In contrast to the past, other treatment goals beyond glycemic control are sought nowadays. The current guidelines and consensus recommendations of international diabetology societies take into account the results of large outcome studies in which an additional cardiovascular benefit of GLP-1 receptor agonists and SGLT-2 inhibitors has been demonstrated. The ADA/EASD consensus report specified criteria for drug selection.
The most important points of the consensus report of ADA (“American Diabetes Association”) and EASD (“European Association for the Study of Diabetes”) were presented by Prof. Dr. med. Michael Nauck from the Ruhr University Hospital in Bochum [1]. It is important to assess patients with type 2 diabetes mellitus individually and translate this into a treatment strategy with stringent or less stringent glucose control.
Use of GLP-1-RA and SGLT-2 inhibitors independent of HbA1c level.
After diagnosis, patients should first be educated regarding lifestyle management and baseline therapy with metformin is recommended if the individual HbA1c target has not been achieved by lifestyle modification alone. In addition, SGLT-2 inhibitors and GLP-1 receptor agonists (GLP-1-RA) should be used because of the empirically demonstrated cardiovascular benefits of these classes of agents. Diabetics have an increased risk of cardiovascular sequelae such as heart attack and stroke compared to people without this metabolic disease. The cardio- and nephroprotective effects of GLP-1-RA and SGLT-2 inhibitors open new therapeutic perspectives here. If diagnosed early, they can contribute not only to the stabilization of glucose metabolism but also to cardiovascular and renal prevention.
EASD/ADA consensus recommendations: Update on new substance classes
The large cardiovascular endpoint studies of the past decade have demonstrated the particular importance of representatives from the GLP-1 RA (liraglutide, dulaglutide, semaglutide) and SGLT-2 inhibitor (empagliflozin, dapagliflozin, canagliflozin) substance classes. These results have also been incorporated into the 2020 updated consensus report of European and American diabetologists (EASD/ADA) [2]. Accordingly, GLP-1 receptor agonists or SGLT-2 inhibitors should be recommended to patients with type 2 diabetes for cardiovascular risk reduction.
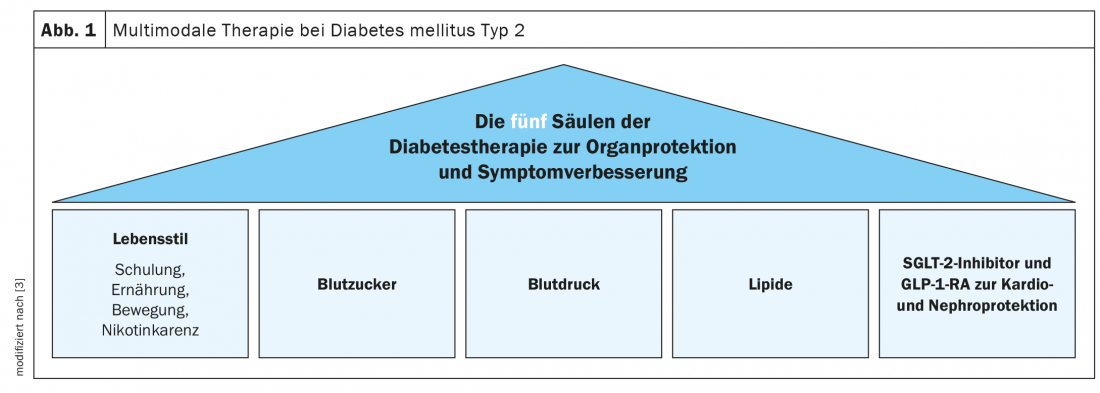
In various international guidelines, SGLT-2 inhibitors and GLP-1-RA are now established as treatment options with proven additional cardiovascular and renal benefits. The German Diabetes Society has added these substance classes as one of the five pillars of diabetes therapy for type 2 diabetes (Fig. 1) [3].
Dulaglutide for cardiovascular primary prevention.
With regard to drug selection, the ADA/EASD consensus report differentiates as follows:
GLP-1-RAs are the first choice to prevent cardiovascular events (MACE) when a diabetic patient has manifest cardiovascular disease (after myocardial infarction, stroke, revascularization) OR is at high cardiovascular risk (age ≥55 years plus left ventricular hypertrophy or arterial stenosis >50% in coronaries, carotids and/or peripheral arteries).
In diabetic patients with heart failure and reduced ejection fraction (HFrEF <45%), SGLT-2 inhibitors are primarily recommended because this class of agents has the best evidence in this regard to prevent hospitalizations for heart failure, MACE, and cardiovascular death.
In case of intolerance or contraindication to an SGLT-2 inhibitor or inadequate renal function, experts advise GLP-1 RA and vice versa. If glycemic control is inadequate, the two groups of substances can be combined.
Congress: Diabetology without borders 2021
Literature:
- Nauck M: ADA/EASD consensus paper. Prof. Michael Nauck, MD, Diabetology without borders, Feb. 27, 2021.
- Buse JB, et al: 2019 update to: Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 2020; 63(2): 221-228.
- Kellerer M: Practice guideline of the German Diabetes Society. Prof. Dr. med. Monika Kellerer, Diabetology without borders, 27.02.2021.
FAMILY DOCTOR PRACTICE 2021