Early correct diagnosis of acute pancreatitis is seminal for the therapeutic approach. While a mild course of disease is expected in the majority of affected individuals, severe acute pancreatitis can be associated with significant morbidity. Infected necrosis is associated with an increased risk of mortality. Assessment of severity and prediction of disease progression are an important basis for patient-oriented choice of adequate treatment.
The updated S3 guideline published under the aegis of the German Society of Gastroenterology, Digestive and Metabolic Diseases (DGVS) summarizes the rapidly evolving state of knowledge on acute and chronic pancreatitis [1]. “Acute pancreatitis is defined pathophysiologically as a primarily sterile inflammation of the pancreas, characterized by nonphysiologic enzyme activation leading to an inflammatory reaction with edema, vascular damage, and cell death,” explains the lead author of the guideline, PD Georg Beyer, MD, LMU Klinikum München [2]. The diagnosis of acute pancreatitis can be made if at least two of the following criteria are present [1]:
- Typical abdominal pain (acute onset, persistent upper abdominal pain, often with girdling radiation to the back)
- Increase of serum lipase to at least three times the upper limit value
- characteristic image morphological findings
Recurrent acute pancreatitis is defined as two or more attacks of acute pancreatitis with symptom-free intervals without evidence of the presence of chronic pancreatitis. This must be distinguished from chronic pancreatitis, in which recurrent episodes of inflammation cause the pancreatic parenchyma to be replaced by fibrotic connective tissue.
Assess severity and course of disease
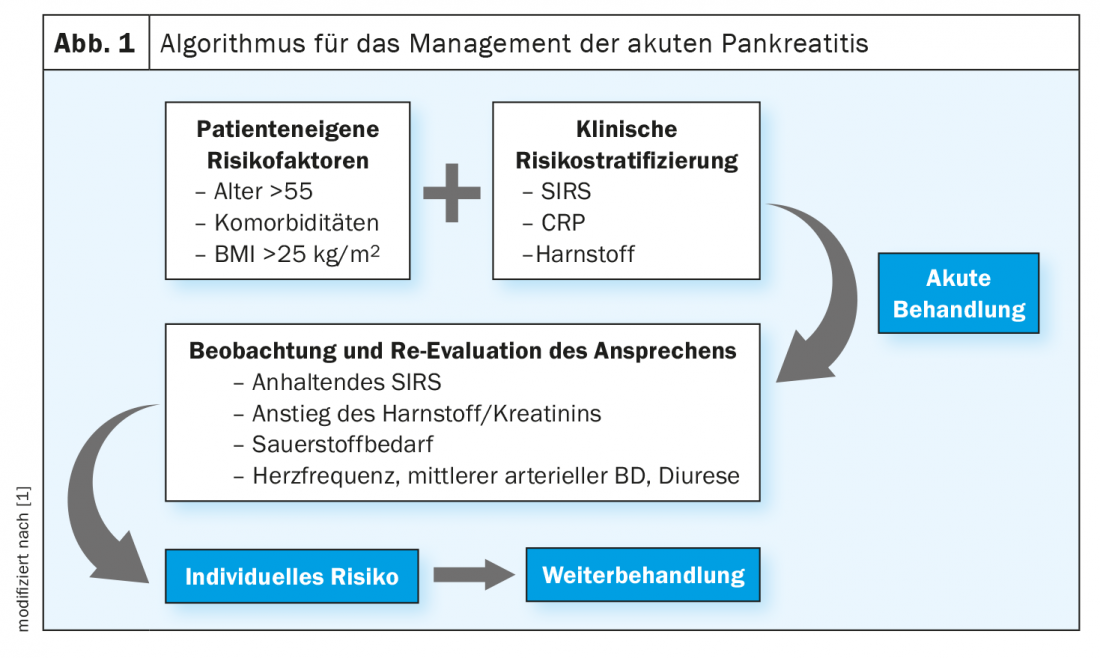
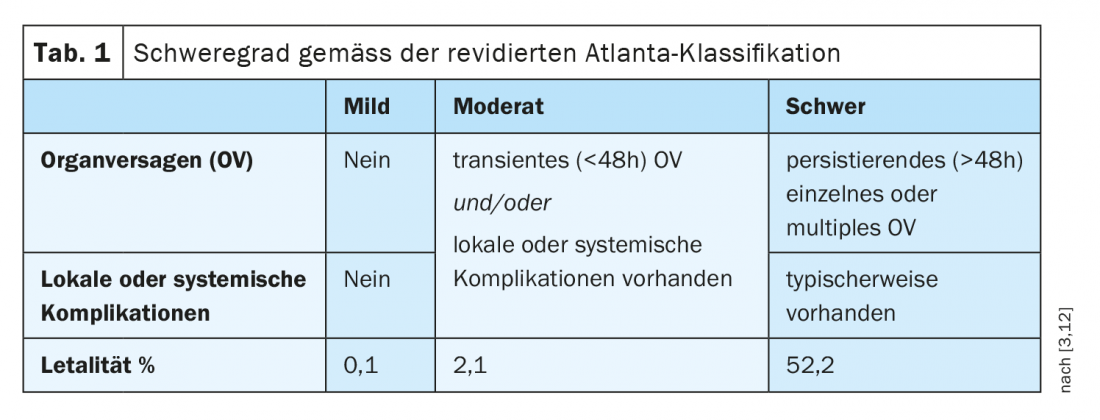
Determinants of the severity of acute pancreatitis include transient (<48 h) and persistent (>48 h) organ failure and local or systemic complications. These prognostic predictors are incorporated into the various severity levels of the revised Atlanta classification (Table 1) [3]. Patient-specific risk factors include older age and certain comorbidities. Patients with metabolic syndrome are at increased risk for a moderate, severe, or lethal course. This seems to be mainly due to the inflammatory activity of visceral fat. The same is true for triglycerides, whose level correlates proportionally and independently of the cause of pancreatitis, with persistent organ failure [4].
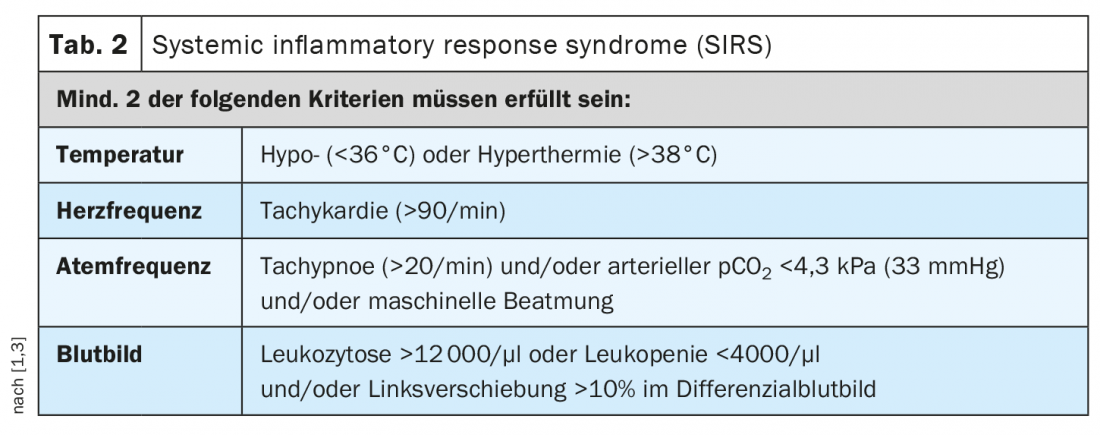
Alcohol-induced acute pancreatitis has a particularly high rate of necrotizing courses that require intensive medical care [5]. Prognostic scoring systems were found to have no significant advantage over determination of systemic inflammatory response syndrome (SIRS) criteria, so the use of SIRS criteria is recommended because of its simplicity (Table 2) [1,3]. If SIRS is present on the day of hospital admission, there is an 85-100% chance of a severe course. The absence of SIRS has a high negative predictive value (98-100%) [7].
If complications of acute pancreatitis are clinically suspected, transabdominal ultrasonography should be performed, followed by contrast-enhanced CT if the findings are inconclusive. Endoscopic retrograde cholangiopancreaticography (ERCP) is not indicated in mild biliary pancreatitis. According to the guideline, it is considered when there is concomitant cholangitis, demonstrable choledocholithiasis, and/or bile duct obstruction. The APEC trial had shown no survival or morbidity benefit of early ERCP (<24 h) in patients with severe pancreatitis without cholangitis [8].
Initiate adequate therapy in appropriate setting
In addition to the correct diagnosis and severity assessment, the correct therapy of pancreatitis in the early phase is of crucial importance. Adequate fluid therapy plays a particularly important role in the patient’s prognosis, as the development and extent of pancreatic necrosis depends on it. The predicted severity is the basis for choosing the appropriate level of care, including the appropriate setting (normal ward, intermediate care, or intensive care unit), to meet the needs of the patient and the vagaries of the disease process. In addition to pain management, for which there are no relevant updates in the new guideline, volume and nutrition therapy are the central components of early therapy.
Volume therapy with Ringer’s lactate solution: Volume therapy should be started early, i.e., preferably within 24 h of confirming the diagnosis of acute pancreatitis. “Compared with isotonic saline, balanced whole electrolyte solutions seem to have advantages, especially in the formation of systemic inflammation,” emphasized Dr. Beyer [2]. The guideline recommends predominantly using Ringer’s lactate solution for initial controlled volume therapy. In the first 24 hours – if necessary after initial bolus administration – the infusion rate should be 200-250 ml/h. In patients with end-stage renal failure or severe congestive heart failure, a lower substitution rate should be selected, if appropriate. Initial volume administration is always performed under monitoring and re-evaluation of important clinical parameters such as blood pressure, heart rate, diuresis and oxygen demand/breath rate. Subsequently, targeted volume therapy should be administered based on ‘blood urea nitrogen’ (or serum urea), hematocrit, and parameters of advanced hemodynamic monitoring in severe acute pancreatitis.
Nutritional therapy: There has been a paradigm shift in nutritional therapy. If possible, oral or enteral feeding should be started as early as possible, in the case of a mild course already on the first day after admission. On the one hand, this helps to halt catabolism and ATP depletion in the pancreas (and thus pancreatic necrosis), and on the other hand, the integrity of the intestinal mucosa is maintained by promoting blood flow, according to Dr. Beyer [2]. Even in patients with a predicted or manifest severe course, the recommendation is to start oral or enteral feeding by tube early, if possible. The background is a meta-analysis according to which an early start of enteral nutrition compared with parenteral nutrition significantly reduces the risk of organ failure and complications [9].
|
Follow-up care for the prevention of consequential damage The risk of recurrence, pancreatic insufficiency, and chronic pancreatitis increases with severity and is dependent on etiology [1]. Therefore, structured outpatient follow-up should be provided after the first episode of acute pancreatitis in the following cases: non-mild severity, alcohol-induced pancreatitis, unclear etiology and age over 40 years, lack of symptom relief after discharge. Empirical data show that structured outpatient follow-up after first episode of alcohol-induced pancreatitis with repeated behavioral intervention significantly reduces the risk of recurrence [11]. In the first two years, patients without symptoms should undergo a clinical examination every 6 months and be evaluated for exocrine and endocrine insufficiency by a general practitioner, practicing internist or gastroenterologist. “Of course, the most important predictor in this situation is alcohol withdrawal,” the speaker said. The goal is complete abstinence from alcohol. Structured follow-up is also recommended in patients over 40 years of age after idiopathic acute pancreatitis. Contrast-enhanced cross-sectional imaging or endoscopy should be performed no later than three months after pancreatitis has healed. After 12-24 months, repeat imaging may be appropriate due to the increased risk of pancreatic cancer. |
Necrotizing pancreatitis: treat in stages
“Infected pancreatic necrosis is one of the most serious complications because it is a predictor or a major cause of organ failure,” Dr. Beyer said. Infected (peri)pancreatic necrosis occurs in 20-40% of severe acute pancreatitis. In these cases, the primary treatment goal is prevention or control of organ failure, not removal of necrosis, the speaker emphasized. Therefore, some restraint would be appropriate. An important note in the guideline is that the indication for intervention should be clinical and not imaging-based. The primary goal should always be the procedure with the least invasiveness possible, as part of a staged approach, starting with antibiosis, followed by small-lumen and large-lumen catheterization, and only in a final step performing necrosectomy. In a randomized trial, 39% of patients required no intervention with this approach, only antibiotics [10]. For intervention, the guideline primarily recommends endoscopic access because it causes fewer fistulas and is associated with a shorter hospital stay. Ultimately, however, local expertise at the center is also an important criterion for the choice of access, Dr. Beyer emphasized.
Literature:
- Beyer G, et al: S3-Leitlinie Pankreatitis – Guideline of the German Society for Gastroenterology, Digestive and Metabolic Diseases (DGVS). 2020; AWMF register number 021-003.
- “Acute and Chronic Pancreatitis,” Georg Beyer, MD, 128. Congress of the German Society for Internal Medicine, 03.05.2022.
- Banks PA, et al: Gut 2013; 62: 102-111.
- Nawaz H, et al: Am J Gastroenterol 2015; 110: 1497-1503.
- Lankish PG, et al: Int J Pancreatol 1999; 26: 55-57.
- Mounzer R, et al: Gastroenterology 2012; 142: 1476-1482.
- Kumar A, Chari ST, Vege SS: Pancreas 2014; 43: 1101-1110.
- Schepers NJ, et al. The Lancet 2020. doi: 10.1016/S0140-6736(20)30539-0.
- Bakker OJ, et al: Pancreatology 2014; DOI: 10.1016/j.pan.2014.07.008.
- Boxhoorn L, et al: New England Journal of Medicine. 2021 DOI: 10.1056/NEJMoa2100826.
- Nordback I, et al. Gastroenterology 2009; 136(3): 848-855.
- Sternby H, et al: Ann Surg 2019; 270: 348-355.
HAUSARZT PRAXIS 2022; 17(7): 34-35