Patients with ulcerative colitis and Crohn’s disease who undergo colonoscopies for surveillance significantly reduce the risk of dying from colorectal cancer. White light videoendoscopy (WLE) is still considered the standard, but other procedures have also become established. An expert from the Cantonal Hospital of St. Gallen provided information on the advantages and disadvantages of the various methods.
Chromoendoscopy (CE), in which (usually blue) dye is sprayed on, can enhance the contrast between normal and pathologically abnormal mucosa in this way, explained Prof. Jan Borovicka, M.D., Head of Department of Endoscopy, Clinic for Gastroenterology/Hepatology, Cantonal Hospital St. Gallen. However: a study published by the Swiss IBD Cohort Study Group led by Giulia Santi from the University of Lausanne in October 2020 [1] worked out that only 23 (7.4%) of 309 colonoscopies performed were done by chromoendoscopy. Even virtual chromoendoscopy, at 15.5%, is used by gastroenterologists far less frequently than one might think. Thus, despite current international recommendations, a significant number of patients do not receive adequate endoscopic monitoring, Prof. Borovicka points out. According to him, increased use of chromoendoscopy, monitoring of withdrawal time, and adequate bowel preparation would improve the quality of CRC screening. Adherence to screening guidelines and endoscopic quality should be promoted and standardized accordingly.
Biopsy: random or targeted?
A key question: are random biopsies still useful for detecting neoplasia in patients with IBD undergoing surveillance colonoscopy with chromoendoscopy? In a large study [2] of 1000 patients with IBD (495 with ulcerative colitis, 505 with Crohn’s disease) at risk of neoplasia, chromoendoscopy with targeted biopsies and endoscopic removal of resectable lesions detected most patients with neoplasia. The additional percentage of patients with neoplasms detected only by incidental biopsies was approximately 15%. The detection of neoplasia by random biopsies was associated with personal histology of neoplasia, concomitant primary sclerosing cholangitis (PSC), and a tubular colon. The likelihood of finding neoplasms through random biopsies is nearly zero in patients who lack these three risk factors – which accounts for the majority of patients, the expert said.
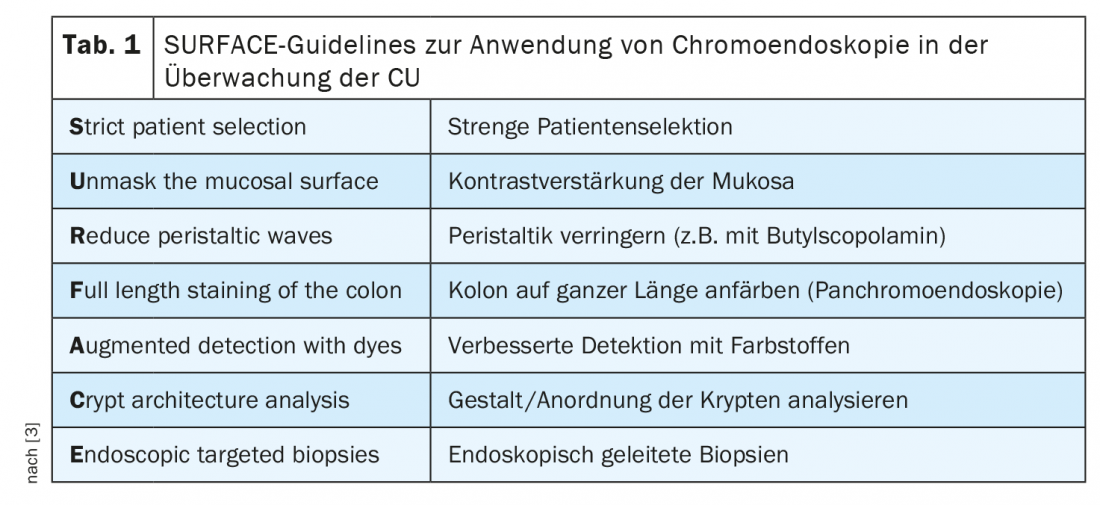
The majority of Swiss gastroenterologists do not resort to methylene blue or indigo carmine – the (probable) reason for skepticism: it takes time and is difficult to interpret. However, the SURFACE guidelines for the use of chromoendoscopy in ulcerative colitis (CU), which are still valid (Table 1), date back to 2004 and advised detection with dyes even then.
CE versus WLE
Despite advanced imaging techniques such as autofluorescence imaging (AFI), narrow band imaging (NBI), high-definition WLE, or CE, specialized endoscopists cannot reliably identify dysplastic lesions.
High-resolution chromoendoscopy may be superior to high-resolution white-light endoscopy in monitoring inflammatory bowel disease, but high-resolution white-light endoscopy is still the standard. This was also shown in a Swedish study [4] in which 305 patients with CU or Crohn’s disease underwent colonoscopy. Dysplastic lesions were detected in 17 patients with HD-CE and 7 patients with HD-WLE (p=0.032). 20% of these patients with dysplasia were identified only by analysis of random biopsies. 3 patients (33%) had PSC.
Therefore, the researchers concluded that HD chromoendoscopy was superior to HD white light endoscopy when both were performed with collection of incidental biopsies to detect dysplasia by colonoscopy. However, HD-WLE is still a good option as well, according to Prof. Borovicka. However, he also pointed out that because of the rare occurrence of dysplasia, studies with larger patient populations are needed to draw more valid conclusions.
Professional society recommends routine use
The expert concluded by referring to the European Society of Gastrointestinal Endoscopy (ESGE) recommendations for the detection and differentiation of colorectal neoplasms in inflammatory bowel disease, the latest version of which was published in 2019.
In it, ESGE recommends the routine use of dye-based pancreatic chromoendoscopy or virtual chromoendoscopy with targeted biopsies for neoplasia surveillance in patients with long-standing colitis when they are in a quiescent phase of disease (strong recommendation, moderate evidence). In contrast, random four-quadrant biopsy can be omitted in the setting of quiescent disease activity (strong recommendation, strong evidence).
The professional society also suggests that in high-risk patients with a personal history (colonic neoplasia, tubular colon, strictures, PSC), chromoendoscopically targeted biopsies can be combined with random four-quadrant biopsies every 10 cm in the colon, but there is only a weak recommendation and low evidence for this.
Take-Home Messages
- Colitis-associated cancers have a different pathogenesis than sporadic colorectal cancer.
- Targeted biopsies using only high-resolution colonoscopy are currently the technique of choice.
- Random biopsies should be added in patients with PSC, histology of colonic neoplasia, or tubular colon.
- Virtual chromoendoscopy has no added value to surveillance colonoscopy (no additional benefit over high-resolution white light alone or high-resolution chromoendoscopy).
Congress: IBDnetTalk, 03/17/2022
Literature:
- Santi G, Michetti P, Froehlich F, et al: Adherence to Recommendations and Quality of Endoscopic Colorectal Cancer Surveillance in Long-Standing Ulcerative Colitis. Inflamm Intest Dis 2021; 6: 25-31; doi: 10.1159/000511010.
- Moussata D, Allez M, Cazals-Hatem D, et al: Are random biopsies still useful for the detection of neoplasia in patients with IBD undergoing surveillance colonoscopy with chromoendoscopy? Gut 2018; 67(4): 616-624; doi: 10.1136/gutjnl-2016-311892.
- Rutter M, Bernstein C, Matsumoto T, et al: Endoscopic Appearance of Dysplasia in Ulcerative Colitis and the Role of Staining. Endoscopy 2004; 36(12): 1109-1114; doi: 10.1055/s-2004-826049.
- Alexandersson B, Hamad Y, Andreasson A, et al: High-Definition Chromoendoscopy Superior to High-Definition White-Light Endoscopy in Surveillance of Inflammatory Bowel Diseases in a Randomized Trial. Clin Gastroenterol Hepatol 2020; 18(9): 2101-2107; doi: 10.1016/j.cgh.2020.04.049.
HAUSARZT PRAXIS 2022; 17(5): 28-29