In etiological terms, rheumatism is not a uniform clinical picture, but means nothing other than pain and functional impairment of the musculoskeletal system. Before diagnosing a chronic pain syndrome of the musculoskeletal system/fibromyalgia syndrome, it is imperative that the so-called “pain tests” are carried out. “red flags” are excluded. In the therapy of soft tissue rheumatic pain syndrome (FMS), improving physical fitness/general condition through adapted exercise training is the most likely therapeutic measure to be recommended. For inflammatory rheumatic diseases, the earlier the diagnosis is made and efficient treatment is initiated, the better the prognosis.
Pain represents the central symptom in patients with rheumatic disease patterns. Numerous studies have shown that pain is the most distressing problem. Pain and rheumatism therefore belong closely together. In etiological terms, rheumatism is not a uniform clinical picture, but means nothing other than pain and functional impairment of the musculoskeletal system. Rheumatism therefore has many different causes (Table 1).

Pain
Pain can be acute, subacute, or chronic. Chronic pain is defined as pain lasting more than six months.
Acute pain is usually receptor pain (neuroceptive pain), i.e., pain that is conducted from a peripheral organ to the center as a warning signal. Neuropathic pain is usually chronic pain and results from damage to sensorimotor structures in the peripheral and central nervous system, e.g., in root compression, spinal cord injury, bottleneck syndromes, postherpetic neuralgia/polyneuropathy, cerebral infarction, etc. Increasingly, so-called mixed pain syndromes are observed, including chronic back pain and other chronic pain syndromes of the musculoskeletal system. While acute pain has a protective and meaningful role, chronic pain is increasingly becoming a pain disorder that is no longer meaningful in the true sense of the word, with massive impairment of quality of life and functionality.
Pain syndromes in degenerative rheumatic diseases
Degenerative changes occur both in the peripheral joints (arthroses) and in the spine (osteochondrosis, spondylarthrosis, spinal canal and foraminal stenosis, root cysts, etc.). In the case of arthrosis, the pain can originate from the joint space itself, but it can also frequently arise extraarticularly, i.e., originating from periarticular structures as in insertion tendinosis/tendinopathy, bursitis, periostitis, etc. Periarthropathy syndromes can occur in practically any joint, most frequently affecting the shoulder, elbow, hip, and knee joints.
It is even more difficult to assign the development of pain in the spine to a specific structure. The cause of pain may be due to the disc itself (e.g., annulus tear, discopathy), but also to compression of neural structures (disc herniation, spinal stenosis, foraminal stenosis) or myelocompression.
Soft tissue rheumatic pain syndromes
Soft tissue rheumatism can be localized, as in sports or work overload (epicondylopathy, neck strains, periarthropathies, etc.), or it can occur as generalized soft tissue rheumatic pain syndrome/fibromyalgia syndrome proper. While the cause of localized soft tissue rheumatic pain is usually known, generalized soft tissue rheumatic pain syndrome, the cause of which is still largely obscure, presents an increasing challenge in both diagnosis and treatment. Additional factors (so-called risk factors) play an important role, such as
- Psychosocial stress situation
- Psychiatric comorbidity
- Job dissatisfaction/heavy work/low education level
- Stress processing disorder, etc.
Generalized soft tissue rheumatic pain syndrome is one of the most common chronic pain syndromes in rheumatology, along with chronic low back pain. These are:
- Somatoform pain disorder (ICD-10)
- Somatization disorder (F45.0)
- Persistent somatoform pain disorder (F45.4).
In these chronic pain syndromes, the following “red flags” are important for making the diagnosis: age over 80 years or under 20 years, history of malignancy, general condition deterioration, pathological laboratory findings, weight loss. These “red flags” must be considered in any case before diagnosing a chronic musculoskeletal pain syndrome.
While until recently the search for and definition of so-called painful fibromyalgia pressure points was required for the diagnosis of fibromyalgia syndrome, the definition has shifted in recent years in the sense that the following points are newly defined for the purpose of diagnosis:
- Increased pressured dolence/diffuse painfulness of soft tissues (allodynia)/lowered pain threshold
- Psychological comorbidities/cognitive symptoms
- Vegetative accompanying symptoms such as irritable bladder, irritable bowel, dizziness, etc.
- Non-restorative sleep/daytime sleepiness (fatigue)
- Exclusion of a tangible cause of the complaints.
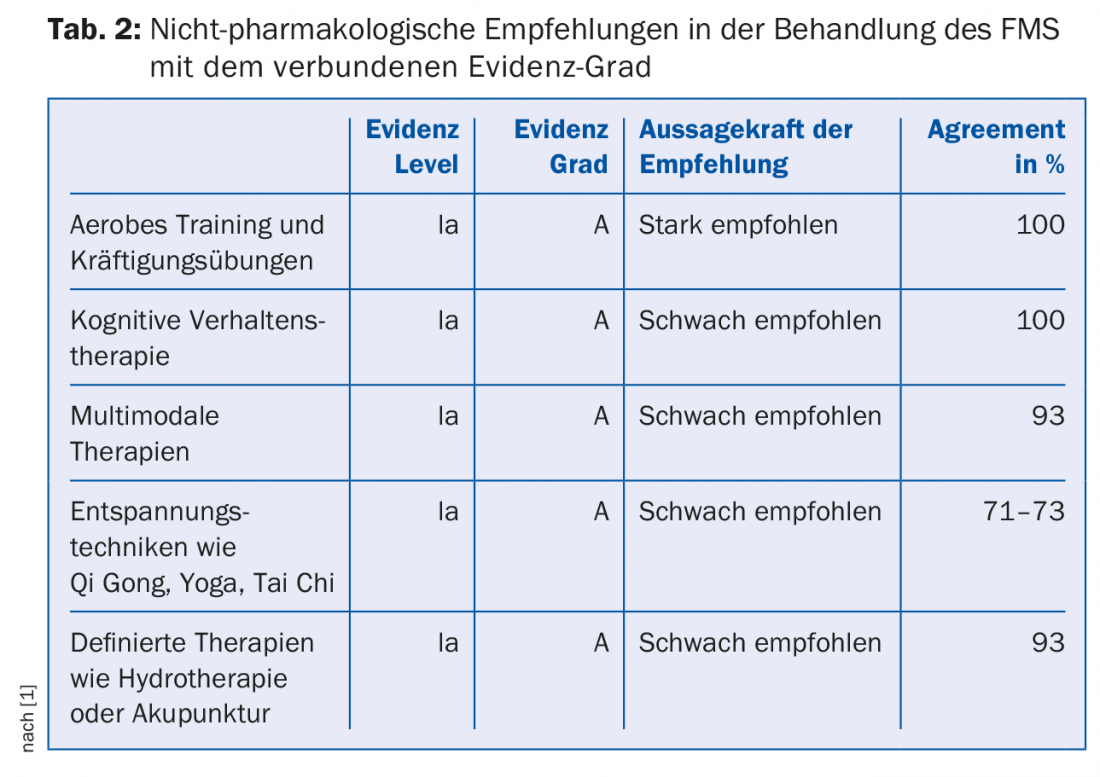
Since the cause of chronic musculoskeletal pain syndromes is still largely unknown, their treatment is also difficult and poses a challenge to any therapist. According to recent studies, one of the few significantly effective therapeutic measures is the improvement of general condition/fitness through adapted exercise training, which can have a positive influence on this disease (Tab. 2).
With regard to drug therapies, there has not yet been a clear correlation with efficacy, i.e., a significant influence on symptoms (tab. 3).

Inflammatory rheumatic diseases
These include primarily rheumatoid polyarthritis, ankylosing spondylitis (sero-negative spondyloarthropathies), and collagenoses (lupus erythematosus disseminatus, systemic sclerosis, Wegener’s disease, and other less common collagenoses). In these inflammatory rheumatic systemic diseases, pain is caused by the inflamed joints and soft tissues in which the antigen-antibody reaction takes place, as well as by the involvement of the connective tissue structures and, in more severe cases, the internal organs. These diseases are now quite well researched. In the last 20 years, with biologicals (TNFα inhibitors, B-cell depletors, interleukin antibodies), groundbreaking new treatment strategies have emerged alongside DMARDs that have been available for some time (methotrexate, Salazopyrin® etc.). Pain can usually be positively influenced by combating the inflammation, i.e. the underlying disease, as early as possible. Unfortunately, despite the most modern therapy methods, a full remission is not always achieved and it can lead to recurrent attacks of the disease and thus to pain. Moreover, in many patients chronic changes have already occurred by then, which can be the cause of chronic pain.
Metabolic diseases
These include first and foremost the crystal arthropathies such as.
- Gouty arthropathy
- Chondrocalcinosis (calcium-phosphate deposits)
- Hydroxyapatite deposits.
Another metabolic disease is osteoporosis, which has become massively more important in the last 30 years as the population has aged. In the case of metabolic diseases, the cause of the disease must be treated first and foremost. In osteoporosis, secondary pain can result from deformation and collapse of vertebral bodies, which can lead to chronic back pain. In the treatment of osteoporosis, very potent drugs and surgical treatment strategies (vertebroplasty, kyphoplasty) are now available. Early diagnosis and initiation of therapy is also important here in order to prevent late consequences and thus chronic pain and functional deficits up to immobility.
Literature:
- Macfarlane GJ, et al: EULAR revised recommendations for the management of fibromyalgia. Annals of the Rheumatic Diseases 2017; 76: 318-328.
Further reading:
- Affleck G, et al: Sequential daily relations of sleep, pain intensity, and attention to pain among women with fibromyalgia. Pain 1996; 68: 363-368.
- Benett R: Shining a light on fibromyalgia treatment. Nature Rev 2016; 12: 568-569.
- Edinger J, et al.: Can CBT for insomnia also improve pain sensitivity in fibromyalgia patients? Results from a randomized clinical trail. Sleep Medicine 2013; 14, e213. DOI: 10.10.16/j.sleep.2013.11.509.
- Egle UT, Ecker-Egle ML, Nickel R: Fibromyalgia syndrome-a stress processing disorder. Swiss Archives Neurol & Psych 2011; 162(8): 326-337.
- Gerdle B, et al: Increased interstitial concentrations of glutamate and pyruvate in vastus laterlis of women with fibromyalgia syndrome are normalized after an exercise intervention – a case-control study. PLoS One 2016 Oct 3; 11(10): e0162010. DOI: 10.1371/journal.pone.0162010.
- Koroschetz J, Baron R: Neuropathic pain – causes and therapeutic approaches. Rheumatology Act 2010; 35: 164-171.
- Merker M, et al: [Undesired side effects of tapentadol in comparison to oxycodone. A meta-analysis of randomized controlled comparative studies]. Pain 2012 Feb; 26(1): 16-26.
- Pierer M, et al: Opioids in musculoskeletal pain. Act Rheumatol 2010; 35: 184-188.
- Smythe HA: “Fibrositis” as a disorder of pain modulation. Clin Rheum Dis 1979; 5: 823-832.
HAUSARZT PRAXIS 2017; 12(3): 16-19