In 1896, a form of chronic infantile rheumatism was first noted in which symptoms of massive general inflammation were present in addition to arthritis. The disease was long referred to as Still’s syndrome or Still’s disease and was classified as a form of juvenile arthritis. With the classification of Juvenile Idiopathic Arthritis (JIA), the disease was classified as Systemic JIA (SJIA). Many children have SJIA without arthritis, called juvenile still syndrome (jSD). The article provides an overview of the infantile and adult forms of Still’s syndrome.
In 1896, the English pediatrician Georg Frederic Still described for the first time a form of chronic infantile rheumatism in which, in addition to arthritis, there were also symptoms of massive general inflammation [1]. The disease was long referred to as Still’s syndrome or Still’s disease and was classified as a form of juvenile arthritis. With the classification of Juvenile Idiopathic Arthritis (JIA) by ILAR [2], the disease was classified as Systemic JIA (SJIA). Many children have SJIA without arthritis; we then refer to it as juvenile Still ‘s disease ( jSD) [3]. Despite isolated case reports, it was not until 1971 that a systematic description of adult onset Still’s disease ( AOSD) was published by the English rheumatologist E.G.L. Bywaters [4].
SJIA, jSD as infantile forms, and AOSD have other differences in addition to different times of initial manifestation, but share many similarities. This summary provides an overview of the infantile and adult forms of Still’s syndrome.
Pathogenesis
SJIA and AOSD are distinguished from the other inflammatory arthritides by the fact that, according to current pathogenetic understanding, the autoinflammatory component is more prominent than the autoimmune component. Historically, SJIA, like all other subtypes of JIA, has been classified as rheumatic diseases of childhood and adolescence in the autoimmune group. However, SJIA is now understood to be an autoinflammatory disease [5]. “Autoinflammatory” diseases ( AID) are usually the result of malfunctions of the innate immune system. Many AIDs have monogenetic causes, i.e. they are based on mutations of one of the genes encoding proteins or regulatory factors in proinflammatory signal transduction pathways of the innate immune system. Monogenic autoinflammatory diseases: here, a monogenetic dysregulation of the IL-1 signaling pathway may be causative. These include cyropyrin-associated periodic syndromes (CAPS) [6,7], familial Mediterranean fever (FMF) [7,8], and mevalonate kinase deficiency (MKD) [9]. Other pathomechanisms are found in tumor necrosis factor receptor-associated periodic syndrome (TRAPS) [10] or deficiency of IL-1 receptor antagonist (DIRA) [11].
The placement of SJIA and AOSD with AID is based primarily on three key observations:
during active disease phases, a significantly increased activation of genes is observed, which either have an amplifying effect on the IL-1 pathway or result in an activation of macrophages or granulocytes [12].
the protein S100A12 as a marker for an activation of macrophages and granulocytes is found significantly increased [13,14].
Drugs that block the IL-1 pathway, or drugs directed against IL-6 or its receptor, are therapeutically successful, whereas therapeutics, such as TNF-alpha inhibitors, that are successful in RA or other forms of JIA are usually insufficiently effective.
Clinical picture & diagnostics
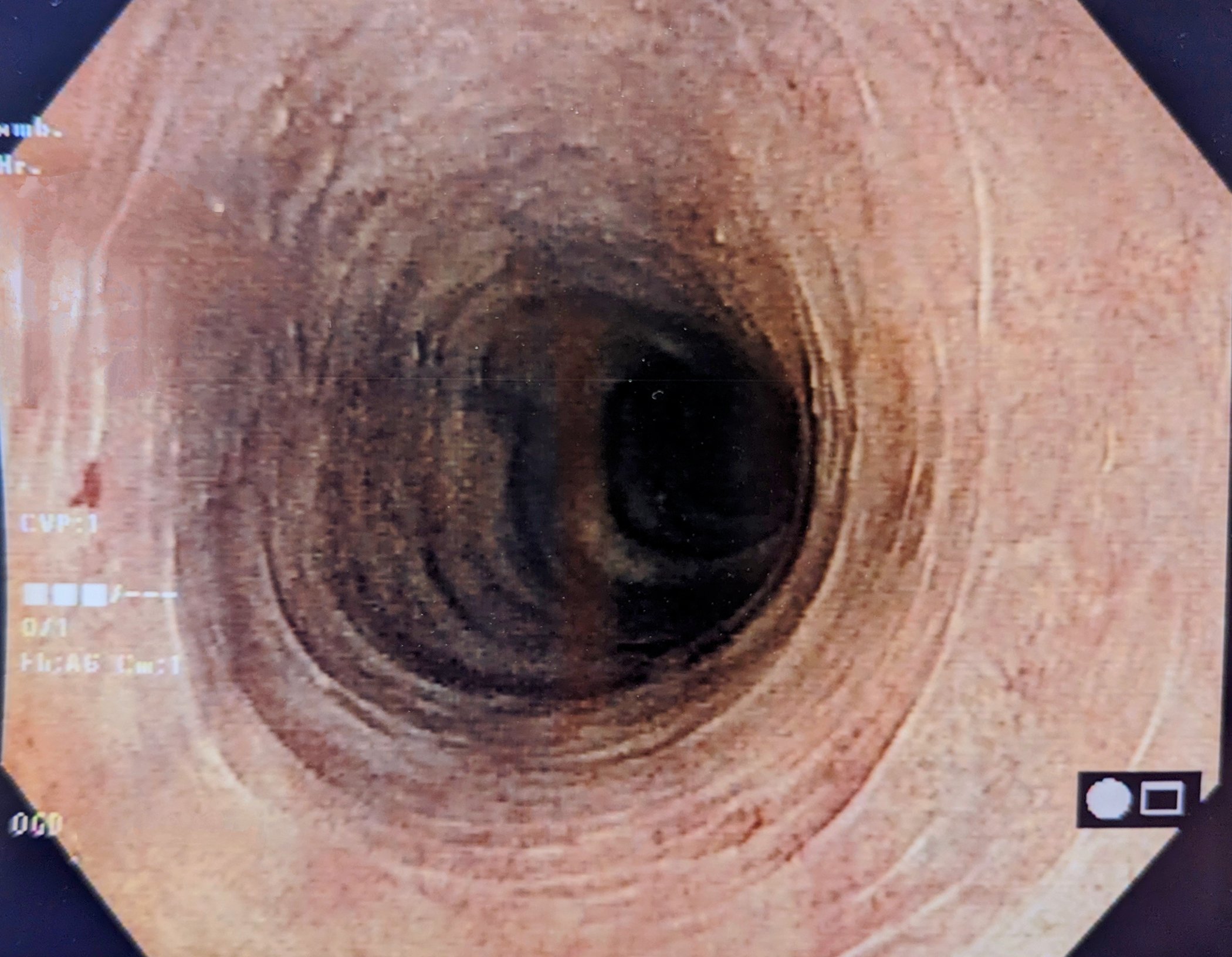
In Germany, epidemiological data are only available for SJIA. According to this, the incidence of JIA is about 16.5/100 000/y. [15], of which approx. 5% are cases with SJIA, which corresponds to a number of approx. 80 new cases annually. The peak age of SJIA is between 2 and 4 years of age [5]. In Japan, SJIA has a much higher proportion of all JIA patients, accounting for approximately 50% of cases [16]. Incidence figures for adult AOSD sufferers are not available for Germany, however, according to data from France and Norway, the incidence compared to SJIA is likely to be significantly lower at 0.16-0.4/100 000/year [17]. Overall, therefore, within the rheumatoid arthritides in children and in adults, these are rather rare disease patterns. Typical features of SJIA and AOSD are the usually simultaneous occurrence of 1. arthralgias or arthritis, 2. intermittent, high (fever spikes, “spiking fever”) and 3. a mostly salmon-colored, volatile exanthema (Fig. 1B). Joint involvement preferentially affects large joints and often has a destructive course if untreated (Fig. 1A). In addition, there is often generalized lymphadenopathy, hepato- and/or splenomegaly (Fig. 1B+D). Especially in cases of high activity of Still’s syndrome, complicating organ manifestations may occur, which in some cases considerably worsen the prognosis: In life-threatening macrophage activation syndrome (MAS), a cytokine storm with consecutive activation of macrophages results in hemophagocytosis of hematopoietic stem cells in the bone marrow with persistent fever and multiple organ failure, incl. Neurological Symptoms [18]. Cardiac involvement usually manifests as pericarditis (Fig. 1C), and less commonly myocarditis, tamponade, or noninfectious endocarditis [19]. Pulmonary involvement in Still’s syndrome can be multifaceted and therefore present problems in differentiating it from infections and interstitial lung disease in particular [20]. Sytemic amyloidosis is rarely observed, usually in association with prolonged, uncontrolled disease activity [3,5,21–24].
Regarding laboratory diagnostics, there are no specific parameters for either SJIA or jSD and AOSD. In contrast to other rheumatologic diseases with arthritis, the anti-nuclear antibodies (ANA) that are frequently positive in JIA are absent, as are the rheumatoid factors (RF) typical of rheumatoid arthritis. This is congruent with the findings on pathogenesis. However, later in the course of the disease, autoantibodies (ANA and IgM-Rf) may also appear in patients with SJIA [25]. In addition to an increase in general inflammatory parameters (ESR, leukocytosis), high initial ferritin levels are observed, especially in AOSD: usually ≥ 5 times the upper normal value. Nevertheless, even at this threshold, the specificity for an AOSD is only around 50% [26], so other causes of hyperferritinemia must be considered for differential diagnosis, especially malignancies and infections [27]. In both children and adults, rapidly increasing or excessively high levels of ferritin should be considered MAS [28]. The protein S100A12, a marker of macrophage and granulocyte activation, is of interest as a laboratory value in two ways. On the one hand, the extremely high levels for this protein indicate the autoinflammatory genesis of all three disease patterns, and on the other hand, this protein seems to be a relevant biomarker for both SJIA, jSD and AOSD [13,14]. In contrast to the situation in children, however, this parameter has so far no consensual value in the diagnosis of the adult form due to insufficient validation [30,31]. Many other biomarkers have been insufficiently validated [13]. Increasingly, however, there are signs that in childhood and adulthood the determination of serum IL-18 may allow a more specific diagnosis of Still’s syndrome, e.g., also in the differentiation from sepsis [29]. However, the availability of the determination is limited in routine care.
The diagnosis of Still’s syndrome is therefore based on a characteristic constellation of symptoms in combination with elevated inflammatory parameters in children according to a consensus recommendation of a group of experts as well as in adults according to the recommendations of the guideline [3,9,30] under the condition that alternative causes are excluded. Important differential diagnoses include infections and malignancies, hereditary autoinflammatory syndromes (more common in childhood), and alternative rheumatologic diseases (Table 1).
Therapy & Prognosis
By the mid-20th century, the mortality of infantile Still’s syndrome was over 40% of cases. Only the introduction of corticosteroids into therapy [30] reduced lethality. Patients with SJIA were also the first pediatric rheumatology cases to receive therapy with methotrexate [31]. The treatment of AOSD was guided by the therapy of SJIA. Separate protocols involving cyclosporin A have been developed for the therapy of MAS [32]. Nevertheless, before the introduction of interleukin-inhibiting therapies, mortality in children and adults with Still’s syndrome exceeded 10%. Then, in the early 2000s, successful therapies were introduced in SJIA using the recombinant IL-1 receptor anatgonist anakinra [33] and the monoclonal antibody tocilizumab [34] directed against the IL-6 receptor. Systemic corticosteroids remain an essential component of therapy during the initial phase. As described above, diagnostic certainty is limited in the initial manifestation of all three diseases due to the lack of specific parameters. Nevertheless, therapy protocols that already initially use the recombinant IL-1 receptor antagonist anakinra to save steroids have become established in recent years [35]. Evidence-based consented treat-to-target therapy protocols from the Society for Childhood and Adolescent Rheumatology (GKJR) are now available for SJIA and childhood Still’s syndrome [3].
For AOSD, systemic glucocorticoids are recommended as acute therapy according to the guidelines. Methotrexate or calcineurin inhibitors (usually cyclosporine A) are suggested for glucocorticoid sparing when disease activity is low, and anakinra, canakinumab, or tocilizumab are suggested with increasing activity or failure of conventional therapies. Anakinra and canakinumab can also be used as first-line therapy in cases of high disease activity. EMA approval in Europe for AOSD currently exists only for anakinra (after glucocorticoid and NSAID failure, alternatively beforehand in moderate to high disease activity) and canakinumab (after glucocorticoid and NSAID failure), but in contrast to the situation with SJIA, not for tocilizumab.
The German Society for Rheumatology (DGRh) published a corresponding S2 guideline [23,24,36]. Generally, a staged approach is recommended in children and adults based on the current clinic, inflammatory laboratory, and comorbidities. The goal of treatment is to achieve remission while using steroid-containing drugs as sparingly as possible.
Differences of juvenile and adult Still syndrome.
By most experts, the juvenile and adult forms of Still’s syndrome are considered to be a disease continuum with different phenoytpic manifestations [30]. This is supported in particular by comparable genetic risk constellations, very similar clinical presentation except for individual domains. and a comparable therapeutic response to interleukin or corresponding receptor blockades, which in turn could indicate the same pathogenesis [37]. However, differences are also known; for example, the sex ratio in SJIA is balanced, whereas in AOSD, two-thirds of the patients are women. Other differences may be explained by a more immature immune system in children compared to adults, e.g., the strong seasonal clustering in the colder months (infectious triggers?) and the clustering of a chronic course (more aggressive disease with earlier onset and severe course?) in the juvenile form [37]. Differences in clinical presentation are also observed; for example, pharyngodynia are so characteristic of a first manifestation in adulthood (approximately 60% of cases) that they have found their way into the Yamaguchi classification criteria, but in childhood they are present in only 10% of cases [38]. In terms of joint involvement (Fig. 2) , the hip and cervical spine are a significant problem in children, accounting for 32% and 24%, respectively, whereas these joints are affected in less than 2% of adults [39]. In SJIA, there is also evidence of an autoimmune event, which seems to become increasingly relevant, at least during the course of the disease. Here, the association with the HLA system [40], the course as polyarthritis with development of autoantibodies [25], the activation of Th1 and Th17 cells and functional deficits of regulatory T cells should be mentioned [41]. Apparently, therefore, the adaptive immune system can be engaged during the course of the disease, which then also brings about changes with regard to the disease-maintaining signaling pathways [42]. The therapeutic consequences have not been adequately investigated at present.
Regarding therapy, major differences between SJIA and AOSD exist in the level of evidence and in the approval situation [23,24]: For example, while RCTs with successful primary endpoints are available for the SJIA-approved options methotrexate, NSAIDs, tocilizumab, anakinra, and canakinumab, the evidence base for adults is limited and approval for AOSD formally exists only for anakinra and canakinumab.
Summary
The infantile forms and the adult have many similarities, but also differences, in addition to the different age of first manifestation. Both SJIA and jSD, as well as AOSD, are fundamentally different in pathogenesis from the other forms of inflammatory arthritis in their respective age groups (JIA and rheumatoid arthritis) and are now understood to be autoinflammatory diseases. If SJIA/jSD is suspected, a pediatric rheumatologist should be consulted early on, and a rheumatologist should be consulted if AOSD is suspected.
Take-Home Messages
- The infantile and adult forms of Still’s syndrome are similar, but not the same.
- Clinical hallmarks are:
Arthralgias/arthritis (affecting mainly “large” joints) and signs of autoinflammation (fever, exanthema) - Children: frequent HSM, adults: strep throat
- Clinical hallmarks are:
- Kinder:
- initial often without arthritis (40%)
- monophasic course in 40% d.F.
- Prevalence depending on ethnicity
- Switch to polyarticular disease without autoinflammation
- Life-threatening courses due to MAS and perimyocarditis are possible.
- Admitted pathogenetically important role of IL-1 (and IL-6) has implications for treatment planning.
Literature:
- Still GF: On a form of joint disease in children. Med Chir Trans 1897;80: 47.
- Petty RE, Southwood TR, Baum J, et al.: Revision of the proposed classification criteria for juvenile idiopathic arthritis: Durban, 1997. J Rheumatol 1998; 25(10): 1991–1994.
- Hinze CH, Holzinger D, Lainka E, et al.: Practice and consensus-based strategies in diagnosing and managing systemic juvenile idiopathic arthritis in Germany. Pediatr Rheumatol Online J 2018; 16(1): 7.
- Bywaters EG: Still’s disease in the adult. Ann Rheum Dis 1971; 30(2): 121–133.
- Lainka E, Haas JP, Horneff G, et al.: Systemic Juvenile Idiopathic Arthritis – New Aspects of Clinical Features, Diagnostic Tools and Treatment Strategies. Ann Paediatr Rheumatol 2013(2): 3–13.
- Kastner DL: Hereditary periodic fever syndromes. Hematology Am Soc Hematol Educ Program 2005: 74–81.
- McDermott MF, Aksentijevich I: The autoinflammatory syndromes. Curr Opin Allergy Clin Immunol 2002; 2(6): 511–516.
- Ozen S: New interest in an old disease: familial Mediterranean fever. Clin Exp Rheumatol 1999; 17(6): 745–749.
- Normand S, Massonnet B, Delwail A, et al.: Specific increase in caspase-1 activity and secretion of IL-1 family cytokines: a putative link between mevalonate kinase deficiency and inflammation. Eur Cytokine Netw 2009; 20(3): 101–107.
- Rosen-Wolff A, Kreth HW, Hofmann S, et al.: Periodic fever (TRAPS) caused by mutations in the TNFalpha receptor 1 (TNFRSF1A) gene of three German patients. Eur J Haematol 2001; 67(2): 105–109.
- Aksentijevich I, Masters SL, Ferguson PJ, et al.: An autoinflammatory disease with deficiency of the interleukin-1-receptor antagonist. N Engl J Med 2009; 360(23): 2426–2437.
- Allantaz F, Chaussabel D, Stichweh D, et al.: Blood leukocyte microarrays to diagnose systemic onset juvenile idiopathic arthritis and follow the response to IL-1 blockade. J Exp Med 2007; 204(9): 2131–2144.
- Bae CB, Suh CH, An JM, et al.: Serum S100A12 may be a useful biomarker of disease activity in adult-onset Still’s disease. J Rheumatol 2014; 41(12): 2403–2408.
- Wittkowski H, Frosch M, Wulffraat N, et al.: S100A12 is a novel molecular marker differentiating systemic-onset juvenile idiopathic arthritis from other causes of fever of unknown origin. Arthritis Rheum 2008; 58(12): 3924–3931.
- Thomschke S, Schulz M, Bätzing J: Epidemiologie der juvenilen idiopathischen Arthritis (JIA) in der ambulanten Versorgung – eine Analyse anhand bundesweiter vertragsärztlicher Abrechnungsdaten der Jahre 2009 bis 2015. Berlin: Zentralinstitut für die kassenärztliche Versorgung in Deutschland (Zi); 2018.
- Fujikawa S, Okuni M: Clinical analysis of 570 cases with juvenile rheumatoid arthritis: results of a nationwide retrospective survey in Japan. Acta Paediatr Jpn 1997; 39(2): 245–249.
- Evensen KJ, Nossent HC: Epidemiology and outcome of adult-onset Still’s disease in Northern Norway. Scand J Rheumatol 2006; 35(1): 48–51.
- Ravelli A, Minoia F, Davi S, et al.: 2016 Classification Criteria for Macrophage Activation Syndrome Complicating Systemic Juvenile Idiopathic Arthritis: A European League Against Rheumatism/American College of Rheumatology/Paediatric Rheumatology International Trials Organisation Collaborative Initiative. Ann Rheum Dis 2016; 75(3): 481–489.
- Bodard Q, Langlois V, Guilpain P, et al.: Cardiac involvement in adult-onset Still’s disease: Manifestations, treatments and outcomes in a retrospective study of 28 patients. J Autoimmun 2021;116: 102541.
- Ruscitti P, Berardicurti O, Iacono D, et al.: Parenchymal lung disease in adult onset Still’s disease: an emergent marker of disease severity-characterisation and predictive factors from Gruppo Italiano di Ricerca in Reumatologia Clinica e Sperimentale (GIRRCS) cohort of patients. Arthritis Res Ther 2020; 22(1): 151.
- Delplanque M, Pouchot J, Ducharme-Benard S, et al.: AA amyloidosis secondary to adult onset Still’s disease: About 19 cases. Semin Arthritis Rheum 2020; 50(1): 156–165.
- Riera E, Olive A, Narvaez J, et al.: Adult onset Still’s disease: review of 41 cases. Clin Exp Rheumatol. 2011; 29(2): 331–336.
- Vordenbaumen S, Feist E, Rech J, et al.: [DGRh S2e guidelines : Diagnostic and treatment of adult-onset Still’s disease (AOSD)]. Z Rheumatol 2022; 81(Suppl 1): 1–20.
- Vordenbaumen S, Feist E, Rech J, et al.: [Guideline report on the DGRh S2e guidelines on diagnostics and treatment of adult-onset Still’s disease (AOSD)]. Z Rheumatol 2022; 81(Suppl 1): 21–27.
- Hugle B, Hinze C, Lainka E, et al.: Development of positive antinuclear antibodies and rheumatoid factor in systemic juvenile idiopathic arthritis points toward an autoimmune phenotype later in the disease course. Pediatr Rheumatol Online J 2014; 12: 28.
- Bilgin E, Hayran M, Erden A, et al.: Proposal for a simple algorithm to differentiate adult-onset Still’s disease with other fever of unknown origin causes: a longitudinal prospective study. Clin Rheumatol 2019; 38(6): 1699–1706.
- Moore C Jr, Ormseth M, Fuchs H: Causes and significance of markedly elevated serum ferritin levels in an academic medical center. J Clin Rheumatol 2013; 19(6): 324–328.
- Kostik MM, Dubko MF, Masalova VV, et al.: Identification of the best cutoff points and clinical signs specific for early recognition of macrophage activation syndrome in active systemic juvenile idiopathic arthritis. Semin Arthritis Rheum 2015; 44(4): 417–422.
- Takakura M, Shimizu M, Yakoyama T, et al.: Transient natural killer cell dysfunction associated with interleukin-18 overproduction in systemic juvenile idiopathic arthritis. Pediatr Int 2018; 60(10): 984–985.
- Debre R, Thieffry S, Mozziconacci P, et al.: [Still’s disease treated by ACTH and cortisone; 6 cases]. Arch Fr Pediatr 1951; 8(8): 668–671.
- Kolle G: [Current treatment of juvenile rheumatoid arthritis (juvenile chronic polyarthritis) and Still’s syndrome]. Monatsschr Kinderheilkd 1968; 116(10): 529–534.
- Mouy R, Stephan JL, Pillet P, et al.: Efficacy of cyclosporine A in the treatment of macrophage activation syndrome in juvenile arthritis: report of five cases. J Pediatr 1996; 129(5): 750–754.
- Verbsky JW, White AJ: Effective use of the recombinant interleukin 1 receptor antagonist anakinra in therapy resistant systemic onset juvenile rheumatoid arthritis. J Rheumatol 2004; 31(10): 2071–2075.
- Yokota S: Interleukin 6 as a therapeutic target in systemic-onset juvenile idiopathic arthritis. Curr Opin Rheumatol 2003; 15(5): 581–586.
- Vastert SJ, de Jager W, Noordman BJ, et al.: Effectiveness of first-line treatment with recombinant interleukin-1 receptor antagonist in steroid-naive patients with new-onset systemic juvenile idiopathic arthritis: results of a prospective cohort study. Arthritis Rheumatol 2014; 66(4): 1034–1043.
- Vordenbaumen S, Feist E, Rech J, et al.: Erratum to: Diagnosis and treatment of adult-onset Still’s disease: a concise summary of the German society of rheumatology S2 guideline. Z Rheumatol 2023; 82(Suppl 2): 93–94.
- Jamilloux Y, Gerfaud-Valentin M, Martinon F, et al.: Pathogenesis of adult-onset Still’s disease: new insights from the juvenile counterpart. Immunol Res 2015;61(1–2): 53–62.
- Ruscitti P, Natoli V, Consolaro A, et al.: Disparities in the prevalence of clinical features between systemic juvenile idiopathic arthritis and adult-onset Still’s disease. Rheumatology (Oxford) 2022; 61(10): 4124–4129.
- Pay S, Turkcapar N, Kalyoncu M, et al.: A multicenter study of patients with adult-onset Still’s disease compared with systemic juvenile idiopathic arthritis. Clin Rheumatol 2006; 25(5): 639–644.
- Ombrello MJ, Remmers EF, Tachmazidou I, et al.: HLA-DRB1*11 and variants of the MHC class II locus are strong risk factors for systemic juvenile idiopathic arthritis. Proc Natl Acad Sci USA 2015; 112(52): 15970–15975.
- Feist E, Mitrovic S, Fautrel B: Mechanisms, biomarkers and targets for adult-onset Still’s disease. Nat Rev Rheumatol 2018; 14(10): 603–618.
- Nigrovic PA: Review: is there a window of opportunity for treatment of systemic juvenile idiopathic arthritis? Arthritis Rheumatol 2014; 66(6): 1405–1413.
- Tsai HY, Lee JH, Yu HH, et al.: Initial manifestations and clinical course of systemic onset juvenile idiopathic arthritis: a ten-year retrospective study. J Formos Med Assoc 2012; 111(10): 542–549.
HAUSARZT PRAXIS 2023; 18(7): 10–14