Patients with stable coronary artery disease (CAD) and indication for revascularization have a survival advantage after coronary bypass surgery. Primarily, arterial grafts should be used for revascularization. In patients with stable CHD, there is still no evidence for superiority in terms of mortality reduction with a combination of percutaneous intervention (PCI) and optimal drug therapy versus optimal drug therapy alone. In stable situation and complex coronary anatomy, ad hoc PCI should not be performed without adequate cardiac functional diagnosis and patient education. There should always be an interdisciplinary evaluation. Patients should be evaluated not only by scoring systems but also by history, physical examination (general condition), and attention to additional diseases not included in the primary scoring system.
Cardiovascular disease remains the leading cause of death in the Western world. This includes ischemic heart disease, most commonly caused by coronary artery disease (CAD) with artherosclerotic changes in the coronary arteries. Briefly summarized, this is divided into a stable and unstable form.
The unstable form includes acute coronary syndrome (ACS, myocardial infarction with or without ST elevation on ECG). Stable CHD is typically due to a hard, collagen-rich plaque that leads to reversible stable angina starting at about 70% luminal constriction under conditions of increased oxygen demand. In contrast, in ACS, blood flow is critically reduced by rupture of lipid-rich soft plaques in the presence of the highest-grade stenoses or acute occlusions. Also, patients with ACS regularly show fewer affected vessels with fewer stenoses and occlusions, thus poorer collateralization [1]. According to the different initial situation, the therapy recommendations are also different.
Currently still no survival benefit with PTCA compared to drugs
In patients with ACS, it is generally accepted that coronary revascularization reduces the risk of death and myocardial infarction [2]. In patients with stable CHD requiring intervention, it has been shown to date that there is generally a clear survival advantage for these patients after aortocoronary bypass (ACB) surgery [3].In ACB surgery, arterial grafts are primarily used for revascularization, and the internal mammary artery should be harvested skeletally [4,5]. In multivessel disease, complete surgical revascularization is superior to surgical revascularization of only the culprit artery in terms of overall survival and time to reintervention [6].
Percutaneous transluminal coronary angioplasty (PTCA) with stenting currently fails to achieve a significant survival benefit compared with drug treatment [7]. The results of the COURAGE and BARI 2D trials showed that patients with stable CHD and comparable atherosclerotic and ischemic burden had a similar risk of death and myocardial infarction after PTCA and stenting and optimal drug therapy compared with optimal drug therapy alone [8,9]. This may change with the use of the latest coated stents, but no conclusive long-term results are yet available [10]. The fact that the symptoms of CHD can be improved by PTCA and that this also improves the quality of life was confirmed, among others, by the RITA-2 study [11,12].
New ISCHEMIA study
In all previous studies, patients with stable CHD were assigned to the different therapy groups only after diagnostic cardiac catheterization. Therefore, a global clinical trial (ISCHEMIA) has now been launched that will enroll 8000 patients in 400 centers [13]. In this study, for the first time, patients with stable CHD will be randomized to one of the groups prior to cardiac catheterization in order to evaluate the optimal therapy (“drug + stent” versus “drug alone”).
Current guidelines
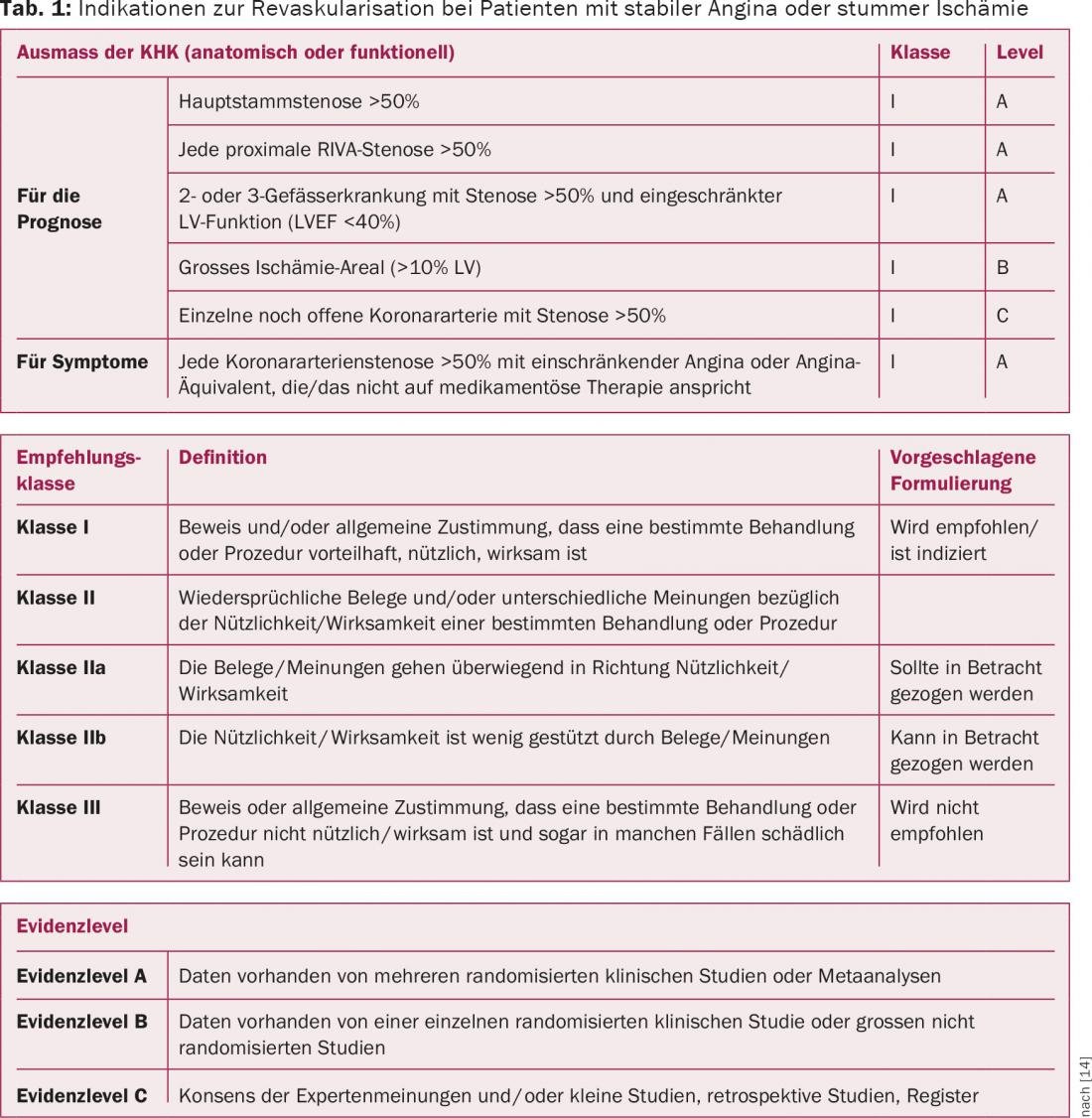
The current 2014 European guidelines recommend myocardial revascularization for patients with stable CAD if they remain symptomatic despite optimal medical therapy and have greater than 50% coronary artery stenosis (Table 1) [14]. Furthermore, revascularization is recommended in asymptomatic patients to improve prognosis if they have main stem or proximal RIVA (R. interventricularis anterior) stenosis greater than 50%, two- or three-vessel disease with stenosis greater than 50% and concomitant LVEF less than 40%, a single patent coronary artery with greater than 50% stenosis, or a large area of ischemia greater than 10% of the left ventricle.
When is ad hoc PCI indicated?
Although the indications for coronary revascularization thus seem clear, the type of revascularization can be debated. In stable CHD, the diagnosis is currently confirmed predominantly by coronary angiography. If an intervention, so-called ad hoc PCI, is performed simultaneously during this diagnostic angiography, this is only justified after prior adequate information of the patient and complete cardiac diagnostics including functional testing of the heart (possibly stress tests, possibly measurement of fractional flow reserve in moderate coronary stenoses, viability diagnostics in poor left ventricular function) [14].
Patients with stable CHD and complex coronary pathology, including main stem lesions or proximal RIVA stenosis and coronary three-vessel disease, should not usually be treated ad hoc but should be discussed first by the HeartTeam. At a minimum, the HeartTeam should include interventional cardiologists, cardiac surgeons, and noninterventional cardiologists [14].
In contrast, in the acute situation, ad hoc intervention of the culprit lesion is indicated without prior HeartTeam discussion; appropriate parameters include progressive ischemia, hemodynamic instability, pulmonary edema, recurrent ventricular arrhythmia, or complete occlusion of the causative coronary artery.
SYNTAX score and EuroSCORE
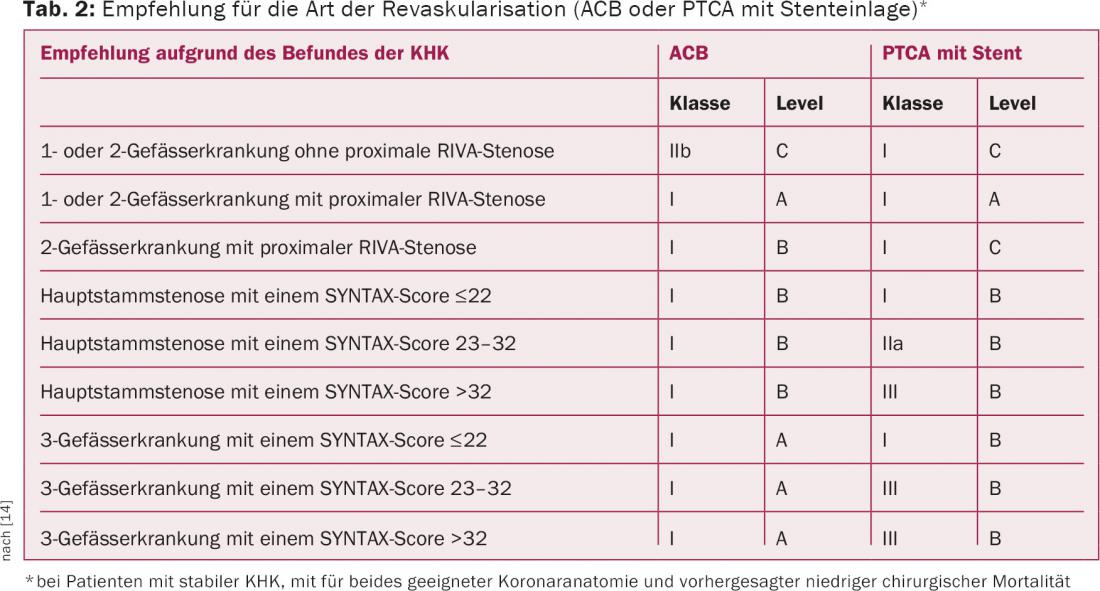
Depending on the findings of coronary angiography, there is subsequently a clear indication for surgery for stable CAD in the presence of high-grade proximal RIVA stenosis, main-stem stenosis, or three-vessel disease and concomitant low surgical risk (Table 2). For PTCA, the so-called SYNTAX score is available [15]. It can be used to predict long-term mortality in patients with complex three-vessel disease or left main stem stenosis. The SYNTAX score is composed of a combination of anatomic features of the coronary vessels and assesses the complexity of the CAD. A SYNTAX score >22 favors ACB surgery, and a SYNTAX score ≤22 favors PTCA. This includes single- or branch-vessel disease with or without proximal RIVA stenosis, main-stem stenosis with low SYNTAX score, and three-vessel disease with low SYNTAX score as guideline-appropriate indications (Table 2) [14]. To determine the surgical risk in ACB surgery, the EuroSCORE II is mainly used in Europe [16].
Therapy decision: more than score assessment
However, these scores can only be used to assess the statistical risk, but cannot predict the actual future events that will occur in the individual patient. Indispensable is the assessment of the overall situation, the general condition with direct evaluation of the patient by history and physical examination, and the joint evaluation of additional diseases that are not included in the primary scoring system.
Considering the benefit-risk ratios, the treatment decision should be made with weighting of the potential risks for the patient: These include periprocedural death, myocardial infarction, stroke, quality of life and long-term survival, and repeat revascularization. Other important criteria include coronary anatomy, age, existing concomitant diseases and conditions as well as patient opinion and preference. There must be an ethical requirement to inform the patient in an unbiased, transparent and comprehensive manner about different and alternative therapy options with their advantages and disadvantages, and to give the patient sufficient time to make a decision (several days between diagnosis and therapy).
Literature:
- Agewall S: Acute and stable coronary heart disease: different risk factors. Eur Heart J 2008; 29: 1927-1929.
- Fox KA, et al: Long-term outcome of a routine versus selective invasive strategy in patients with non-ST-segment elevation acute coronary syndrome a meta-analysis of individual patient data. Am J Coll Cardiol 2010; 55: 2435-2445.
- Yusuf S, et al: Effect of coronary artery bypass graft surgery on survival: overview of 10-year results from randomised trials by the Coronary Artery Bypass Graft Surgery Trialists Collaboration. Lancet 1994; 344: 563-570.
- Locker C, et al: Multiple arterial grafts improve late survival of patients undergoing coronary artery bypass graft surgery. Circulation 2012; 126: 1023-1030.
- Ali E, et al: Does a skeletonized or pedicled left internal thoracic artery give the best graft patency? Interact Cardiovasc Thorac Surg 2010; 10(1): 97-104.
- Habib RH, et al: CABG versus PCI. J Am Coll Cardiol 2015; 66(13): 1417-1427.
- Stergiopoulos K, et al: Initial coronary stent implantation with medical therapy vs medical therapy alone for stable coronary artery disease: meta-analysis of randomized controlled trials. Arch Intern Med 2012; 172: 312-319.
- Boden WE, et al: Optimal Medical Therapy with or without PCI for Stable coronary Disease. N Engl J Med 2007; 356: 1503-1516.
- Chaitman BR, et al: The bypass angioplasty revascularization investigation 2 diabetes randomized trial of different treatment strategies in type 2 diabetes mellitus with stable ischemic heart disease: impact of treatment strategy on cardiac mortality and myocardial infarction. Circulation 2009; 120(25): 2529-2540.
- Hlatky MA, et al: Impact of drug-eluting stents on the comparative effectiveness of coronary artery bypass surgery and percutaneous coronary intervention. Am Heart J 2015; 169(1): 149-154.
- Henderson RA, et al: Seven-year outcome in the RITA-2 trial: coronary angioplasty versus medical therapy. J Am Coll Cardiol 2003; 42(7): 1161-1170.
- Pocock SJ, et al: Quality of life after coronary angioplasty or continued medical treatment for angina: three year follow-up in the RITA-2 trial. Randomized Intervention Treatment of Angina. J Am Coll Cardiol 2000; 35(4): 907-914.
- www.ischemiatrial.org
- Windecker S, et al: 2014 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J 2014; 35: 2541-2619.
- Mohr FW, et al: Coronary artery bypass graft surgery vs. percutaneous coronary intervention in patients with 3-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet 2013; 381(9867): 629-638. www.syntaxscore.com
- Nashef SA, et al: EuroSCORE II. Eur J Cardiothorac Surg 2012; 41(4): 734-744.
CARDIOVASC 2015; 14(6): 9-13











