In renal healthy individuals, adequate drinking may reduce the risk of renal dysfunction. In chronic renal failure, the effects of fluid intake depend, among other things, on the stage of the disease. Salt consumption also plays an important role.
The prevalence of chronic renal impairment is higher in older individuals. Swiss dietary recommendations for older adults indicate that drinking may often be reduced due to a decreased sense of thirst in old age [1]. The German Society for Nutrition recommends at least 1.5 to 2.5 liters of fluid per day as a rough guideline, whereby the individual fluid requirement varies depending on the state of health and physical activity as well as other factors [2]. Analyses of drinking behavior should also take into account the amount of fluid excreted in urine or via sweat secretion, as well as salt intake, explained Prof. Peter Mertens, MD, Magdeburg (D) [3].
Influence of drinking behavior in normal renal function.
Empirical evidence suggests that drinking plenty of fluids is beneficial in renal health because it suppresses the secretion of antidiuretic hormone (ADH). According to data from two cross-sectional studies in the general population (n=2744, n=2476), the incidence of kidney disease was reduced by 50% with daily drinking of 3.2 l/day vs. 1.8 l/day (OR 0.50; 95% CI 0.32-0.77). Beverage consumption was surveyed by questionnaire, and the respondents were >50 years old. The authors concluded that higher fluid intake is a protective factor with respect to chronic kidney disease [4]. That it is not irrelevant which beverages are consumed regularly is shown by data published in 2019 from a prospective study (n=3003) in the USA. Accordingly, the risk of chronic kidney disease is increased by 61% with regular consumption of sugary beverages over a long period of time (OR 1.61; 95% CI 1.07-2.41). Overall, 6% developed chronic kidney disease during a median follow-up period of eight years. Beverage consumption was assessed by questionnaire, and the mean age at baseline was 54 years. To eliminate confounding factors, stratification was performed with respect to eGFR at baseline, demographic factors, lifestyle factors, and other aspects. Subsequent evaluation using regression analysis and PCA (“Principal Component Analysis”) revealed the following: The risk of chronic kidney disease was 61% higher with higher consumption of sugary beverages (OR 1.61; 95% CI 1.07-2.41). New-onset chronic kidney disease was defined as the following constellation: eGFR <60 ml/min per 1.73 m2 and ≥30% eGFR decline compared with baseline values (eGFR ≥60 ml/min per 1.73 m2). The authors concluded that further studies are needed to find out more about the relationship between drinking patterns/type of beverages and risk of chronic kidney disease as a basis for appropriate dietary recommendations [5].
Kidney disease: salt consumption should be reduced
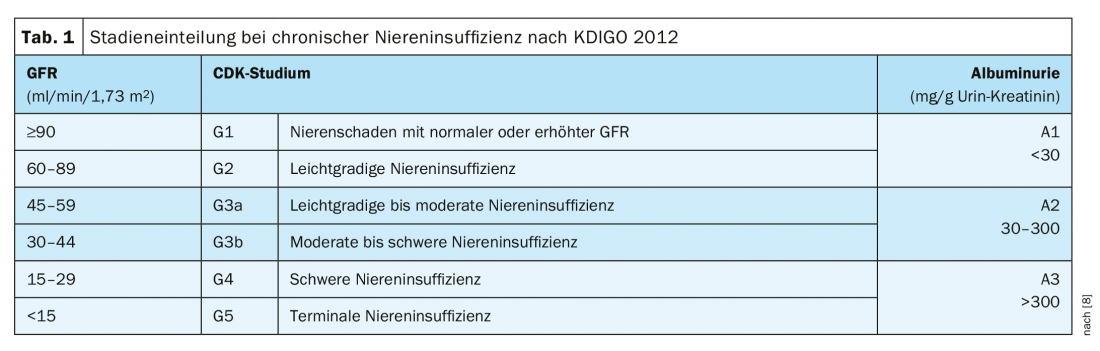
In chronic renal failure, the kidneys are permanently damaged. As a result, the tissue gradually perishes, so that the function of the kidneys continues to decline.This can be caused by congenital or acquired kidney diseases and diabetes. Due to the decreasing activity of the kidneys, various disturbances occur in the organism. For example, uremic substances such as urea, uric acid or creatinine accumulate in the blood and are toxic in higher concentrations. Normally, these substances are excreted through the kidneys in the urine. The decrease in kidney tissue also leads to disturbances in the water, electrolyte and hormone balance. The consequences are anemia, hypertension and increased bone loss (renal osteopathy). Estimated glomerular filtration rate (eGFR) is considered a parameter for clinical assessment of the extent of renal dysfunction (Table 1). In patients with chronic kidney disease in predialysis stages, increased water consumption is associated with better renal function in various observational studies [6]. In contrast, a randomized trial published in JAMA in 2018 in patients with stage 3 CKD (GFR 60-30 ml/min/1.73 m2) did not demonstrate a benefit to increased water intake. Patients in one group (n=316) were instructed to drink more water, and the control group (n=315) was to maintain their previous fluid intake. That the verum group had actually drunk more fluid was evident from the higher 24-hour urine volumes, which were 0.6 l higher than in the control group. The mean change in GFR was -2.2 ml/min/1.73m2 in the group that increased fluid intake and -1.9 ml/min/1.73m2 in the control group. This difference was not significant. It is possible that the result was not independent of the test methodology, according to the authors [7].
In addition to adequate drinking, limiting salt intake is also something very important, he said. Quantification of salt intake was best done by collecting urine over 24 h, he said. Based on this, one can calculate the amount of sodium absorbed. The fact that a high daily salt intake is a possible risk factor for the development of hypertension and cardiovascular disease has been discussed for some time [9]. Regarding chronic kidney disease, it was empirically demonstrated that over a 48-month period, the correlation with dialysis dependency was lowest at a salt intake of <6 g/day, no large differences were measurable at 6-12 g/day, but at a daily salt intake of >12g, the risk for dialysis dependency increased significantly [10].
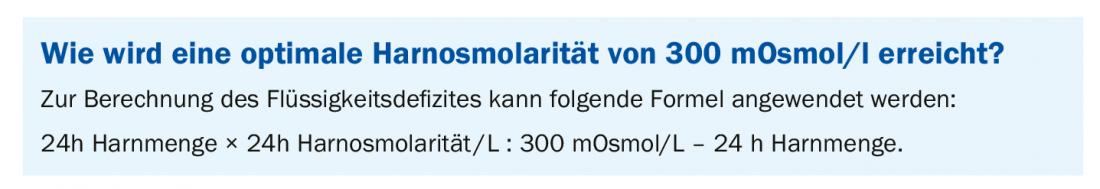
That urinary osmolarity is associated with increased dialysis requirement is shown by a retrospective cohort analysis (n=273) in patients with chronic kidney disease (stage 1-4) by Plischke et al. 105 patients required dialysis during the follow-up period (92 months). After statistically factoring out demographic and other factors (e.g., creatinine clearance and diuretics), higher urine osmolarity was found to be a risk factor for dialysis dependency. The optimal urine osmolarity can be calculated using a formula (box).
Literature:
- Swiss Society for Nutrition (SGE): Nutrition Recommendations for Older Adults, www.sge-ssn.ch/media/Ernährungsempfehlungen_d_def.pdf
- German Nutrition Society (DGE): Water, dge.de/science/reference-values/water/
- Mertens P: Myths in nephrology. Slide presentation Prof. Dr. med. Peter Mertens, Magdeburg (D). Tutorial/Expert Forum, DGIM May 5, 2019.
- Strippoli GF, et al: Fluid and nutrient intake and risk of chronic kidney disease. Nephrology (Carlton) 2011; 16(3): 326-334.
- Rebholz CM, et al: Patterns of Beverages Consumed and Risk of Incident Kidney Disease. CJASN 2019; 14(1): 49-56.
- DGFN www.dgfn.eu/wissenschaftsnews-details/hoehere-trinkmenge-zum-schutz-der-nierenfunktion.html
- Clark WF, et al: Effect of Coaching to Increase Water Intake on Kidney Function Decline in Adults With Chronic Kidney Disease: The CKD WIT Randomized Clinical Trial. JAMA 2018; 319(18): 1870-1879.
- KDIGO: Guidelines 2012, https://kdigo.org/
- Federal Agency for Food and Agriculture (BMEL): Results of the DEGS Study, www.bmel.de/SharedDocs/Downloads/Ernaehrung/Ergebnisse%20DEGS-Salzaufnahme.pdf;jsessionid=2E2E861F98424D603B373C4C17896386.2_cid376?__blob=publicationFile
- Vegher S, et al: Sodium Intake, ACE Inhibition and Progression to ESRD. J Am Soc Nephrol 2012; 23(1): 165-173.
- Plischke M, et al.: Urine osmolarity and risk of dialysis initiation in a chronic kidney disease cohort – a possible titration target? PLoS One 2014; 9(3): e93226.
FAMILY PRACTICE 2019; 14(12): 38-39











