That vedolizumab in the maintenance treatment of IBD shows comparable efficacy when administered subcutaneously to intravenous administration has been demonstrated several times. Patients can thus carry out the treatment independently at home using a pre-filled syringe or pre-filled pen. At this year’s ECCO conference, new “real world” data were presented regarding the practicality and safety of switching from intravenous to subcutaneous modes of administration. The balance was very positive.
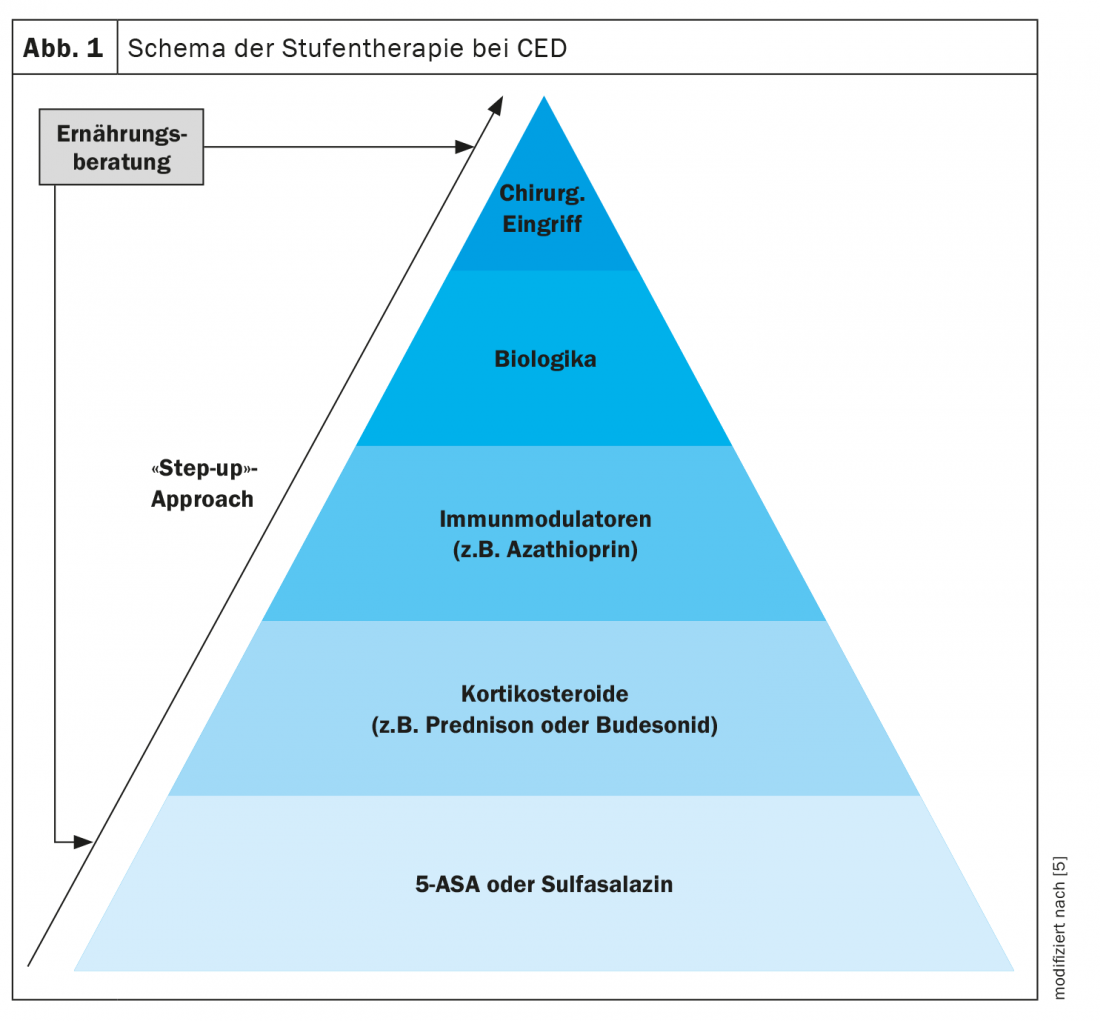
Treatment with conventional drugs such as aminosalicylates (5-ASA) or corticosteroids does not bring the desired success in all IBD patients. Approximately half of patients with Crohn’s disease (M. Crohn’s) and over one-third of those with ulcerative colitis (C. ulcerosa) are thought to require advanced intensified therapy with immunosuppressants, biologics, or “small molecules” [1]. This is particularly true for cases of IBD with extensive involvement, high disease activity, and refractory course [2]. In addition to various TNF-α inhibitors and the interleukin-12/23 antibody ustekinumab, the integrin antibody vedolizumab is also available in Switzerland from the group of biologics. Which biologic is appropriate for which patient must be decided on an individual basis [1]. The integrin blocker vedolizumab belongs to the new generation of biologics and is approved in Switzerland for the treatment of moderately to highly active Crohn’s disease and C. ulcerosa in patients for whom therapy with conventional drugs or TNF-α blockers was not effective. Integrins are proteins that act as adhesion molecules to enable a connection between two cells. The α4β7-integrin is located on the surface of memory T lymphocytes that migrate to the gastrointestinal tract and participate in inflammation characteristic of Crohn’s disease and ulcerative colitis. The mechanism of action of vedolizumab is that it specifically binds to the α4β7-integrin. This prevents the advance of the defense cells from the bloodstream into the intestinal tissue, so that the inflammation is counteracted. Vedolizumab can be administered as an infusion, as well as a subcutaneous injection. A subcutaneous injection can be self-injected by the patient after at least two infusions of vedolizumab. Here, the patient has the choice between a pre-filled syringe or a pre-filled pen.
Changeover of the application type proves to be practicable and safe
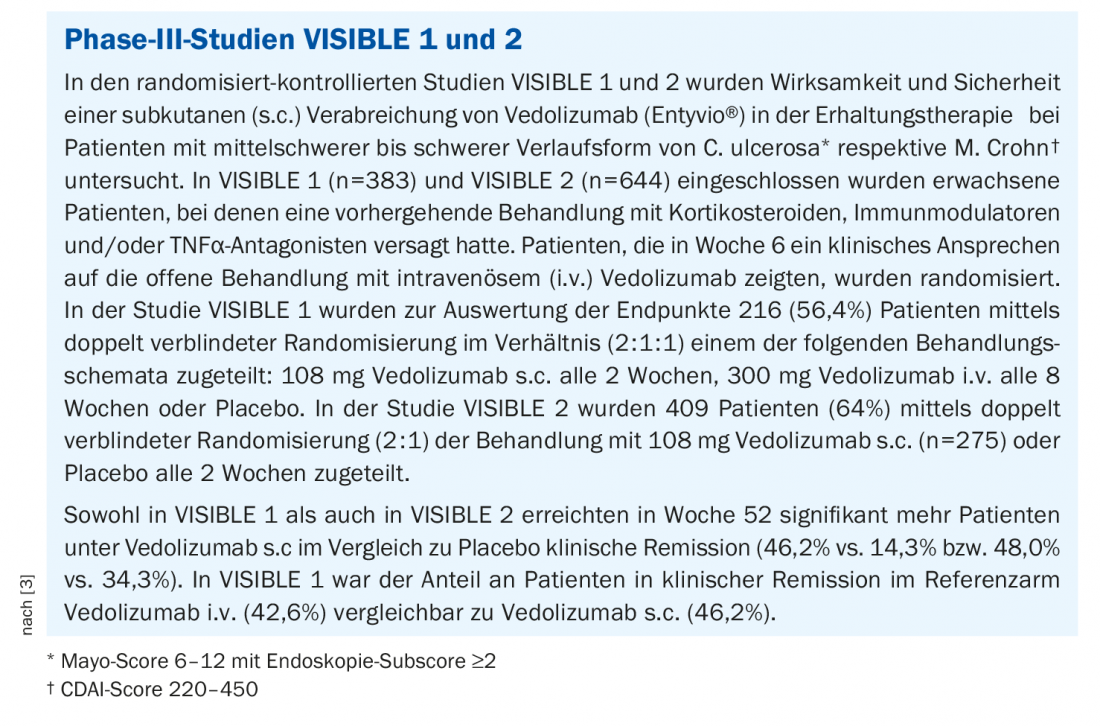
Approval of the subcutaneous route of administration is based on the VISIBLE 1-2 studies (box) [3]. The study by a Norwegian research team presented at this year’s virtual congress of the European Crohn’s and Colitis Organization (ECCO) shows that the switch from intravenous to subcutaneous administration of vedolizumab has proven itself in terms of practicability and safety in everyday practice [4]. CED patients who were on treatment with vedolizumab were identified from the medical record. Exclusion criteria for the study included treatment during the induction phase and a change in treatment regimen planned for the following three months or a surgical procedure planned during this period. The dosage of s.c. Vedolizumab was calculated based on current i.v. dose and injection interval. Treatment was evaluated at the time of the first and fourth injections and after three months. The primary endpoint was the percentage of patients who retained the s.c. form of administration after three months. Secondary endpoints included adverse events, disease activity (Harvey Bradshaw Index and Partial Mayo Score), C-reactive protein (CRP) and fecal calprotectin, and patient satisfaction with each route of administration.
A total of 51 patients with C. ulcerosa and 57 with M. Crohn’s completed a switch from intravenous to a subcutaneous dosage form of vedolizumab. After 3 months, 95.3% of the 108 study participants maintained s.c. treatment. No serious adverse events related to the change in route of administration occurred. The mean injection interval was 12 days. The plasma concentration of vedolizumab was 44.4 mg/l (interquartile range: 28.9-64.7 mg/l) after three months. In C. ulcerosa and Crohn’s disease patients, 92% and 72%, respectively, were in clinical remission at the time of the first injection, while the corresponding rates at three months were 88% (p=0.18) and 83% (p=0.11), respectively. No significant changes were observed with respect to CRP and fecal calprotectin. Before the switch, 25% of patients had indicated a preference for i.v. treatment, 28% favored the s.c. dosage form and 47% did not care. Three months after the completed switch, the corresponding rates were 18%, 53%, and 29%, respectively (p<0.001). Injection site reactions occurred in 19 (17.6%) of patients.
Overall, this “real world” study confirms that the switch from intravenous to subcutaneous administration of vedolizumab is feasible and safe in the maintenance treatment of IBD and that s.c. administration is an attractive alternative to i.v. administration. administration is an attractive alternative to i.v. administration. Data collection at the 3-month follow-up showed that there were no changes with the switch in terms of clinical remission rates, CRP, and fecal calprotectin. Patients were generally satisfied after the switch was made and favored the subcutaneous form of administration.
Congress: European Crohn’s and Colitis Organization
Literature:
- Bokemeyer B, et al: Inflammatory bowel disease: Tips for a differentiated biologic selection. Dtsch Arztebl 2021; 118(37): [4]; DOI: 10.3238. www.aerzteblatt.de/archiv/221197/
- Manthey CF, Reher D, Huber S: What is certain in the therapy of inflammatory bowel diseases. Internist 2021; 62: 1269-1279.
- Swissmedic: Medicinal product information, www.swissmedicinfo.ch, last accessed 18.03.2022
- Wiken T, et al: P376 Switching from intravenous to subcutaneous vedolizumab maintenance treatment; feasibility, safety and clinical outcome. Poster presentations: Clinical: Therapy and Observation 2022. 17th Congress of ECCO, February 16-19, 2022, Virtual.
- Edmonton Pediatric IBD Clinic, www.kidsibd.ca/ibd-treatments (last accessed Mar. 18, 2022).
HAUSARZT PRAXIS 2022; 17(4): 24-25











