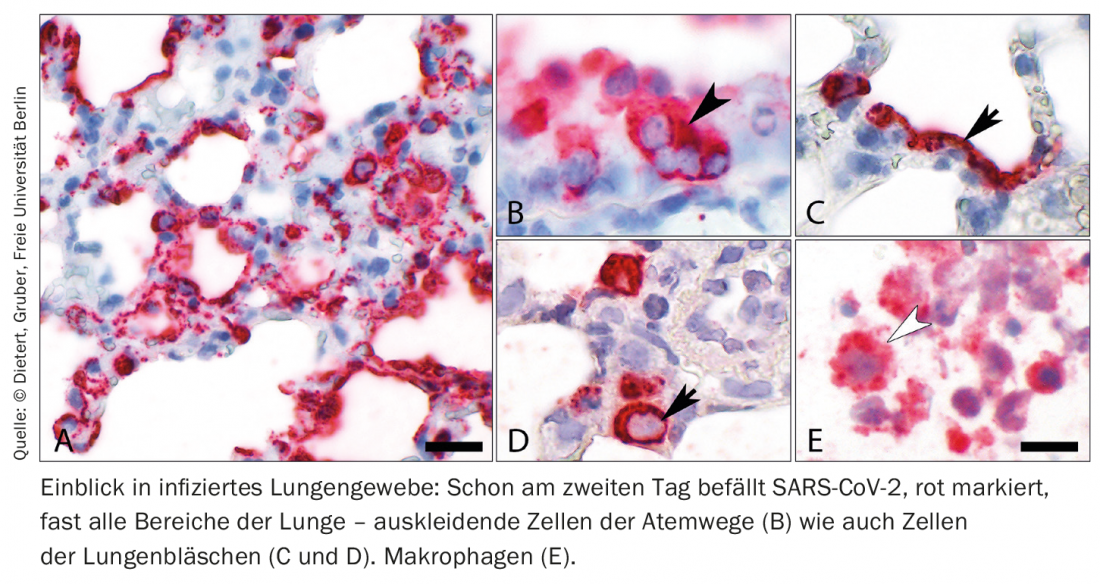
Researchers have studied in detail the cellular mechanisms at the onset of inflammatory lung injury triggered by SARS-CoV-2 infection. Accordingly, the damage that necessitates ventilation is not caused by direct destruction of the lungs by the multiplication of the virus. Rather, inflammatory processes and the endothelium of the lung are significantly involved in severe courses.
For the past year and a half, researchers around the world have been trying to understand COVID-19, a disease caused by the SARS-CoV-2 coronavirus. To date, there are almost no drugs to treat the disease. One of the hurdles: COVID-19 is caused, among other things, by a misguided, sometimes exuberant reaction of the body’s immune system. In order to find therapeutic targets, it is necessary to understand in detail how and where exactly which adverse processes are triggered in the body. Patient-centered research is reaching its limits here – especially when it comes to investigating disease mechanisms in the early phase of infection. Biomaterial as a basis for studies is usually only accessible after admission to a hospital. In the case of mild or moderate courses associated with pneumonia, it is usually not possible to obtain any tissue at all from the lungs – the risk would be too high for acutely ill patients. What remains is the analysis of cell tissue after the death of COVID-19 patients.
Using available patient samples, the team led by Prof. Dr. Martin Witzenrath, Deputy Director of the Medical Clinic with a focus on Infectiology and Pneumology at Charité, was able to gain valuable information about the mechanisms and course of the disease. In addition, in order to study lung areas that cannot be readily viewed in patients and to gain insight into the early phase of the disease, the research team was looking for a suitable model. In international COVID-19 research, as well as in SARS-CoV-1 research, hamster models have proven informative. “We wanted to know whether the models could be used to develop new therapeutic approaches, and we tried to find findings from samples taken from patients in them,” says Prof. Witzenrath. “We were particularly interested in the endothelial cells of the lung, the barrier that lines the blood vessels. This loses function in severe COVID-19, eventually leading to lung failure.”
Animal model with hamsters
In their current work, the scientists performed a detailed characterization of SARS-CoV-2 infection in animal models and supported this with data sets from samples taken from patients. The analysis is designed to harness the most important non-transgenic model currently available for COVID-19, the golden hamster, for the development of therapies. Hamsters become infected with the same virus variants as humans. They also develop similar symptoms of disease, and their lungs are damaged when they become severely ill. In this context, COVID-19 progresses differently in individual species. While it usually takes only a moderate course in golden hamsters, Roborovski dwarf hamsters become severely ill.
While the immune system goes into turmoil in the wake of a COVID-19 attack, SARS-CoV-2 initially proliferates weakly in the lungs and respiratory cells. “The destruction of lung tissue in severe COVID-19 courses is not directly caused by the multiplication of the virus in the cells, but by the strong inflammatory response,” explains MDC scientist Dr. Emanuel Wyler. “This seems to be true of the cells of the blood vessels, especially the endothelial cells in the lungs, as well. They react strongly to the virus but are not infected by it and do not perish.” If the disease takes a severe course, occluded blood vessels and unstable vascular walls can lead to acute lung failure.
Model to help develop therapies
In moderate COVID-19 disease, on the other hand, vascular damage is very unlikely to play a role. “We had expected that the endothelium is activated in COVID-19. The fact that these cells are at the same time an active motor of inflammation rather surprised us,” says Prof. Witzenrath. Accordingly, there are two ways of therapeutically attacking these cells, which are central to the course of the disease: First, with substances that seal the endothelial barrier. On the other hand, with those that calm the endothelium. One of them, he said, has already been researched and shown to be successful in pneumonia and ventilation. Anti-inflammatory drugs against COVID-19 that are also currently being tested target the immune response as such – they also act on monocytes and macrophages and slow down their activity.
The now confirmed model is expected to contribute to the development of effective and safe therapies in COVID-19. The goal is to reduce the number of patients with severe lung damage. Currently, the multidisciplinary research team is analyzing the responses of different cell types in the Roborovski dwarf hamster. The researchers want to find out why the infection is more severe here and not self-limiting as in the case of the golden hamster.
Source: Charité, MDC and Freie Universität Berlin (D)
Literature:
- Nouailles G, Wyler E, Pennitz P, et al: Temporal omics analysis in Syrian hamsters unravel cellular effector responses to moderate COVID-19. Nat Commun 2021; 12: 4869; doi: 10.1038/s41467-021-25030-7.0.
InFo PNEUMOLOGY & ALLERGOLOGY 2021; 3(3): 36.