Symptoms of heart failure are a common consequence of various cardiovascular risk factors. As a rule, the primary care physician is the first point of contact and important therapeutic advisor in further disease management. The recently updated European Society of Cardiology (ESC) guideline provides an evidence-based foundation to help heart failure patients individually according to the latest state of knowledge. Various therapeutic principles have been revised and there are also new concepts in the management of concomitant diseases.
The most common causes of chronic heart failure are coronary artery disease (CAD) and/or hypertension. Prevalence increases with age, and untreated patients with heart failure have a high risk of mortality. Diagnosis and differentiation from other diseases is challenging because symptoms are often nonspecific. Patients with dyspnea, impaired exercise capacity, and fluid retention should be evaluated for possible heart failure. Classification tools include the NYHA* criteria and the American College of Cardiology and American Heart Association (AHA) classifications [1]. The categorization of heart failure according to functional pathophysiology has not changed significantly in the recently published updated guideline of the European Society of Cardiology (ESC), which continues to be based on left ventricular ejection fraction (LVEF) [2,3]: HFrEF is present in ≤40%, HFmrEF in 41-49%, and HFpEF in ≥50%. Also largely unchanged is the overall treatment goal: to improve the clinical condition of patients, thereby contributing to a reduction in the risk of hospitalization and mortality, and to improve the quality of life of those affected.
* NYHA = New York Heart Association
HFrEF: simplified therapy algorithm and inclusion of phenotypes.
For heart failure with reduced ejection fraction (HFrEF), the treatment regimen has been significantly modified. The guideline authors have moved away from the conventional staging scheme and opted for a simplification of the algorithm. The most important key points at a glance [2,3]:
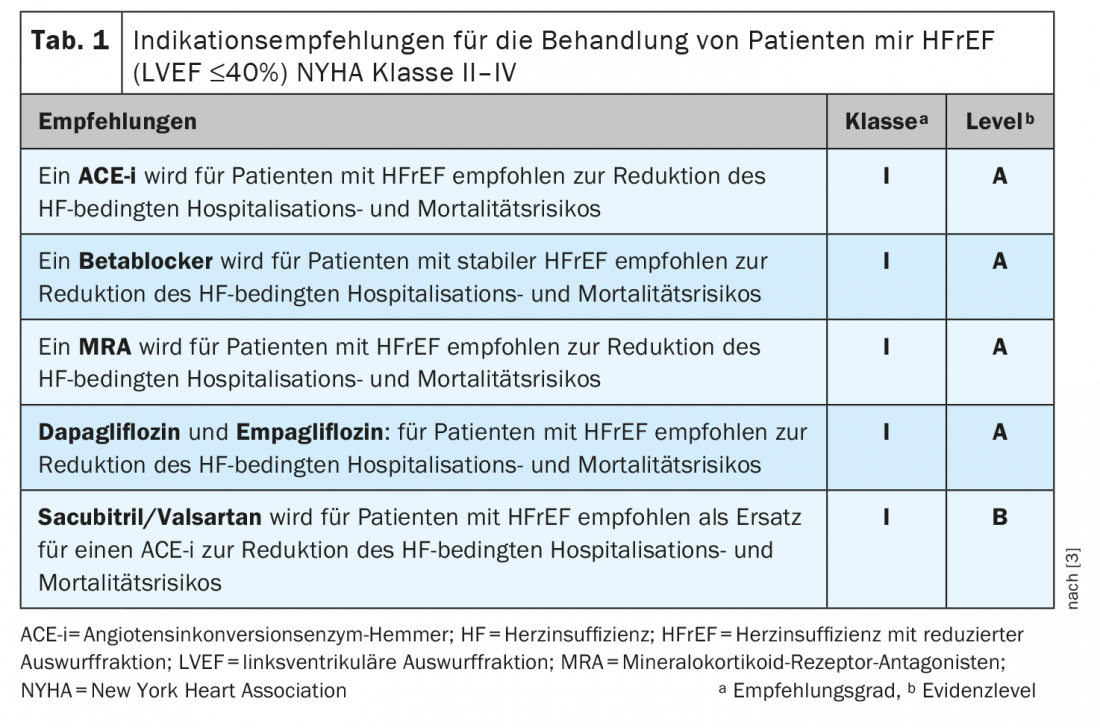
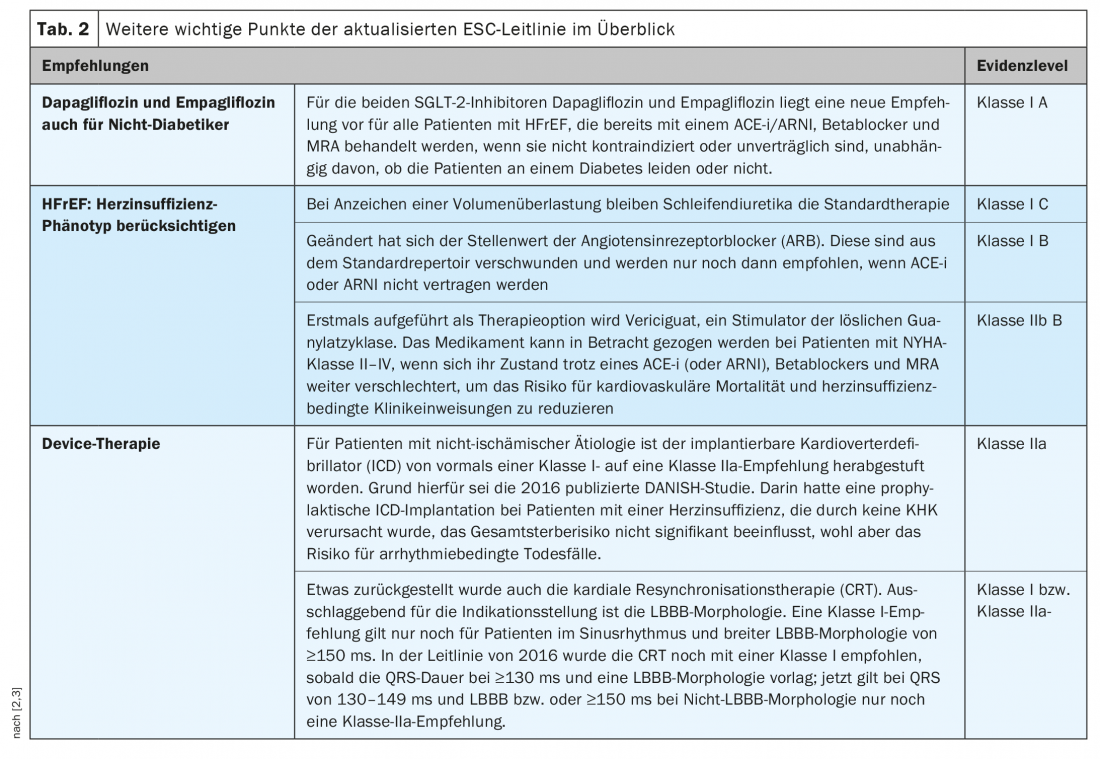
These four key medications are essential: every patient with HFrEF should receive an ACE inhibitor (ACE-i) or angiotensin receptor neprilysin inhibitor (ARNI), a beta blocker, a mineral corticoid receptor antagonist , and an SGLT-2 inhibitor (dapagliflozin or empagliflozin). All four substances have a Class IA recommendation.
No prescribing of the therapy sequence: the decision as to which of the four listed agents should be prescribed first is left to the physician. Thus, the 2021 updated guidelines no longer specify a treatment sequence. The door has been left open here, commented guideline chair Prof. Theresa McDonagh, MD, King’s College Hospital, London (UK).
Consider heart failure phenotype: Treatment beyond this standard therapy should be tailored to the specific heart failure phenotype, depending on the severity of left bundle branch block (LBBB) etiology (ischemic or nonischemic), heart rate, and concomitant disease.
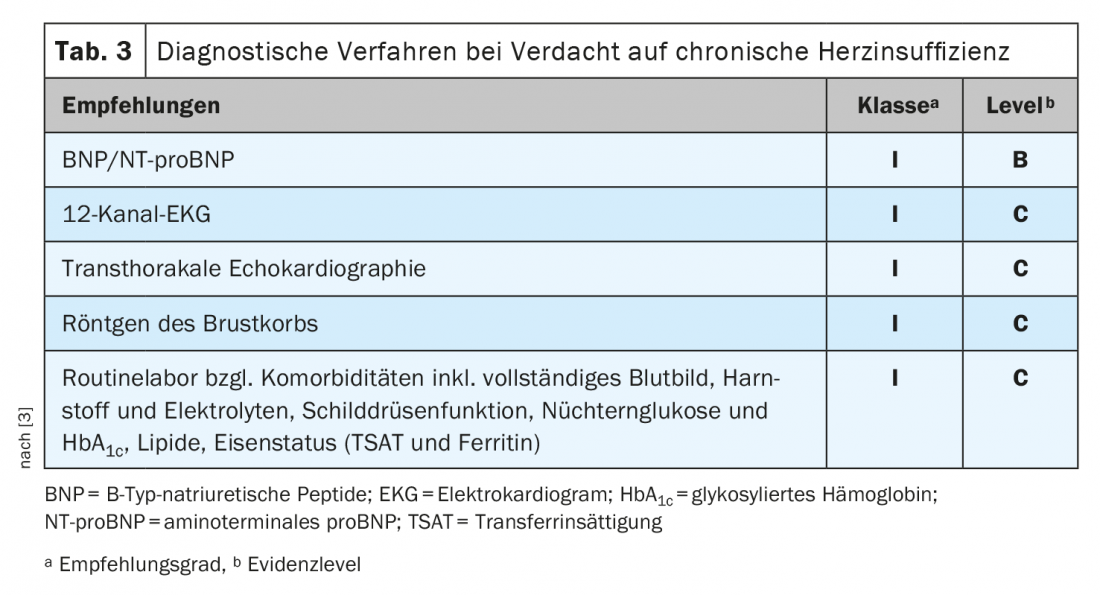
Other important aspects concerning the treatment of HFrEF patients can be seen intables 1 and 2 .
HFpEF: adapted diagnostic algorithm
The three essential criteria in the simplified and more pragmatically designed diagnostic algorithm for patients with preserved ejection fraction (HFpEF) are as follows [2,3]:
- Symptoms and signs of heart failure
- LVEF ≥50%
- Objective evidence of structural and/or functional cardiac abnormalities consistent with left ventricular diastolic dysfunction and elevated LV filling pressures, including elevated natriuetic peptides
Regarding the treatment of HFpEF, the updated guideline is still at the same level as five years ago: Due to a lack of evidence, no drug is currently recommended to improve prognosis. However, there is some movement and it is important to await the results of ongoing HFpEF studies. Of particular interest here is the EMPEROR-Preserved study, which was presented at the ESC Congress shortly after the guideline was published. This indicates that empagliflozin can effectively reduce the risk of heart failure-related hospitalization in HFpEF patients.
HFmrEF: Innovation regarding terminology
According to the new guideline version, the abbreviation HFmrEF no longer stands for “heart failure with mid-range ejection fraction” but for “heart failure with mildly reduced ejection fraction” [2,3]. The reason given for this change was the growing evidence that patients with HFmrEF appear to benefit from HFrEF treatments to a similar extent as HFrEF patients themselves. This is also reflected in the therapy recommendations for these patients. These differ little from those for HFrEF, except that SGLT-2 inhibitors are not listed at all and all other agents aside from diuretics are listed only with a class IIb C recommendation.
In addition: new recommendations for concomitant diseases
There are separate treatment recommendations for HFrEF patients suffering from the following comorbidities [2,3]: atrial fibrillation, hemodynamic instability, chronic coronary syndrome, valvular disease. Specific treatment algorithms have also been developed for patients with heart failure and cancer, pregnancy, acute myocarditis or cardiac amyloidosis. Another important change concerns the recommendation of regular monitoring for a possible iron deficiency or anemia and the therapeutic consequences thereof**: from now on, for symptomatic patients (LVEF <50%) with iron deficiency and recent heart failure-related hospitalization, i.v. iron carboxymaltose administration is recommended to reduce the risk of further hospitalization rather than to improve exercise capacity and quality of life alone, as in the past.
** Serum ferritin <100 ng/ml, or serum ferritin 100-299 ng/ml with transferrin saturation <20%.
Literature:
- “Chronic heart failure: guideline recommends SGLT-2 inhibitors,” www.pharmazeutische-zeitung.de/leitlinie-empfiehlt-sglt-2-hemmer-127991, last accessed Jan. 03, 2022.
- “Heart Failure Guideline 2021 – What’s New, What’s Changed,” Aug. 29, 2021, www.kardiologie.org/esc-kongress-2021/akute-herzinsuffizienz-und-lungenoedem/neue-herzinsuffizienz-leitlinie—das-ist-neu–das-hat-sich-geae/19609474, last accessed Jan. 03, 2022.
- McDonagh TA, et al: ESC Scientific Document Group: 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021 Sep 21;42(36): 3599-3726.
HAUSARZT PRAXIS 2022; 17(1): 26-27