Inertia with regard to therapy adjustment is called therapeutic “inertia” in the literature and is one reason why treatment goals are not fully achieved in the disease management of a chronic disease. So far, there is hardly any data on this in the field of psoriasis. A team of researchers from France has now recently conducted a study, published in JEADV in 2020, that looks at the issue from different angles.
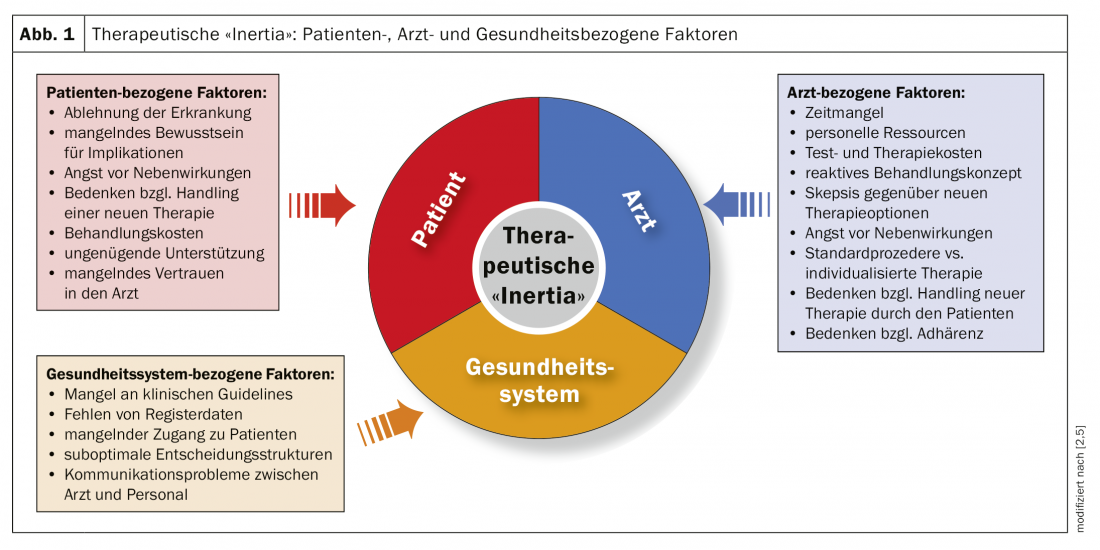
Since the concept of therapeutic “inertia” by Phillips et al. [1] was described in relation to disease management of chronic diseases in 2001, more than 1000 scientific articles have been published on this in the field of blood pressure, diabetes, cardiovascular diseases and osteoporosis [2,3]. During the EADV Congress in Madrid, Dr. Bruno Halioua, Dermatology Department of the Alfred Fournier Institute, Paris, presented on the first study conducted in France on this topic in relation to psoriasis [2]. In view of the constantly expanding spectrum of therapy options, the question of a treatment regimen optimally adapted to individual patient characteristics and thus also the topic of therapy adaptation is very topical. What are the explanations for therapeutic “inertia”? Several factors are cited as causes, including overestimation of current treatment, lack of training, and organizational barriers. In the context of disease management in diabetes, where there are numerous empirical findings on this phenomenon, the reasons were divided into patient-, physician-, and health system-related aspects (Fig. 1).
Observational study yields interesting results
In the study conducted by Halioua et al. conducted was a questionnaire study in the period from January to June 2019 [2,4]. Patients were recruited through the Carenity Platform and completed online surveys. The objectives of the study: to elicit causes of therapeutic “inertia” from the patient’s perspective; to evaluate consequences; and to identify ways to solve the problem. 181 subjects participated in the study, the mean age was 51.3 years (SD 14.4), and the mean time since diagnosis was 15.7 years (SD 13.9). 30.4% of the subjects were female, 69.6% male. Topical treatment was received by 46% at the time of the survey, and conventional systemic therapy (methotrexate, acitretin, apremilast) was used in 31%. Treatment with biologics was 20% and about 6% received phototherapy as monotherapy/or concomitant therapy. Treatment was coordinated by a dermatologist in 62%, by a general practitioner in 30%, and the remainder were managed by rheumatologists or other specialists. Among those receiving biologic treatment, the proportion of patients managed by dermatologists was 81%; for conventional systemic treatment (methotrexate, acitretin, apremilast), 77%; and for topical therapy, 44%.
Reflect on “treat to target” on a case-by-case basis
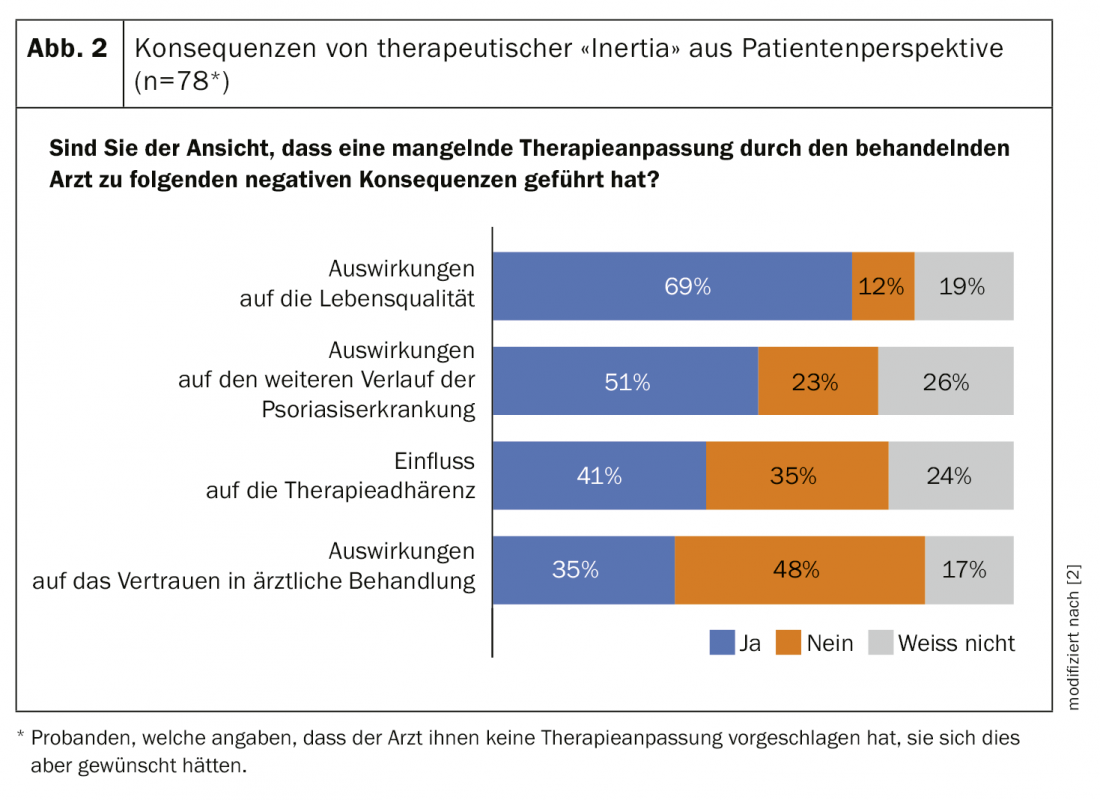
In 51% of the respondents, there has been an adjustment in therapy in the course to date, half of whom believe that their physician should have modified treatment earlier. 41% switched from topical to oral treatment, and 31% switched from oral to subcutaneous therapy. Among patients to whom the physician had not suggested a treatment modification, 68% indicated that they would like the physician to suggest a treatment modification. The speaker emphasizes that this is a surprisingly high percentage. Among the suspected reasons why the treating physician does not offer oral or subcutaneous therapy to topically treated patients, the study participants indicated the following: Underestimation of the extent of impairment due to psoriatic disease, resistance to innovative therapies, lack of time, therapy adjustment is not given sufficient relevance, physician does not feel competent enough to prescribe oral or subcutaneous therapy options. For 69% of those who have not yet had their therapy adjusted, the lack of treatment modification has an impact on quality of life, and 51% believe that it affects the course of psoriasis (Fig. 2).
Therapy decision influences adherence
To overcome therapeutic “inertia”, it is important to correctly grasp the complexity of “treat to target” in a specific case and to organize routine clinical procedures in a way that facilitates the implementation of appropriate measures [1]. 71% of all study participants (128 of 181) had a change of physician. Reasons given were: for 42%, switching to another doctor was independent of treatment, 41% felt the doctor was not prescribing the best possible treatment, 29% felt the doctor was not involved enough, 16% found the explanations of treatment decisions insufficient; for the rest, other reasons were decisive. Resistance to therapy is a complex issue. When asked how they would respond if they felt the physician was not prescribing the best possible therapy, 14% of patients said they would discontinue treatment and 9% said they would not follow through consistently. Overall, this corresponds to a proportion of 23% for which non-adherence would be a likely consequence with the possible consequence of a worsening of the condition, the speaker emphasizes. The study by Haliou et al. [2,4] shows that therapeutic “inertia” has implications for the treatment and course of psoriatic disease and that adequate attention to this complex problem can contribute to improved treatment outcomes and patient satisfaction.
Literature:
- Phillips LS, et al: Clinical inertia. Ann Intern Med 2001; 135: 825-834.
- Halioua B: Perception of therapeutic inertia by patients with psoriasis in France. Bruno Haliou, MD, Free communications, EADV Congress, Madrid, Oct. 10, 2019.
- Khunti K, et al: Therapeutic inertia in the treatment of hyperglycaemia in patients with type 2 diabetes: A systematic review. Diabetes Obes Metab 2018; 20: 427-437.
- Halioua B, et al: Therapeutic inertia in the management of moderate-to-severe plaque psoriasis. J Eur Acad Dermatol Venereol 2020; 34(1):e30-e32. doi: 10.1111/jdv.15882.
- Allen JD, Curtiss FR, Fairman KA: Nonadherence, clinical inertia, or therapeutic inertia? J Manag Care Pharm 2009; 15(8): 690-695.
DERMATOLOGY PRACTICE 2020; 30(2): 22-24











