The Interventional Cardiology Symposium at the University Hospital Zurich was also dedicated to anticoagulants and antiplatelet agents. Here, the question was “one, two, or three?” As it turned out, the duration and type of combination in dual platelet inhibition are best chosen individually and depend on the ischemic and bleeding risk. Triple therapy for VHF and acute coronary syndrome/stenting should be as brief as possible. For certain cases, a dual approach consisting of (N)OAK and clopidogrel is an option.
Prof. Thomas F. Lüscher, MD, Clinic Director of the Department of Cardiology at the University Hospital Zurich, discussed the question: “Dual antiplatelet therapy (DAPT) – which combination and for how long? New revascularization guidelines were published in 2014 on the situation in stable coronary artery disease (CAD) and after percutaneous coronary intervention. They recommend DAPT after implantation of a drug eluting stent (“DES”) for a period of six months (IB recommendation). A shorter duration of therapy may be considered in patients at high risk of bleeding, and a longer duration in patients at low risk of bleeding but high risk of ischemia. The importance of DAPT is in preventing stent thrombosis and preventing reoccurrence. But how long is long enough (6, 12, 24 months)? And what are the dangers?
Overview of the study situation
In addition to aspirin, the following antiplatelet agents are available: Ticagrelor, prasugrel, clopidogrel. In recent years, the following findings have been obtained in their clinical trials:
CAPRIE trial: clopidogrel produced a significantly lower cumulative event rate of ischemic stroke, myocardial infarction, or vascular death than aspirin (relative risk reduction of 8.7% at three years, p=0.043) in 19 185 patients who had recently suffered a stroke or myocardial infarction or had symptomatic peripheral arterial disease [1].
CURE study: In 12,562 patients with acute coronary syndrome, clopidogrel added to aspirin significantly reduced the ischemic event rate consisting of cardiovascular death, myocardial infarction, or stroke compared with aspirin plus placebo (risk reduction of 20% after one year, p<0.001). However, there were also significantly more individuals with severe bleeding (RR 1.38, p=0.001) [2].
TRITON trial: In 13,608 patients with acute coronary syndrome and percutaneous coronary intervention (PCI), prasugrel performed better than clopidogrel (both added to low-dose aspirin) in the primary endpoint, which was defined the same as in CURE. The event rate was 12.1 vs. 9.9%, representing a significant 19% risk reduction at 15 months (HR 0.81; 95% CI 0.73-0.90; p<0.001). Stent thrombosis was also significantly less frequent. However, more major bleeding again occurred with prasugrel (2.4 vs. 1.8%; HR 1.32; 95% CI 1.03-1.68; p=0.03) [3].
DAPT study: The so-called DAPT study [4], which was presented last year at the AHA congress, among others, attracted much attention: 9961 patients with CHD and DES were randomized and observed over approximately three years (33 months). Either they received DAPT (aspirin + clopidogrel or prasugrel) for 12 months and then only aspirin plus placebo, or dual therapy was extended to 30 months. Prolonged therapy reduced the risk of so-called in-stent thrombosis by more than two-thirds after 30 months: in the study group, the rate was (0.4% vs. 1.4%; HR 0.29; 95% CI 0.17-0.48; p<0.001). The coprimary end point consisting of relevant cardiovascular or cerebrovascular adverse events also showed a significant 29-
percent difference in favor of the long-term therapy variant. Bleeding was again significantly more frequent by prolonging DAPT.
PEGASUS Study: Results from the PEGASUS study were recently presented at the 2015 ACC Congress in San Diego. They showed that patients who had suffered a myocardial infarction more than one year previously benefited from ticagrelor added to aspirin in the primary end point (defined the same as in CURE): Risk decreased with a dose of 2× 90 mg/d significantly by 15% and with a dose of 2× 60 mg/d by 16% compared to placebo (follow-up: three years). However, as expected, they also suffered severe bleeding significantly more often [5].
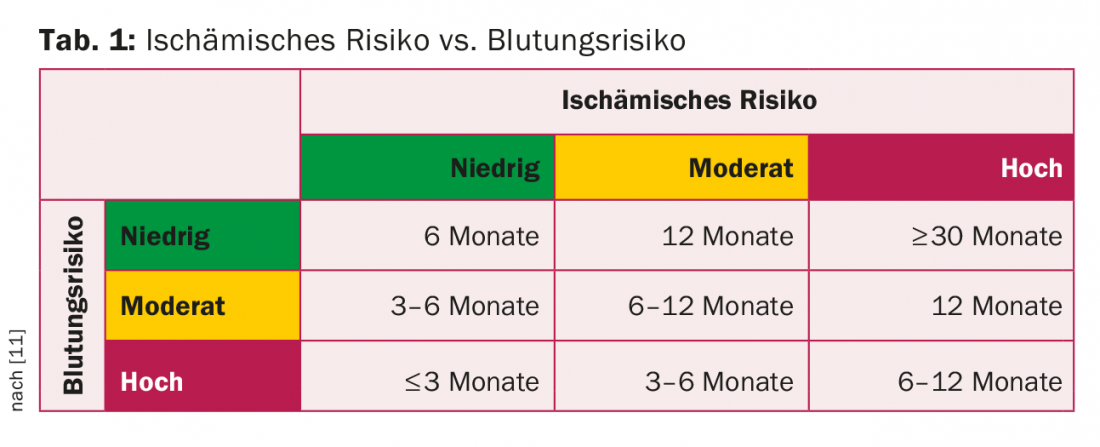
“In stable CHD, I would recommend ticagrelor (alternatively clopidogrel) for DAPT after PCI in view of the current study situation, and prasugrel (STEMI) and ticagrelor (NSTEMI) for acute coronary syndrome,” Prof. Lüscher said. “On the risk-benefit scale, the benefit must clearly outweigh the risk: Prevention of death, infarction, and stent thrombosis are the goals – this with as little increase in the risk of bleeding as possible.” Therefore, with regard to duration, an individualized approach is most appropriate: for example, the complexity of coronary changes and comorbidities have a critical impact on future acute coronary syndrome events, which may necessitate an increase in the duration of therapy. “It is important to find the so-called sweet spot between protection and bleeding (tab. 1),” advised Prof. Lüscher. “Young, stable, and otherwise healthy patients are recommended to receive DAPT for three to six months, and for acute coronary syndrome for twelve. Complex patients with peripheral arterial disease, diabetes, etc., should be treated longer if necessary.”
Triple Therapy
Prof. Dr. med. Jürg Hans Beer, Chief Physician, Department of Internal Medicine, Kantonsspital Baden, discussed the issue of triple therapy. Here, the problem of the risk-benefit analysis becomes even more acute. “In principle, the motto is: bleeding is rarely good for you,” Prof. Beer said. A large Danish cohort study [6] showed that fatal and nonfatal bleeding in atrial fibrillation (VHF) already increased with dual therapy-but increased significantly more with triple treatment consisting of warfarin, aspirin, and clopidogrel, more than threefold compared with warfarin monotherapy (HR 3.7; 95% CI 2.89-4.76).
The following findings have been made in the field of atrial fibrillation in recent years:
Atrial fibrillation without CAD/stent: Here, the addition of aspirin to oral anticoagulation with warfarin has been shown to cause a significant swing in favor of the risk side: The risk of suffering a major bleed increased by a significant 53% within six months [7].
Atrial fibrillation after PCI: Dual therapy with clopidogrel and oral anticoagulation (OAC) significantly reduces the risk of bleeding by 64% compared with triple treatment with OAC, aspirin, and clopidogrel (cumulative incidence 19.4 vs. 44.4%), according to the WOEST trial [8]. The secondary endpoint defined as death, myocardial infarction, or stroke also occurred significantly less frequently. Specifically, the risk was reduced by 40% with dual therapy (p=0.025). A closer look showed that the difference was mainly due to minor bleeding, and major bleeding was not significantly less frequent. Overall, WOEST nevertheless found a clear swing to the benefit side by omitting one agent, which Lamberts and colleagues [9] confirmed again in the same year. They also conclude that clopidogrel and OAK perform at least as well as, and tend to perform better than, triple therapy in terms of safety and efficacy. As a follow-up to the WOEST trial, the AHA/ACC/HRS societies issued a class IIb recommendation (evidence B) for the combination of a vitamin K antagonist (VKA) and clopidogrel (VHF patients after PCI). The 2014 ESC guidelines also consider the dual approach with (N)OAK and 75 mg/d clopidogrel an alternative for selected patients.
Furthermore, in triple therapy, clopidogrel should never be replaced by prasugrel – otherwise the bleeding rate increases significantly (risk increase by a factor of 4.6), as a 2013 study showed [10]. The same has been true so far for ticagrelor.
Conclusion
So, in summary, there are currently two options for VHF and acute coronary syndrome/stenting:
- First, one can treat with oral anticoagulation and DAPT, preferably for as short a time as possible (1, 3, or 6 months). If the new oral anticoagulants are used, the lower dosage should be selected. With VKA, aim for a target INR of 2-2.5. Prasugrel and ticagrelor should be avoided in triple therapy.
- On the other hand, in some cases a dual approach with (N)OAK and clopidogrel is possible.
Source: Symposium Interventional Cardiology, March 26, 2015, Zurich
Literature:
- CAPRIE Steering Committee: A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). CAPRIE Steering Committee. Lancet 1996 Nov 16; 348(9038): 1329-1339.
- Yusuf S, et al: Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med 2001 Aug 16; 345(7): 494-502.
- Wiviott SD, et al: Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 2007; 357: 2001-2015.
- Mauri L, et al: Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. N Engl J Med 2014 Dec 4; 371(23): 2155-2166.
- Bonaca MP, et al: Long-Term Use of Ticagrelor in Patients with Prior Myocardial Infarction. N Engl J Med 2015 Mar 14 [Epub ahead of print].
- Hansen ML, et al: Risk of bleeding with single, dual, or triple therapy with warfarin, aspirin, and clopidogrel in patients with atrial fibrillation. Arch Intern Med 2010 Sep 13; 170(16): 1433-1441.
- Steinberg BA, et al: Use and associated risks of concomitant aspirin therapy with oral anticoagulation in patients with atrial fibrillation: insights from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF) Registry. Circulation 2013 Aug 13; 128(7): 721-728.
- Dewilde WJ, et al: Use of clopidogrel with or without aspirin in patients taking oral anticoagulant therapy and undergoing percutaneous coronary intervention: an open-label, randomised, controlled trial. Lancet 2013 Mar 30; 381(9872): 1107-1115.
- Lamberts M, et al: Oral anticoagulation and antiplatelets in atrial fibrillation patients after myocardial infarction and coronary intervention. J Am Coll Cardiol 2013 Sep 10; 62(11): 981-989.
- Sarafoff N, et al: Triple therapy with aspirin, prasugrel, and vitamin K antagonists in patients with drug-eluting stent implantation and an indication for oral anticoagulation. J Am Coll Cardiol 2013 May 21; 61(20): 2060-2066.
- Binder RK, Lüscher TF: Duration of dual antiplatelet therapy after coronary artery stenting. Cardiovascular Medicine 2015; 18(1): 3-5.
CARDIOVASC 2015; 14(3): 31-34