At the Update Refresher General Internal Medicine, diagnostic and therapeutic strategies for various gastroenterological diseases were discussed. Among other things, the common clinical pictures of chronic constipation and diarrhea were discussed. In addition, the question arose as to which clarifications are useful in liver cirrhosis and celiac disease.
Chronic constipation is a clinical picture that is frequently encountered in everyday practice. Simplified, the motto is: “Too hard and too seldom”. First, it is important to exclude secondary causes (colonoscopy, if necessary). Possible differential diagnoses of secondary constipation include medication use (especially opiates, sympathomimetics), mechanical causes (e.g., strictures, anal fissure, colorectal carcinoma), neurologic or metabolic disorders, myopathy, and other factors such as depression, dementia, and immobility. Once these points are ruled out, a gradual laxative therapy usually follows. It is also important to take away from the patient possible fears of an “internal poisoning by Obstipation” or similar, so Dr. med. Marcel Halama, medical center Fluntern.
Laxative measures initially include lifestyle counseling (exercise, hydration, high-fiber diet, etc.). After that, fiber/swelling agents such as psyllium, wheat bran, ispaghula and psyllium are used. “The substances do not act immediately. Therefore, do not order the patients again until after four weeks,” the expert advised. If this does not achieve the desired effect, osmotic laxatives can be added as an add-on. These include, for example, salts such as magnesium and sodium sulfate, sugar (alcohols) such as lactulose, sorbitol, and – the most important and nowadays most frequently used group – polyethylene glycols such as macrogol (Laxipeg®) or Transipeg®. The fourth stage is followed by stimulant laxatives (e.g., Senna, bisacodyl p.o./supp.). Since there are many different dosage forms, from powder to syrup to dragées and suppositories, the patient’s preferences can also be taken into account in the choice of medication.
Special clarifications
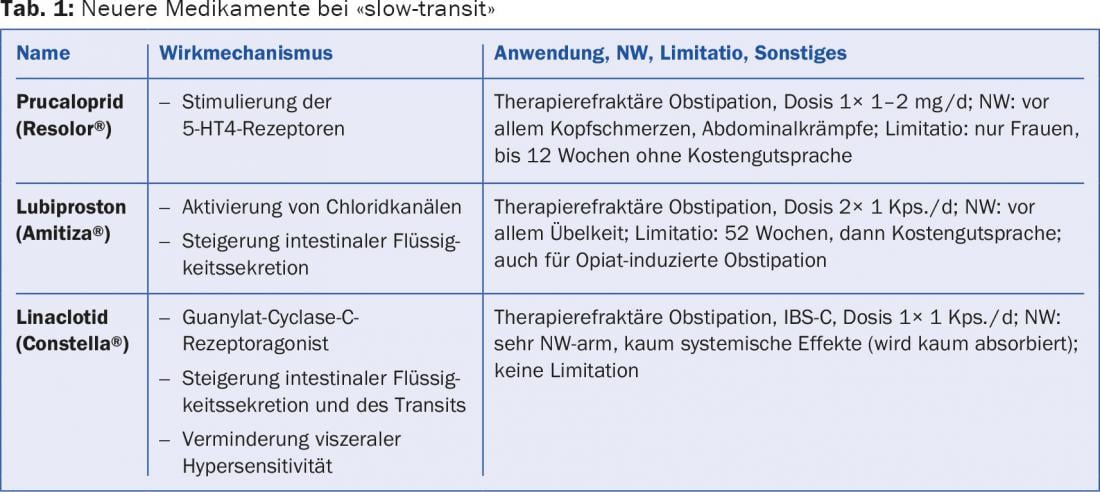
If the above measures still do not make any progress, special clarifications can be considered. One of them is transit time determination (measurement of colonic passage time with radiopaque markers). In addition to constipation with normal transit time, there are mild and severe forms of slow-transit constipation (table 1). The mild form should be treatable with conventional laxatives, whereas the severe form, which is found mainly in young women and in enteric neuropathy, poses greater challenges for the physician. In this case, almost all the markers are still in the intestine when the X-ray is taken on the seventh day. “Colon transit time shows a correlation to the Bristol Stool Chart, so using this scale is helpful when dealing with the patient – especially when there are difficulties in communication,” Dr. Halama said.
25% of the chronically constipated have anorectal voiding dysfunction. Anorectal manometry provides valuable information in this regard. This examination provides information about the pressure conditions in the area of the sphincter of the rectum or rectum. of the anal canal. Structural problems, in turn, can be detected with (MR) defecography.
Diarrhea
Chronic diarrhea (over four weeks) has a very broad differential diagnosis, so a focused history is important. This includes the question of any existing B symptoms (fever, night sweats, weight loss), a connection with food (e.g. lactose/fructose), the medications taken, previous operations/diseases or underlying diseases (thyroid, diabetes, etc.) and stays abroad (parasites).
The inflammatory marker calprotectin is particularly important in the workup. Diarrhea with negative calprotectin may be due to irritable colon, food intolerance, or microscopic colitis. The latter is characterized by the diagnostic triad of chronic watery diarrhea, normal colonoscopy, and pathologic histology and is divided into the two subtypes collagenous colitis (chronic intermittent course in 90% of cases) and lymphocytic colitis (>80% spontaneous healing). There is no progression from one subform to the other. “Especially in women over 50 years of age, one should think about this clinical picture,” advised the speaker. “Autoimmune diseases are clustered in microscopic colitis. Patients with celiac disease who still have diarrhea after a diet may therefore want to be evaluated for the disease.” Therapy is budesonide 9 mg/d and/or loperamide (Imodium®) up to 16 mg/d for eight to twelve weeks. “Anyway, loperamide 2-16 mg/d as drops, sublingually or as capsules is firmly established in the treatment of diarrhea and is the best drug in this indication. The study situation is very good and you can dose high,” says Dr. Halama.
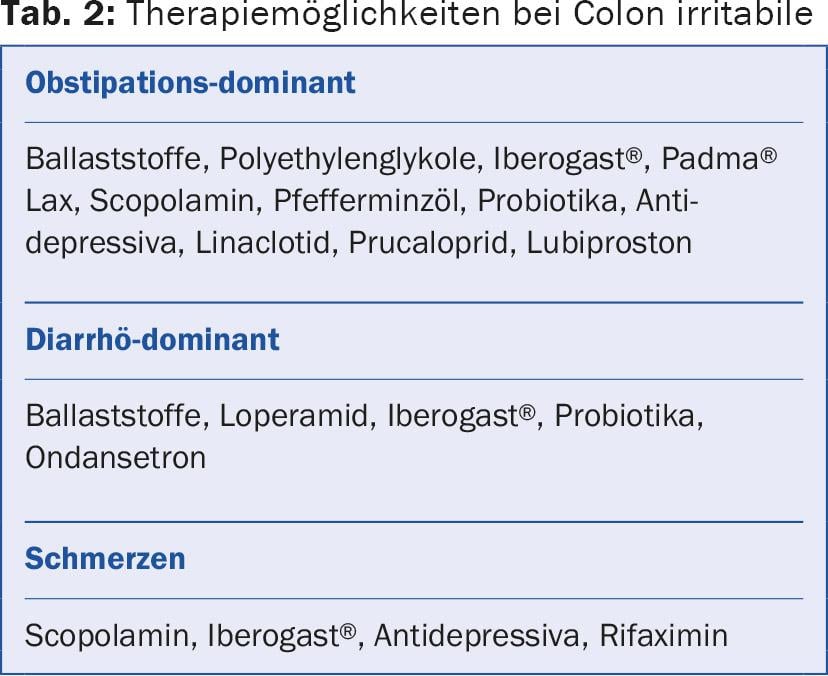
Therapeutic options for irritable colon are shown in Table 2 . Very well effective for irritable bowel is peppermint oil. This is available in capsule form (Colpermin®, 3× 1-2 Kps./d before meals). Among the antidepressants, trimipramine 10-50 mg/d and amitriptyline 10-30 mg/d show significant pain reduction in irritable bowel syndrome.
How to proceed if liver cirrhosis is suspected?
According to Beat Helbling, M.D., Gastroenterology Bethany, it is crucial to detect liver cirrhosis early (“think about it and specifically look for it”). Laboratory changes are often discrete, as are ultrasound signs. The staging or location of liver cirrhosis is therefore supplemented by the following investigation options: fibroscan, liver biopsy and gastroscopy. Fibroscan is a convenient, painless, non-invasive procedure that provides an indication of liver stiffness (the higher the kPa value recorded, the harder the liver). Thus, the measurement shows a correlation to fibrosis. The gold standard is liver biopsy. It provides additional information on the:
- Staging (present): exact degree of fibrosis, amount of fat, information about possible cause
- Grading (future): Statement on inflammatory activity/prognosis, differentiation of fatty liver from steatohepatitis.
Gastroscopy is used to find varices and is necessary at least once if cirrhosis is confirmed. A six-monthly ultrasound allows detection of hepatocellular carcinoma (HCC).
The two prognostic scores CHILD and MELD are helpful only in advanced cirrhosis. CHILD provides a long-term forecast and MELD provides a short-term forecast. By clarifying and addressing etiology (chronic hepatitis B/C, alcohol, hemochromatosis) and treating complications (portal hypertension: ascites, spontaneous bacterial peritonitis, hepatorenal syndrome, varices; HCC), one can influence the prognosis of cirrhosis. “Remember: viral hepatitis should always be sought and, if present, definitely treated. For antiviral therapy in HBV cirrhosis, for example, tenofovir can be considered. You are familiar with the excellently effective and tolerable new oral hepatitis C drugs – much has been written about them in the specialist and lay press. So here we have an extremely expensive therapy that actually cures it,” says Dr. Helbling.
One possible consequence of end-stage cirrhosis is hepatic encephalopathy. Early symptoms here are concentration disorders, dyscalculia, sleep disorders and daytime fatigue. A new drug in this indication is called rifaximin (Xifaxan®). In a meta-analysis, antibiotics were superior to non-absorbable lactulose in terms of ameliorating hepatic encephalopathy [1].
Celiac disease clarification
According to Prof. Dr. med. Stephan Vavricka, Stadtspital Triemli, a serology should be carried out before the gluten diet. The best marker in sprue serology is anti-tissue transglutaminase antibodies. Anti-gliadin and anti-endomysium antibodies are other specific celiac disease antibodies. It is important to actively exclude selective IgA deficiency, a condition that occurs more frequently in celiac disease patients (prevalence 1.7-3%), by determining total IgA. Another diagnostic step is small bowel biopsy (gold standard: six biopsies from pars II duodeni). Histology shows total or partial atrophy of the villi, increased intraepithelial lymphocytes, and proliferation of lymphocytes in the lamina propria. Figure 1 summarizes the diagnostic algorithm again.
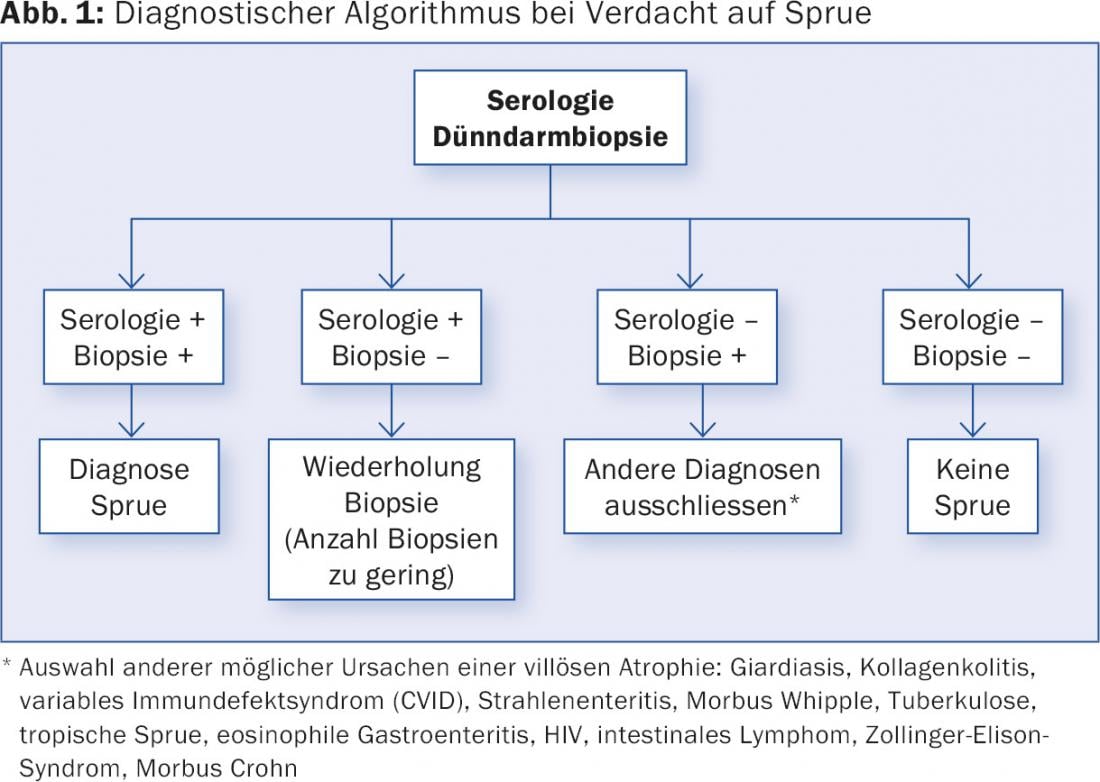
Three to six months after starting a gluten-free diet, serology should normalize, and finally, after six to twelve months, histology should normalize as well. In addition to the above-mentioned examinations, there are also genetic tests for the clarification of celiac disease. HLA genotyping excludes celiac disease with a negative result (HLA DQ2/DQ8 negative) in more than 99%. Conversely, the presence of one of these alleles does not indicate celiac disease, as they are also present in about 20% of the healthy population.
The following can be said about the differentiation of the various “gluten diseases”: On the one hand, there is the differentiation also at the highest level according to autoimmune and allergic forms. While celiac disease (whether symptomatic or asymptomatic) and dermatitis herpetiformis Duhring have an autoimmune genesis, in wheat allergy this is – as the name suggests – allergic in nature. The latter may be accompanied by asthma, diarrhea or urticaria. A recently increasingly discussed and researched non-autoimmune mediated form of “gluten disease” is the so-called non-celiac gluten sensitivity (NCGS). This is a diagnosis of exclusion (no celiac disease, no wheat allergy).
Source: Update Refresher General Internal Medicine, November 4, 2015, Zurich
Literature:
- Als-Nielsen B, Gluud LL, Gluud C: Non-absorbable disaccharides for hepatic encephalopathy: systematic review of randomised trials. BMJ 2004 May 1; 328(7447): 1046.
HAUSARZT PRAXIS 2016; 11(1): 45-47











