Contact allergic eczema is common. The main differential diagnosis is irritant contact dermatitis. However, especially on the hands, chronic contact eczema is often a combination of irritant and contact allergic eczema. The most common non-eczema manifestation of contact allergy is erythema multiforme-like contact dermatitis. The selection of test allergens should be guided by the medical history. Important allergens are nickel, cobalt, rubber ingredients, textile dyes, fragrances and epoxy resin. In addition, the preservative (chloro)methylisothiazolinone (MI), which is increasingly found in cosmetics, has led to a veritable epidemic of contact sensitization. Sensitization to para-phenylenediamine by so-called “black henna” tattoos is mainly found during vacations.
Contact allergic eczema is common and may account for up to 15% of inflammatory skin diseases of dermatologic patients. In terms of differential diagnosis, irritant contact eczema in particular must be differentiated, but there is a whole range of other differential diagnoses (Tab. 1).

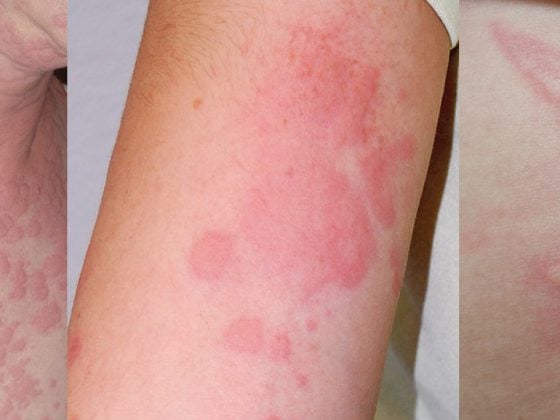
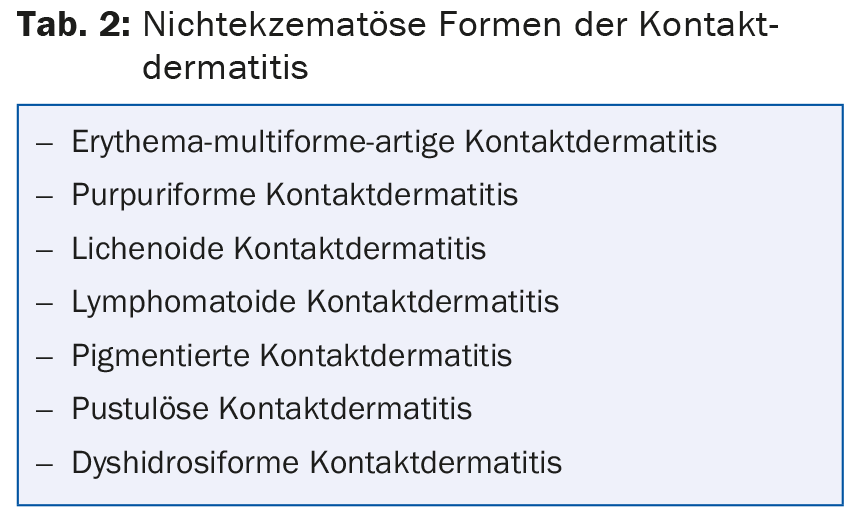
Chronic contact dermatitis is often a combination of irritant and contact allergic eczema, especially on the hands. In addition, it must also be taken into account that contact allergies can manifest themselves in a clinical form other than eczema (Tab. 2) .
The most common non-eczema manifestation of contact allergy in this context is erythema multiforme-like contact dermatitis (Fig. 1). But also in the case of eczema manifestations, the pattern recognition and thus the noxious agent that could be the trigger can be difficult to recognize, since the allergen can be transmitted aerogenically or from the partner, or dislocated only leads to the eczema (e.g. transferred from the hands to the eyelids).

Common and increasingly observed allergens
The selection of allergens to be tested should be guided by the medical history. Irrespective of this, testing of the standard series (Tab. 3) can frequently detect sensitization even in the case of an inconspicuous medical history.

Nickel, cobalt: The “allergen hit list” is still headed by nickel, although a decrease in sensitizations can be observed. However, the nickel content in jewelry and piercing materials still often exceeds the limits permitted by the EU directive, so that sensitization continues to occur, especially in younger patients. (Fig. 2). Also razors and – what may be surprising – even computer mice, laptops and cell phones can be sources of nickel, which have to be recorded anamnestically depending on the localization of the eczema.

Cobalt sensitization is also common and usually associated with nickel sensitization. However, in addition to such coupling allergy to metal salts from jewelry, cobalt can also be observed as an isolated allergen. The allergen sources can be colors and leather.
Fragrances: Among fragrances, oakmoss absolue, isoeugenol from fragrance mix I and hydroxyisohexyl 3-cyclohexene carboxaldehyde (HICC, Lyral) from fragrance mix II are common allergens that may be present in up to 30% of the cosmetics and household products tested.
(Chloro)Methylisothiazolinone: The preservative (chloro)methylisothiazolinone (MI) has been increasingly used in cosmetics, personal care and household products for several years and has led to a veritable epidemic of contact sensitization. MI can also be observed as an occupational toxin (Fig. 3) and then mainly affects beauticians and painters.

Epoxy resin: Epoxy resin sensitization is also of occupational relevance and is most common in the construction industry. Allergies can occur not only to the resins themselves, but also in isolation to the thinners and hardeners required, so these should always be tested as well if they are suspected.
Rubber ingredients: Contact sensitization to rubber ingredients is also frequently found. Among these, thiuram sensitizations are most common, followed by dithiocarbamate and mercaptobenzothiazole. These allergies can be particularly problematic with protective gloves, even if they are latex-free.
Textile dyes: Textile dyes show sensitization frequencies of >1%, so that epicutaneous testing of these dyes should be considered in persistent or chronically recurrent eczema of unclear etiology, especially on the trunk. Affected patients should avoid synthetic textiles, as these are more frequently treated with correspondingly allergenic (azo) dyes than textiles made from natural fibers.
Para-phenylenediamine: Sensitization to para-phenylenediamine by so-called “black henna” tattoos represents an unbroken trend of contact sensitization acquired during vacations (Fig. 4) . This sensitization makes subsequent darkening of the hair (e.g. with dyes containing toluylenediamine) and employment in the hairdressing profession impossible. The supposedly harmless, because only painted on “temporary tattoos”, which are offered worldwide on vacation beaches, but occasionally also in hotels or at the hairdresser, should be absolutely avoided.

Further reading:
- Geier J, et al: Current contact allergens. Dermatologist 2011; 62: 751-756.
- Skudlik C, Geier J, John SM: Current trends in occupational dermatology. Dermatologist 2014; 65: 983-995.
- Brasch J, et al: Guideline contact dermatitis. Allergo J Int 2014; 23: 131.
- Richardson C, et al: Mobile Phone Dermatitis in Children and Adults: A Review of the literature. Pediatric Allergy, Immunology and Pulmonology 2014; 27: 60-68.
- Uter W, et al: Contact sensitization to cobalt–multifactorial analysis of risk factors based on long-term data of the Information Network of Departments of Dermatology. Contact Dermatitis 2014; 71: 326-337.
- Läuchli S, Lautenschlager S: Contact dermatitis after temporary henna tattoos – an increasing phenomenon. Swiss Med Wkly 2001; 131: 199-202.
- Kind F, Scherer K, Bircher AJ: Contact dermatitis to para-phenylenediamine in hair dye following sensitization to black henna tattoos – an ongoing problem. JDDG 2012; 10: 572-578.
DERMATOLOGIE PRAXIS 2015; 25(2): 6-8