HAUSARZT PRAXIS met with PD Dr. med. Sibil Tschudin, Head Physician of the Department of Gynecological Social Medicine and Psychosomatics in Basel. The renowned expert in the field of contraception provided information on the safety of natural contraceptive methods, the dangers of the combined pill and the effectiveness of progestogen monopreparations (mini-pill).
Dr. Tschudin, there are so-called “natural” methods of contraception such as coitus interruptus or orientation to the female menstrual cycle. Numerous methods (temperature, hormone measurement, calendar) promise to predict the time of ovulation. Provided they are carried out in a disciplined manner: How safe are these natural types of contraception?
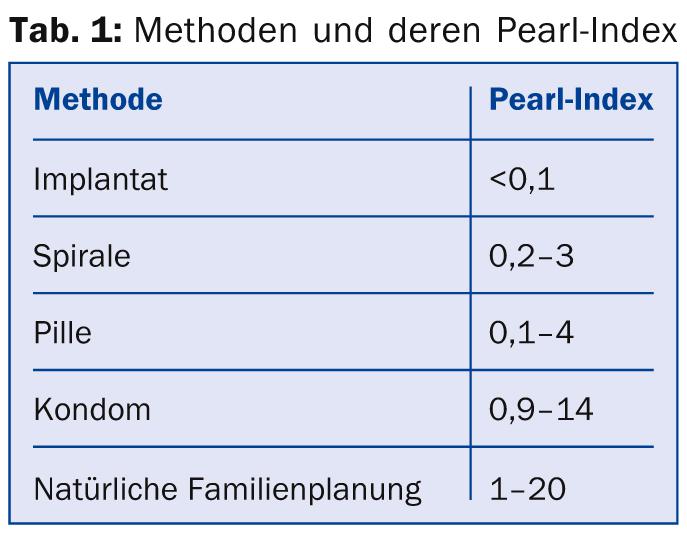
Dr. Tschudin: The safety or efficiency of a contraceptive is indicated by the Pearl index (number of pregnancies per 100 women using the method for one year). It is tested with clinical studies (Phase III studies) before market launch and according to the study results the Pearl index is calculated. In Table 1 I have summarized some methods in a listing resp. comparison.
This shows that with great application discipline, the natural methods may well be successful over a period of time. But they are very prone to error and do not take into account that nature does not always function like clockwork, nor is discipline always at the forefront of sexuality.
Hormonal contraception and its risks regularly reach the media spotlight and are the subject of controversial discussions. With regard to the progestogens contained in combined pills, a distinction is made between different generations. Which progestins are mainly suspected to increase thromboembolic risk?
The available study results indicate that the risk is somewhat higher with third-generation progestins (desogestrel, gestodene) than with second-generation progestin levonorgestrel. However, it is important to keep in mind that with an overall low risk of thrombosis for young healthy women, this increase is only minor. Other factors play a larger role. In any case, the factors age, nicotine consumption, weight and BMI as well as blood pressure and of course the cardiovascular family history have to be included in the clarification and decision.
The risk of thrombosis is also somewhat higher with the anti-androgenic progestins, which are used primarily in women with acne. The Swiss Society of Gynecology and Obstetrics (SGGG) points out that ovulation inhibitors with cyproterone acetate in particular have a slightly higher thromboembolic risk than those with second-generation progestins. Therefore, according to SGGG, the sole desire for contraception without androgenization symptoms is not an indication for a preparation containing cyproterone acetate. Crucially, however, the ethinyl estradiol is responsible for the increased risk of thrombosis, and the progestin combined with it merely has an additional influence.
So when are these preparations contraindicated, and when are they still used?
The preparations are contraindicated if a woman is at above-average risk of thrombosis. To determine this, a careful self and family history is actually the most important thing.
Aside from cyproterone acetate, what is there to say about the other fourth-generation progestins?
Basically, the same applies to the other fourth-generation progestins. However, the risk increase appears to be most pronounced with cyproterone acetate. However, and this is crucial as mentioned, the combined pill with cyproterone acetate also contains a specially high dose of ethinyl estradiol (35 µg).
According to the latest research findings, are progestogen monopreparations (i.e. mini-pills) equally effective as combined pills?
The only progestogen monopreparation of which this can be said is Cerazette®. It is dosed in such a way that it has an ovulation-inhibiting effect.
Most pills contain lactose. Which hormonal contraceptives are independent of gastrointestinal absorption and provide good contraceptive protection?
The lactose thing is actually a problem. In the case of lactose intolerance, hormonal contraceptives include the combination vaginal ring (NuvaRing®) and patch (Evra®) on the one hand, and monopreparations such as the rod (Implanon®) and the three-month injection on the other.
Interview: Andreas Grossmann
HAUSARZT PRAXIS 2014; 9(2): 4











