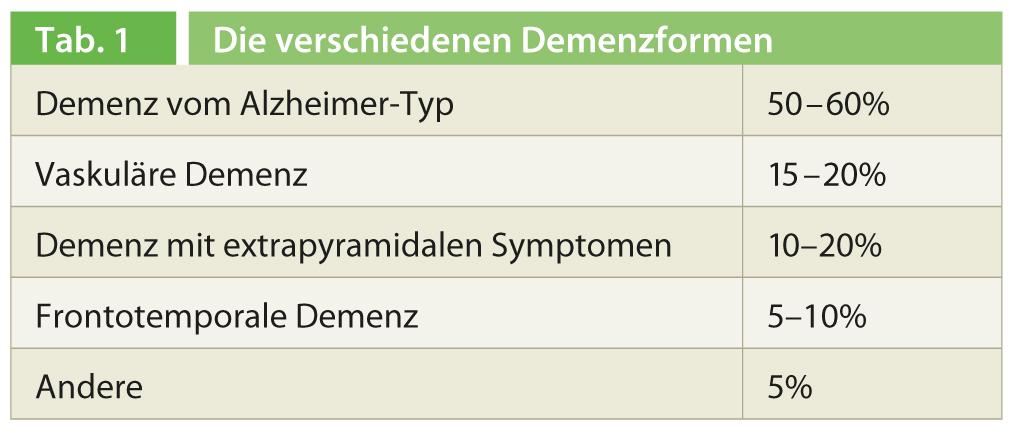
Dementia is a chronic progressive brain disease with a disturbance in several cognitive spheres such as memory, thinking, orientation, comprehension, calculation, learning ability, language, speech and judgment. The consciousness of people with dementia is not clouded and sensory perception is preserved; on the other hand, changes in emotional control, social behavior, and/or motivation are observed with the corresponding effects on everyday life. According to the ICD-10 definition, this condition must persist for a period of at least six months for a diagnosis of dementia to be made. In addition to cognition, dementia affects various daily living skills and bodily functions. At 50-60%, dementia of the Alzheimer type is by far the most common form of dementia (Table 1).
Diagnostics
“In dementia diagnostics, you are in demand as a practitioner. You know the patients and their families, and you are usually the first point of contact when a person’s behavior changes,” says Prof. Hans Jung, MD, University Hospital Zurich. In addition to the medical history and the history of others, the following measures can be easily performed for initial dementia screening in any practice:
- the collection of an orienting internal, neurological and psychopathological report,
- Basic laboratory tests (electrolytes, thyroid values, kidney values, vitamin B12, folic acid, HIV, syphilis) as well as
- one or more standardized short tests (Mini-Mental-State, Clock Test).
If necessary, imaging may also be indicated. Depending on the situation, further diagnostic steps, such as more detailed neurophysiological tests, may be taken in collaboration with a specialist. “Especially in younger patients – and by that I mean patients under the age of 65 or 70 (!) – as well as in cases of diagnostic uncertainty, CSF diagnostics, EEG, or further imaging with PET or SPECT may also be indicated,” Prof. Jung continued. In CSF diagnostics, inflammation levels, tau, phospho-tau, β-amyloid, and protein 14-3-3) are of particular interest.
Early symptoms, such as mild cognitive impairment affecting only memory, may be precursors to Alzheimer’s dementia. 20-30% of patients with so-called MCI (Mild Cognitive Imp airement) eventually develop Alzheimer’s dem entia. Theoretically, it would be possible to identify patients who will develop AD at this early stage using specific markers in CSF and PET/SPECT, but practically this is not practical until preventive treatment is available.
Therapeutic options
Despite intensive research, to date only medications are available for symptomatic treatment, in addition to psychosocial support for patients and their families. Significant positive effects on dementia symptoms were demonstrated for both acetylcholinesterase inhibitors (rivastigmine, galantamine, donezepil) and memantine. The former are indicated for mild to moderate AD, the latter for moderate to severe AD.
With the help of acetylcholinesterase inhibitors, cholinergic transmission in the brain, which is reduced in Alzheimer’s dementia, can be improved again. Although the course of the disease cannot be stopped, the condition can be significantly improved and stabilized, so that the onset of independence and the need for care can be delayed [1, 2]. Therefore, if relevant deficits exist, a trial of these drugs should be undertaken relatively early after diagnosis.
Cholinergic side effects such as nausea, vomiting, and diarrhea are relatively common among acetylcholinesterase inhibitors, most frequently with rivastigmine, although this applies only to the oral formulation. Under the rivastigmine patch, which has been available for several years, the side effect rate is significantly lower and only minimally higher than under placebo [3]. In addition, the patch is available in two doses (9.5 mg/24h and 13.3 mg/24h), so that an additional benefit in terms of efficacy can be achieved with the higher-dose patch while maintaining the same side effect rate [4].
Memantine is particularly effective in the middle and late stages of Alzheimer’s dementia and can contribute to a significant improvement in the care situation by positively influencing behavioral disturbances. “Studies clearly show that a combination of memantine with an acetylcholinesterase inhibitor would be useful, but unfortunately this combination is not yet approved, so you have to apply for it individually in each case,” the speaker concluded [5].
Source: Lunchsymposium, Medidays 2013, September 2-6, 2013, University Hospital Zurich.
Literature:
- Birks J: Cholinesterase inhibitors for Alzheimer’s disease. Cochrane Database of Systematic Reviews 2006: CD005593.
- Birks J: Cholinesterase inhibitors (ChEIs), donepezil, galantamine and rivastigmine are efficacious for mild to moderate Alzheimer’s disease. Cochrane Summaries. Published Online: May 16, 2012.
- Winblad B, et al: Caregiver preference for rivastigmine patch relative to capsules for treatment of probable Alzheimer’s disease. Int J Geriatr Psychiatry 2007; 22: 485-491.
- Cummings J, et al: Randomized, double-blind, parallel-group, 48-week study for efficacy and safety of a higher-dose rivastigmine patch (15 vs. 10 cm2) in Alzheimer’s disease. Dement Geriatr Cogn Disord 2012; 33: 341-353.
- Farrimond LE, et al: Memantine and cholinesterase inhibitor combination therapy for Alzheimer’s disease: a systematic review. BMJ Open 2012;2. pii: e000917.
HAUSARZT PRAXIS 2013, Vol. 8, No. 9











