The classification criteria for the widespread disease diabetes have changed again and again over the years. Since 2000, immune-mediated type 1 forms have been distinguished from type 2 forms, which are caused by insulin resistance, decreased insulin secretion, or chronic inflammation. At this year’s Medidays, Prof. Roger Lehmann, MD, Zurich, focused on the intermediate LADA type and the MODY subtypes.
(ag) Prof. Roger Lehmann, MD, Senior Physician at the University Hospital Zurich, opened his presentation with epidemiological data: “Diabetes mellitus is a worldwide problem: 371 million suffered from it in 2012, and by 2030 it will be 552 million. The number of patients with diabetes is increasing in every country, yet a good 80% of them live in low- and middle-income countries. Half of all cases are also underdiagnosed, meaning these people don’t even know they have diabetes.” Correct diagnosis becomes very relevant from this point of view. It should be done according to the following steps:
- The patient has symptoms of diabetes or is at increased risk of developing it.
- HbA1c must be measured by internationally standardized method.
- If the value is ≥6.5%, the diagnosis is diabetes mellitus, which must be treated according to guidelines.
- If the value is <5.7%, diabetes can be excluded.
- If the value is between 5.7% and 6.4%, fasting glucose (NPG) must also be measured or an oral glucose tolerance test (OGTT) performed.
- If NPG ≥7.0 and/or 2h OGTT ≥11.1, the diagnosis is diabetes mellitus; if NPG <5.6 and/or 2h OGTT <7.8, this can be excluded.
- Difficult cases are those that have values between NPG 5.6 and 6.9 and/or 2h OGTT between 7.8 and 11.0. Education about diabetes risk is needed here, as well as counseling on lifestyle interventions. The most important risk factors should be treated and a new site assessment should be performed in the following year [1].
“When measuring HbA1c, it is important to know that the contribution of a previous glycemia to the current HbA1c is 50% in the first month, 25% in the second, and also 25% in the third and fourth. That is, the last month determines half of the current HbA1c,” Prof. Lehmann explained. “Conversion to average blood glucose is based on a simple calculation: HbA1c = (glucose + 2.6)/1.6 or glucose = (HbA1c × 1.6) – 2.6.”
Studies on the progression of diabetes also show that fasting glucose increases two, whereas postprandial glucose increases six years before diabetes diagnosis [2]. Thus, postprandial glucose is significantly more sensitive than fasting glucose.
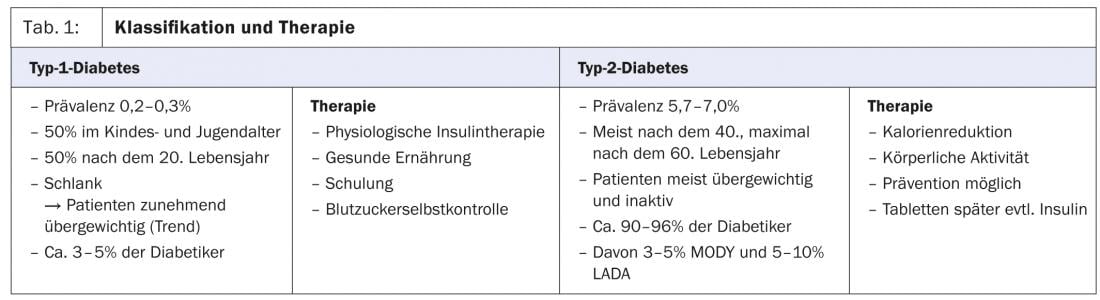
LADA as an intermediate type
In the 1970s, diabetes was still classified according to age: Juvenile and adult-onset diabetes. This classification soon turned out to be inaccurate. This was followed by the classification into insulin-dependent (IDDM) and insulin-independent diabetes mellitus (NIDDM), which was superseded in 2000 by the classification according to the type of pathogenesis: Type 1 diabetes as an immune-mediated disease, Type 2 as a form caused by insulin resistance, decreased insulin secretion or else chronic inflammation. (Table 1). Latent autoimmune diabetes in adulthood (LADA diabetes) is considered an intermediate type. It presents clinically like type 2 diabetes, but is often slightly leaner and shows a higher HbA1c at diagnosis. It is diagnosed by measuring GAD antibodies (as in type 1 diabetes). There is a more rapid insulin dependence than in type 2 and sulfonylureas tend to be unfavorable in therapy. Insulin is used as a first-line agent. Often this form remains undetected and is treated like type 2 diabetes.
MODY
Maturity-Onset Diabetes of the Young (MODY), with its many subtypes, is one of the specific types of diabetes. “A very simple rule of thumb for practice is that if the patient is under 25 and one parent has diabetes, it’s a MODY,” explains Prof. Lehmann. This is a heterogeneous disorder caused by a heterozygous monogenic mutation in at least eleven different genes. Diabetes begins early in life, usually in childhood, adolescence, or as a young adult, but in any case before age 25. Inheritance is autosomal dominant. Except for MODY 2, each is a primary defect of insulin secretion. 3-5% of all so-called “type 2 diabetics” are affected. Frequent and therefore important for the general practitioner are mainly the subtypes MODY 1, 2 and 3. 80% of the cases are MODY 2 or 3, only 5% MODY 1.
“MODY 2 is often overlooked. It occurs in childhood or already during pregnancy. It is an elevated fasting glucose, complications are rare. MODY 3, on the other hand, shows up more often postpubertally and responds particularly well to sulfonylureas, and later to insulin. It is a diabetes that can be associated with microvascular complications and glucosuria,” says Prof. Lehmann.
Gestational diabetes
This form of diabetes is defined by glucose intolerance, which is first discovered during pregnancy. The definition is independent of whether therapy is with insulin or diet, or whether the condition persists after pregnancy. It does not rule out the possibility of preexisting glucose intolerance or diabetes. Because of the increase in women of childbearing age with type 2 diabetes, it is reasonable to screen women who have risk factors for diabetes for diabetes at the first pregnancy visit using commonly used diagnostic criteria. Women who have diabetes are labeled “diabetes in pregnancy” rather than “gestational diabetes.”
To consider
1. in adults and atypical type 2 diabetes, type 1 diabetes should also be considered (antibody measurement, acetone).
- Therapy with insulin
2. if there are abnormalities in family history or particularly mild hyperglycemia, MODY or mitochondrial diabetes should be considered.
- Therapy via sulfonylureas (MODY 1 and 3)
- Therapy with insulin in mitochondrial diabetes
Source: “Diabetes Update”, Seminar at Medidays, September 2-6, 2013, Zurich.
Literature:
- Kerner W, Brückel J: Definition, classification and diagnosis. Diabetology 2010; 5: 109-112.
- Tabák AG, et al: Trajectories of glycaemia, insulin sensitivity, and insulin secretion before diagnosis of type 2 diabetes: an analysis from the Whitehall II study. Lancet 2009 Jun 27; 373(9682): 2215-21. doi: 10.1016/S0140-6736(09)60619-X. Epub 2009 Jun 8.
HAUSARZT PRAXIS 2013; 8(11): 35-37
CONGRESS SPECIAL 2014; 6(1): 26-29