The pathogenesis of psoriasis is complex, but is becoming increasingly better understood. With the modern substance classes of interleukin (IL)-17 and IL-23 inhibitors, highly effective biologics are now available for the treatment of psoriasis. In addition to the fastest possible improvement of the condition under treatment, disease-modifying effects, which ideally continue even after discontinuation of biologic
therapy, are also increasingly the focus of research interest.
Psoriasis is considered a T cell-mediated disease in which CD8+ and CD4+ T cells recognize autoantigens and trigger an inflammatory cascade. This results in the production of pro-inflammatory cytokines such as IL(interleukin)-17 and IL-23, which leads to the proliferation of keratinocytes. It is becoming increasingly clear that the patterns of inflammatory mediators and cells are dynamic during the course of the disease. Biologics selectively inhibit individual components of the misdirected inflammatory response in psoriasis and have a favorable risk-benefit profile. This applies in particular to the modern substance classes of IL-17 and IL-23 inhibitors [1]. In order to influence the progression of the disease in the long term and in the best possible way, it is advisable not to miss a “window of opportunity”. The earlier biologic therapy is started, the greater the chance that its effectiveness will be maintained for a long time, explained Prof. Dr. med. Curdin Conrad, Head Physician at the Department of Dermatology and Venereology, CHUV, Lausanne [2].
TRM cells and epigenetic changes are central
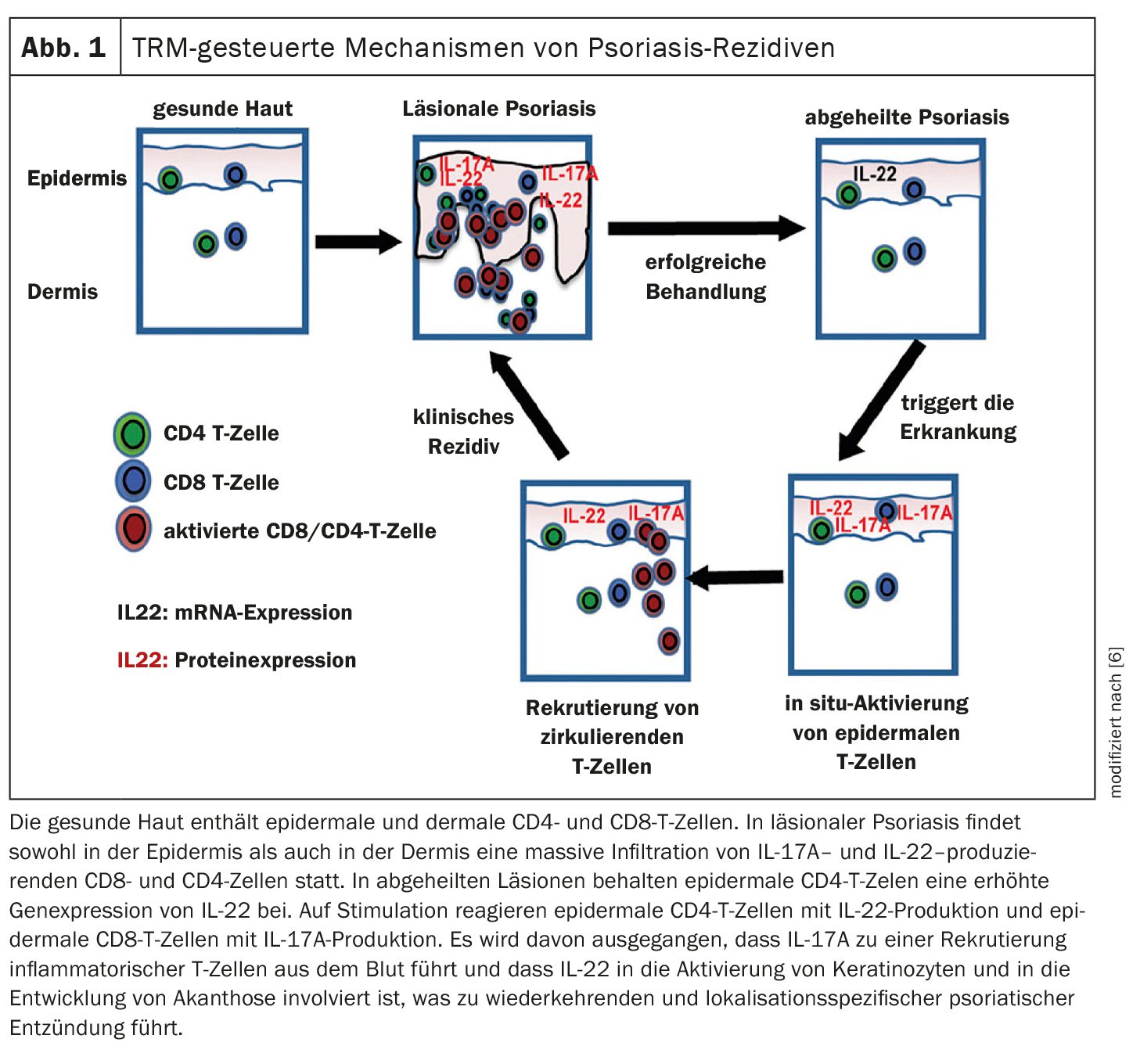
Clinical and experimental evidence suggests that immunological regulation, for example by tissue resident memory T-cells (TRM cells), and epithelial “memory functions” play a central role in the initiation, course and severity of psoriasis [1]. TRM cells are components of the adaptive immune system that remain in the skin and do not circulate through the body like effector T cells. TRM cells are thought to be significantly involved in the development of recurrences in sites where psoriatic lesions had initially healed and it has been shown that patients with longer duration of psoriasis had more TRM cells in the skin compared to those with shorter duration of disease [3]. TRM cells are found in the skin, intestinal tract, lungs, liver and other tissues. In psoriasis research, TRM cells are increasingly becoming the focus of interest with regard to targeting long-lasting relapse-free phases or sustainable healing [7]. “Early intervention may be able to reduce the risk of TRM cells accumulating in the skin,” explained Prof. Conrad [2]. In addition to TRM cells, other cell types are also involved in inflammatory memory. These include, for example, epidermal keratinocytes, which can be altered by epigenetic influences (e.g. DNA methylation and histone modification) [1].
“Windows of opportunity” for biologics is underpinned by studies
Various recent studies indicate that biologics are more effective in psoriasis the earlier they are used in the course of the disease, explained the speaker [2].
- In an extension phase of the ERASURE/FIXTURE studies, the psoriasis relapse rates after discontinuation of secukinumab were determined [4]. After the last dose of secukinumab (300 mg), 20.8% (25/120) and 10.0% (12/120) of patients who had been switched to placebo remained relapse-free for 1 and 2 years respectively. It was found that the duration and severity of psoriasis were significantly associated with the time to relapse (p=0.02 in each case). Patients with a shorter disease duration and lower PASI values at baseline remained relapse-free for longer [4].
- The STEPIn study also showed that early intervention with secukinumab was associated with high and sustained healing rates [5]. The study included biologics-naïve patients with psoriasis lasting <1 year. Over 90% of participants achieved a PASI90 response at week 52 when treated with secukinumab. Light therapy (NB-UVB) served as the comparator arm [5].
- In the GUIDE study, guselkumab therapy achieved better response rates in psoriasis patients with a disease duration ≤2 years than in those with longer-standing psoriasis (51.8% and 39.4% respectively had an absolute PASI score= 0 at week 28) [8].
In summary, these and other study data indicate that early intervention with biologics should be targeted in order to achieve the best possible disease-modifying effects and a sustained clinical response, Prof. Conrad summarized, explaining that the likelihood of reversing epigenetic changes is higher if biologic treatment is started earlier after the initial manifestation of psoriasis [2]. According to Cheuk et al., future therapeutic strategies for psoriasis could have a two-phase structure [6]: in a first phase, signaling molecules such as interleukins and TNF-α are inhibited, which are known to be involved in the chronification of inflammatory processes, and in a next step, TRM cells of earlier psoriasis localizations could be targeted. As an alternative to systemically administered antibodies, topical eradication of TRM cells could also prove to be a possible strategy to prevent psoriasis relapse, according to the authors [6].
Congress: EADV Annual Meeting
Literature:
- Schön MP, Wilsmann-Theis D: Current developments and perspectives in psoriasis. JDDG 2023; 21(4): 363-373.
- “The headline news – Psoriasis”, Prof. Dr. Curdin Conrad, Skin Inflammation & Psoriasis International Network, EADV Annual Meeting, Amsterdam, 25.09.2024.
- Blauvelt A: Resident Memory T Cells in Psoriasis: Key to a Cure? J Psoriasis Psoriatic Arthritis 2022; 7(4): 157-159.
- Lebwohl M, et al: Investigation of plaque psoriasis relapse after secukinumab withdrawal in patients from two phase III studies. Clin Exp Dermatol 2024; 49(8): 793-800.
- Iversen L, et al: Secukinumab demonstrates superiority over narrow-band ultraviolet B phototherapy in new-onset moderate to severe plaque psoriasis patients: Week 52 results from the STEPIn study. JEADV 2023; 37: 1004-1016.
- Cheuk S, et al: Epidermal Th22 and Tc17 cells form a localized disease memory in clinically healed psoriasis. J Immunol 2014; 192(7): 3111-3120.
- Wu H, et al: Pathogenic role of tissue-resident memory T cells in autoimmune diseases. Autoimmun Rev 2018; 17: 906-911.
- Schäkel K, et al: Early disease intervention with guselkumab in psoriasis leads to a higher rate of stable complete skin clearance (‘clinical super response’): Week 28 results from the ongoing phase IIIb randomized, double-blind, parallel-group, GUIDE study. JEADV 2023; 37(10): 2016-2027.
DERMATOLOGIE PRAXIS 2024; 34(6): 18-20 (published on 13.12.24, ahead of print)