Post-traumatic stress disorder is a delayed mental Reaction to an extremely stressful event or to an extraordinary Threat. There is a lack of strategies to overcome the experienced helplessness and the Loss of control to edit. The updated S3 guideline “Posttraumatic Stress Disorder (PTSD)” provides guidance for the treatment of this complex condition. complex clinical picture.
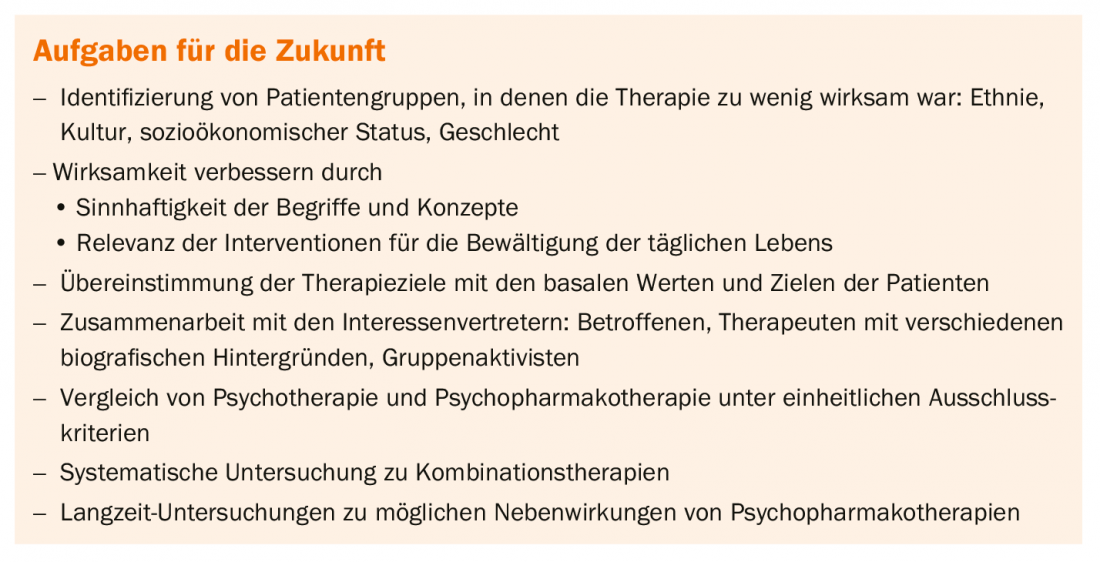
Post-traumatic stress disorder (PTSD) can develop as a result of a traumatic experience. More than half of all people are confronted with a traumatic experience at least once in the course of their lives. Whether they subsequently develop PTSD depends on the nature of the trauma. The risk of disease is particularly high after violent crime and war trauma. Up to one third of those affected develop PTSD in such a case. Natural disasters, fires, chemical or traffic accidents and acute physical illnesses also leave their mark. However, the risk for PTSD is significantly lower. Overall, about 10% of all trauma patients develop PTSD. The disease is characterized mainly by polarity of symptoms. Thus, symptomatology can occur both intrusive and constrictive (Table 1). The four main symptom clusters are intrusion, avoidance, negative cognition and disturbance of the level of arousal.
For the update of the S3 guideline, a systematic search of 8.19 studies and a selection of 288 relevant studies were performed in cooperation of four university working groups. Prof. Dr. med. Ingo Schäfer, Hamburg (D), gave a brief overview of the most important innovations regarding the psychotherapeutic treatment of PTSD. Thus, trauma-focused psychotherapy is treatment of first choice that should be offered to every patient with PTSD. The focus should be on processing the memory of the traumatic experience and/or its meaning. In addition, other problem and symptom areas should be clarified and taken into account in treatment, such as the risk of further victimization in victims of violence, mourning processes, social reorientation, re-evaluation and self-esteem stabilization. In addition, adjunctive procedures such as occupational therapy, art therapy, music therapy, physical and exercise therapy, or physical therapy may be offered as part of the trauma-specific, multimodal therapy regime. Although there is insufficient study evidence for this, there is positive clinical experience, as Schäfer explained. In contrast, potentially dangerous symptoms and behaviors, such as suicidality, psychotic symptoms, dissociative symptoms, self-injury, extraneous aggression, or substance use that result in serious behavioral control disorders, are a relative contraindication to a trauma-focused approach.
Possibilities and limits of pharmacological treatment
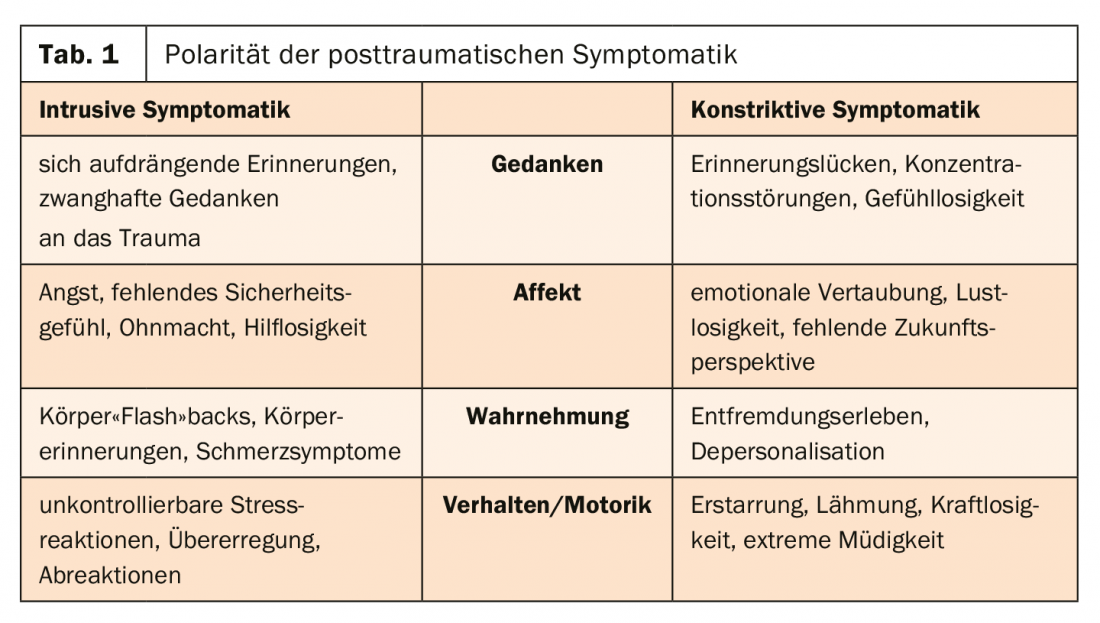
As Julia Schellong, MD, Dresden (D), explained, it is not always possible to predict at what point symptoms will respond to pharmacotherapy. For example, one study of venlafaxine showed that irritability improved as early as week two, but instrumental recall improved later at week four. On the other hand, the drug had no effect on sleep, dreaming, or avoidance symptoms, even after twelve weeks of treatment. Therefore, pharmacologic intervention must be tailored to individual needs. Basically, there are different target regions that are addressed with psychopharmacotherapy (Table 2) .
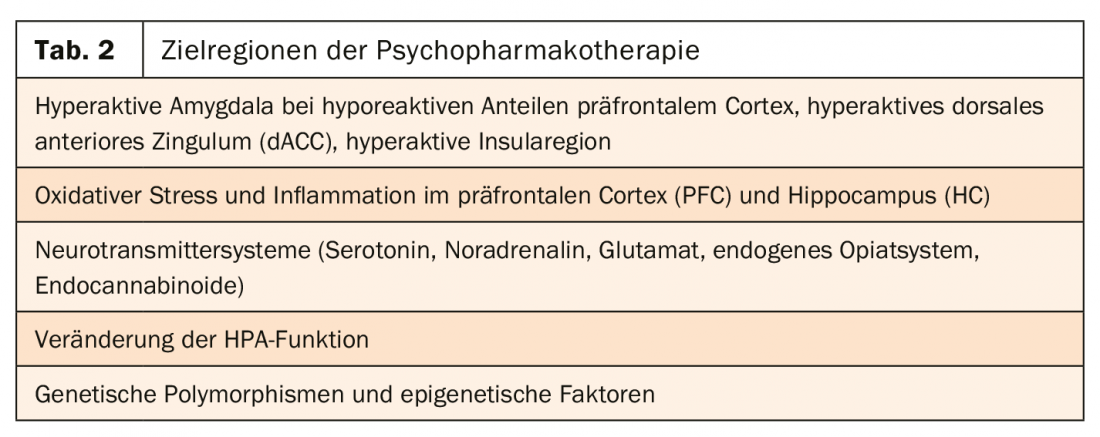
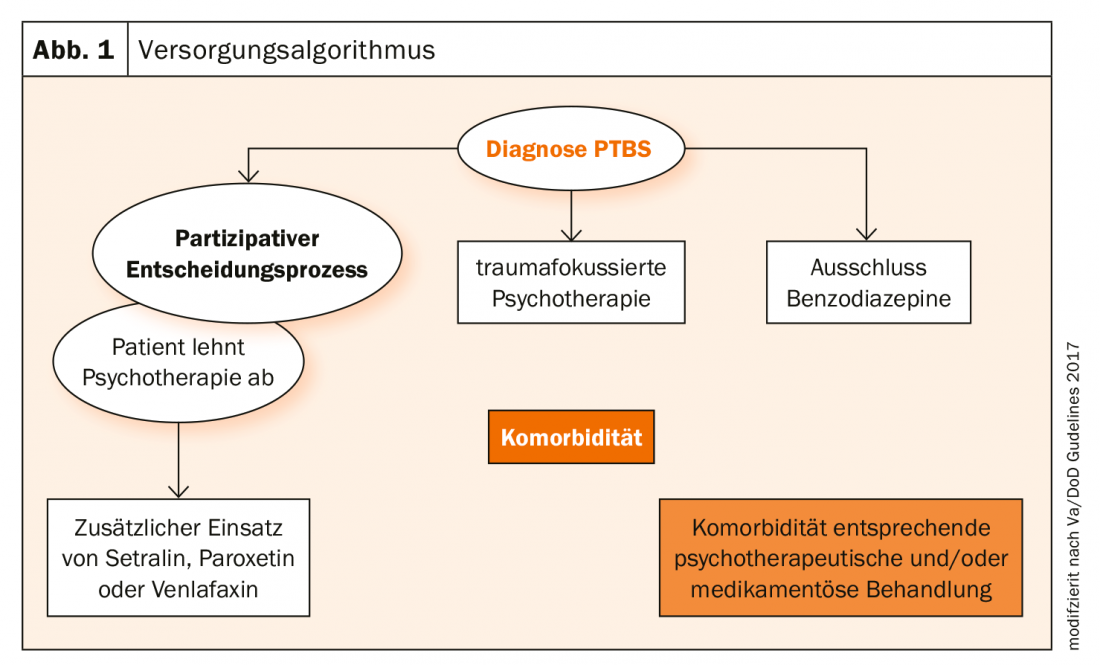
The goal is to improve symptoms and restore functionality. The current guideline indicates that psychopharmacotherapy should not be used as the sole or primary therapy for PTSD. If, after an informed and participatory decision-making process, medication is preferred despite the small effects, only setralin, paroxetine, or venlafaxine should be offered. Benzodiazepines, on the other hand, should not be used (Fig. 1).
Complex PTSD
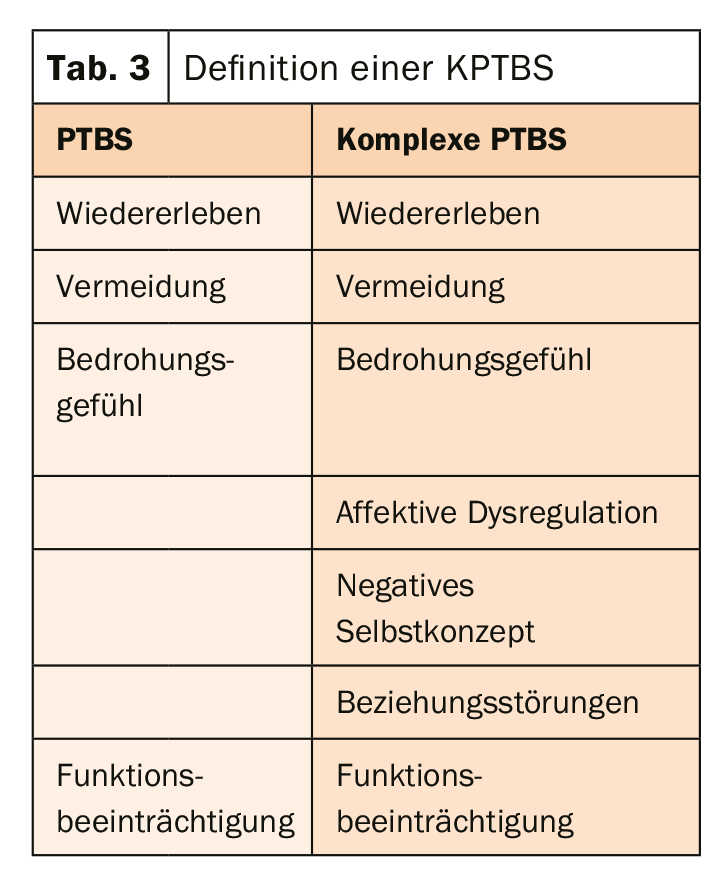
Prof. Dr. Dr. Andreas Maercker, Zurich, dealt with the question of whether PTSD and complex PTSD (KPTBS) are two different disorder patterns. In ICD-11, affective dysregulation, negative self-concept, and relationship disturbances are added to the symptoms of PTSD in KPTBS (Table 3). According to studies, the disorders seem to be associated with different levels of functional impairment and traumatic experiences. Moreover, a central problem of KPTBS seems to be the negative self-concept.
Basically, KPTBS therapy means a likely greater number of therapy components/techniques and/or a longer treatment time. Therefore, therapy should be done with a combination of trauma-focused techniques that focus on processing the memory of the traumatic experiences, processing the meaning of the traumatic experiences, and techniques for emotion regulation and improvement of relational dysfunction in terms of working through dysfunctional interpersonal patterns.
Guidelines – goals and benefits
Fundamentally, the goal of a guideline is to provide appropriate health-related care in specific clinical situations. For this purpose, systemtic statements are developed to support decision making. For this purpose, knowledge from different sources is compiled and evaluated. Opposing viewpoints are discussed and special requirements are revealed.
Level 3 guidelines are evidence-based. This means that a representative panel conducts a systematic search of all available studies and research. These are then evaluated and selected so that a structured consensus can be reached on this basis.It is important to note, however, that guidelines only serve as a decision-making aid and are not legally binding. Therefore, the doctor should always check the applicability individually.
Source: DGPPN 2019
InFo NEUROLOGY & PSYCHIATRY 2020; 18(1): 32-33 (published 1/26/20, ahead of print).