In Germany, the number of skin cancer cases has been increasing for many years. The incidence is currently over 200,000 per year, including approximately 20,000 malignant melanomas. The number of new cases is expected to double further by 2030. In parallel with the number of cases, melanoma mortality continued to rise, despite the introduction of nationwide skin cancer screening as early as 2008. However, the screening program should not be abolished for lack of benefit, but it should be improved.
“Nobody wants to abolish skin cancer screening in Germany,” Professor Claus Garbe, MD, from Tübingen, emphasized at FOBI 2016 in Munich. However, the experts naturally expected more from the precautionary program. Everyone over the age of 35 has been able to be screened for skin cancer free of charge every two years since 2008. In Switzerland, skin cancer screening based on the German model was established in mid-2014.
Participation rate far too low
“The goal, of course, remains to reduce skin cancer mortality,” Garbe said. The fact that this has not yet been achieved has been a source of debate for years. According to the dermatologist, the debate about the sense or nonsense of skin cancer screening has now died down. There are explanations for the lack of benefit and starting points for improvement. A main problem is and remains the far too low participation rate. According to a Forsa survey of around 1,000 people with statutory health insurance in 2013, only about half are aware of their entitlement to statutory skin cancer screening and only 35% have ever taken part. Those who did, preferred the dermatologist and were mostly satisfied with the preventive care.
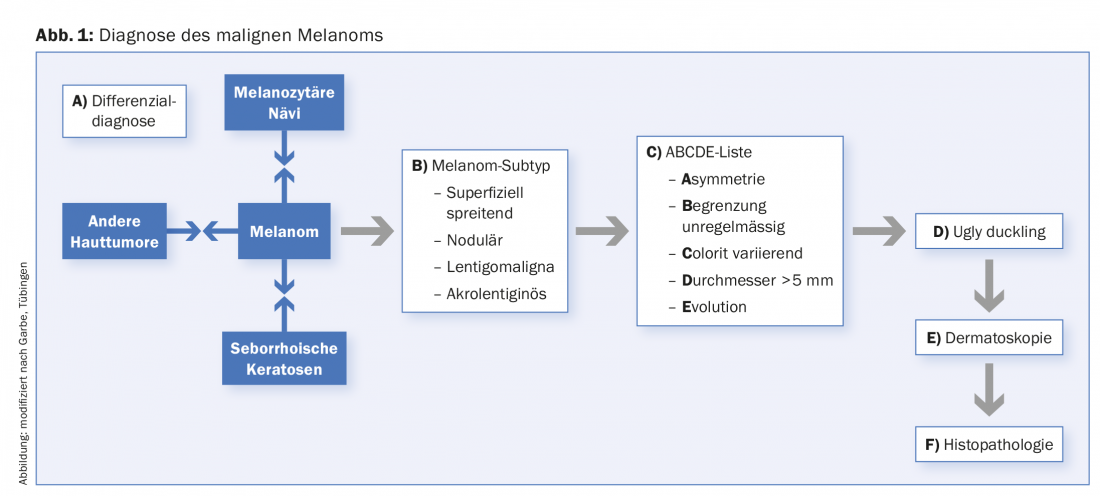
Diagnostic accuracy needs to be improved in skin cancer screening, Garbe said. Currently under discussion is the expansion to 2-step screening in dermatological and non-dermatological practices based on good qualification of general practitioners and inclusion of other specialist groups such as gynecologists, urologists and surgeons. Dermatologists should give preference to high-risk individuals and those with suspected skin cancer during full-body inspections in non-dermatology offices. Dermatologists should offer dermoscopy to diagnose pigmented skin lesions, CT dermoscopy for high-risk individuals, and be specially trained in this area. Of course, this also requires adequate remuneration for this investigation, Garbe said.
Explosion of occupational squamous cell carcinoma.
Work-related UV exposure is often underestimated as a risk factor for skin cancer. People who work outdoors have about three times the risk of epithelial skin tumors than office workers, according to a European case-control study [1], reported Professor Dr. Swen Malte John, dermatologist and preventive physician from Osnabrück.
In Germany, squamous cell carcinomas of the skin caused by natural UV radiation or multiple actinic keratoses and their precursors were added to the list of occupational diseases at the beginning of 2015. According to the medical expert advisory board, approximately 5% of the findings – about 20,000 cases per year in Germany – are work-related. In contrast, the experts did not see any correlation between basal cell carcinomas and malignant malignancies with work-related UV exposure.
When the new occupational disease went into effect, the number of reported cases exploded, John said – from about 550 cases annually from 2005 to 2011 to 6800 cases in 2013. About a quarter of them were (provisionally) recognized as occupational diseases. In Switzerland, the recognition rate for occupational diseases is generally much higher. According to the statutory accident insurance company Suva, the rate is 80% and is the second highest in Europe. A claim for occupational skin cancer is also possible, no distinction is made according to the type of skin tumor.
Skin cancer report with listing of years of radiation exposure required
The difficulty, especially in the case of skin cancer due to natural UV exposure, is to prove that the UV exposure occurred predominantly during occupational activities. Known risk groups with particularly high exposure include road construction workers, letter carriers (with bicycles), and roofers. In individual cases, John said, the report of an occupational skin cancer should include photographic documentation of the skin findings and information about the occupation, if possible, as well as a listing of UV exposure by years of outdoor work and average additional radiation exposure. According to estimates for road construction workers in Bavaria, the average UV exposure in a work week in May (5 days) is about 32 standard erythrocyte doses (SED) and over 600 SED per year. For comparison, UV exposure in the general German population averages 2.5 SEDs/week and about 130 SEDs per year. According to John, UV exposure of outdoor workers in our latitudes is highest in April and May because work is done primarily during midday hours.
The skin cancer report for reporting an occupational disease is currently remunerated in Germany with 30 euros, the annual follow-up report with 50 euros. In addition, the German healthcare system has recently introduced new billing codes in professional dermato-oncology, for example for photodynamic therapy (PDT).
Will daylight PDT become the new standard?
PDT is among the most efficient therapies for actinic keratinosis (AK). Daylight PDT is currently establishing itself as an alternative to classic red light PDT. Among the major advantages of the new procedure are the significantly lower pain intensity with the same effectiveness as the standard and the significantly lower time burden on the practice, reported Professor Dr. Rolf-Markus Szeimies from Recklinghausen. The main disadvantage is that the procedure can be used only in the months of April to October, when the outside temperature is higher than 10 degrees Celsius. The light intensity must be at least 2300 lux and it must not rain during the two-hour sun exposure.
How does a sunlight PDT work?
Sunscreen is applied first, and 15 minutes later, as in red light PDT, the keratotic lesions are roughened and methyl aminolevulinate (MAL) is applied to sensitize the skin. However, occlusion of the sensitizer, as in red light PDT, is not required; two-hour daylight exposure can be started within 30 minutes, Szeimies reported. After exposure, the ointment residues are washed off, ready. Attention should be paid to 24-hour light protection. In daylight PDT, the patient spends only one hour in the office (total procedure: 3 hours); in standard PDT, the entire procedure takes 4 hours.
Treatment success at 3 months is similar: in studies in Australia in patients with predominantly AK-1 lesions and facial AK, approximately 90 percent of lesions healed completely. In European studies with a higher proportion of AK-2 and scalp lesions, cure rates were 70 to 74 percent.
In the pivotal studies, daylight PDT was nearly painless, Szeimies reported, whereas with red-light PDT, pain intensity is usually reported as VAS 4-6. The reason: During daylight PDT, toxic protoporphyrin IX is continuously produced in the skin cells, so that it remains in the cell; during red-light PDT, on the other hand, the concentration of protoporphyrin IX increases more strongly, it is transported out of the cell, which causes the pain, according to Szeimies.
Even in winter, daylight PDT can be simulated using powerful lamps, the dermatologist said. Other variations are being tested, such as the greenhouse PDT, which does not require UV protection. In addition, a MAL cream exclusively for daylight PDT of AK-1 and -2, which patients can apply themselves, has recently been approved. This further reduces the time required for patients in the office.
Source: Plenary session “Dermatooncology II: Non-melanocytic skin tumors”, Munich, July 27, 2016, during the 25th Continuing Education Week (FOBI) for Practical Dermatology and Venereology.
Literature:
- Trakatelli M et al: EADV 2016; 30(Suppl 3): 5-11.
DERMATOLOGIE PRAXIS 2016; 26(6): 34-36