Based on declining case numbers, health officials have relaxed “lockdown” measures. This raises questions about the extent to which protective measures are required and how the situation will develop in the coming months. Experts from the fields of infectiology, virology and epidemology assess the current situation and provide advice.
Protection in the health care system and in the population is central. “It’s the only thing we can currently use against SARS-CoV-2 with documented efficacy,” said Prof. Andreas Widmer, MD, dept. Head of the Department of Infectious Diseases & Hospital Hygiene at the University Hospital Basel and President of the National Center for Infection Prevention [1]. These include masks, hand disinfection and gloves. Unfortunately, about 50% of infections occur before the onset of the disease, which means that these measures must be used consistently when people feel healthy in order to achieve maximum effect.
Protective masks are more important than ever
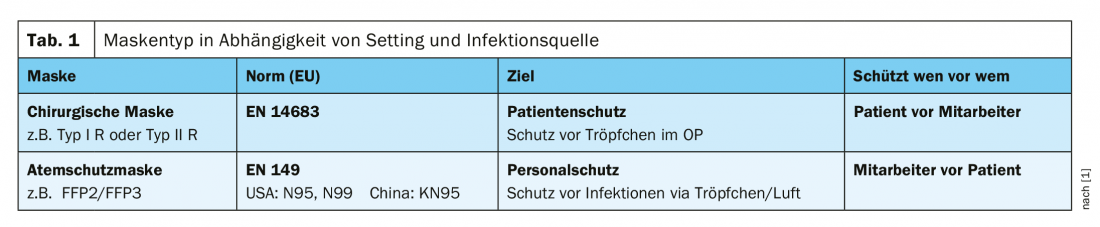
There are very many different mask types, the quality certified ones in Europe are surgical masks and FFP2/3 masks (Tab. 1) . The FOPH recommends the use of the surgical mask (type I R, type II R) for health care workers resp. in the service sector, if a minimum distance of two meters cannot be maintained, and for persons with symptoms of acute respiratory infection who need to leave the house (e.g., for a medical appointment) [2]. The use of a FFP2/FFP3 mask is, according to the FOPH, particularly useful for directly exposed (health) professionals in activities with a high risk of aerosol generation, as well as in patient contact with justified suspicion or confirmed COVID-19. It is recommended to wear the FFP2 mask for up to 30 minutes beyond the aerosol-generating measure, and as long as the ill person is in the room. FFP2 masks can be worn by one employee for an entire shift [2]. An example of the use of a Type I R or Type II R mask is the situation where a surgeon wishes to protect a patient during a surgical procedure. “Type I filters Staphylococcus aureus at 95%, Type II at 98%”. “R” stands for “fluid resistant”, which means if a splash happens in the operating room, this mask will protect against it. Masks with which health professionals can protect themselves are the FFP2 and FFP3 models. International standards exist for both surgical masks and respirators. The FFP2 and FFP3 masks are characterized by the fact that they seal well on the face – the criterion of the European standard (EN149-2001) is that ≤8% of the air is allowed to escape on the side [1]. Surgical masks are therefore primarily for the protection of the patient. Type I R or Type II R also provide some protection against droplet transmission. In a National Health Services study, surgical masks were shown to result in a 6-fold reduction in exposure, with FFP2/3 masks being significantly superior with a 100-fold reduction [3]. A US study published in 2019 showed that a hygiene mask, i.e. a surgical mask type II according to the FOPH Pandemic Act, protects better than assumed [4]. The protection offered by fabric masks was investigated by the WHO in a secondary analysis. The conclusion is that the quality varies greatly, but among the different models there are those that offer quite good protection. Test parameters included filtration capacity, permeability in terms of particle size, material and effects of cleaning/washing the masks. “It’s an emergency measure, but it’s better than nothing,” explains Prof. Widmer. The Center of Disease Control (CDC) has even issued sewing instructions for fabric masks in light of the scarce availability of surgical masks [1].
Hygiene measures are the be-all and end-all
When disinfecting hands, he said, it is important to use the WHO’s 3-step technique (10 seconds per step): 1. spread two strokes of disinfectant (about 3 ml) on the palms and backs of the hands, 2. Rotational rubbing of the fingertips in the palm of the alternative hand, 3. rub both thumbs rotatorily with the other hand. This technique has been evaluated in studies and has proven successful [5,6]. Certain criteria should also be observed for gloves (“Accepted Quality Level” <4). However, the speaker is skeptical about the protective effect of gloves, as it has been shown that it can lead to negligence in disinfecting the hands. His recommendation is to use gloves only for contact with COVID-19 confirmed patients (followed by hand disinfection) or where contact with body fluids is possible.
Literature:
- Widmer A: COVID19: Protection in health care and population. Prof. Dr. med. Andreas Widmer, Deput. Head of the Clinic for Infectiology & Hospital Hygiene at the University Hospital Basel and President of the National Center for Infection Prevention. Slide presentation, digitalMedArt, May 8, 2020.
- New coronavirus: protective concepts and measures, protective masks, www.bag.admin.ch/bag/de/home/krankheiten/ausbrueche-epidemien-pandemien
- Health and Safety Laboratory: Evaluating the protection afforded by surgical masks against influenza bioaerosols. Gross protection of surgical masks compared to filtering facepiece respirators, Research Report 619, 2008, www.hse.gov.uk/research/rrpdf/rr619.pdf
- Radonovich LJ, et al: Outcomes Respiratory Illnesses among Health Care Personnel in the N95 Respiratory Group vs the Medical Mask Group. JAMA 2019, 322(9): 824-833.
- Tschudin-Sutter S, Widmer AF: Clin Microbiol Infect 2017; 23(6): 409.e1-409.e4.
- Tschudin-Sutter S, Widmer AF: Clin Infect Dis 2019; 69(4): 614-660.
Hygiene measures: Experts provide information on important questions
In which situations in everyday life is it useful to wear a mask in public? If you have contact with someone for more than 15 minutes and you can’t follow the 2m rule. This may be unavoidable, for example, during a long train ride. At the University Hospital in Basel, masks are generally compulsory, and it has been shown that this can prevent transmission among staff, explains Prof. Widmer. In any case, you should wear a mask in public transport.
How long can a mask be worn? The industry says that the mask should be changed every two hours, which is how long an operation lasts on average. However, it has been shown that you can definitely wear them longer, especially considering the scarce availability of masks. Switzerland-wide, it has been determined that you can wear the same mask for up to a maximum of 8 hours, unless there is any mechanical damage or moisture penetration. In these cases, one should use common sense. Whereas changing the mask too often could lead to an aggravation of the availability of the masks, even if it is no longer so scarce.
Can masks be reprocessed? This is possible, the FDA has developed various procedures, but their implementation is costly. In the case of surgical masks, there have been attempts to clean them using steam sterilization. Tests showed that the filtering effect was reduced by 30% as a result. For FFP2 masks, experiments were carried out in collaboration with the laboratory in Spiez. These masks then still met the EN 149 standard. “It’s a viable way to go if there’s an emergency situation,” Prof. Widmer said.
How great is protective effect of homemade masks? According to WHO studies, there is a proven protective effect, but the variability is very high. Prof. Widmer advises against homemade masks. In the case of masks without defined quality criteria, one has no certainty of protective effect proven by empirical data. If masks are mandatory, as in certain countries, it is certainly better than nothing.
How great is the risk of becoming infected via surfaces? The main route of transmission is via droplet infection. Surfaces do play a role, for example, there is an in vitro study which showed that when a chair is used, the viruses survive for a few days. Whether these data are transferable to practice is questioned. We assume that it takes 10-20 minutes until the virus is still detectable in the PCR, but no longer replicates. That is why the university hospital is disinfected very intensively, especially much-used surfaces such as elevator buttons, light switches, etc. Prof. Widmer is of the opinion that this should also be done for the public transport.
Should you wear gloves on the tram/public transport? Prof. Widmer advises against this. On the skin, the ph value is relatively low (about 5.5), which viruses do not like. On the other hand, the viruses tend to find better conditions on the gloves and also adhere somewhat better to the gloves. Since you then also disinfect your hands less, the risk tends to increase. You are a little better protected, but at the expense of others.
Source: Widmer A: COVID19: Protection in Health Care and Population. Prof. Andreas Widmer, MD. Interactive panel discussion, digitalMedArt, May 8, 2020.
Future scenarios: Experts provide information on important questions
How next: Which factors are relevant for the development of strategies? First, the normalization of social and economic life. Second, providing the best possible care for all patients, in both inpatient and outpatient settings. Factors that play a role in this: on the one hand, mortality, which is estimated between 0.4-1%, according to Prof. Manuel Battegay, MD, with age and comorbidity being important influencing factors. The other is the fact that there is still no vaccination and no proven effective therapy. “We hope the vaccine will be available in about 1 year,” though this is optimistic, Prof. Battegay said. Immunity is another relevant factor, and related to this is the question of how long immunity lasts. At the present time, no more than 5% of the Swiss population is contaminated.
Forecasts: What are the future scenarios? Possible scenarios depend on the transmission rate. This would need to be reduced by at least 60% compared to the current wave to arrive at an R0 <1 (information status: 08/05/20). Influencing factors: social distancing, hygiene, testing, contact tracing, isolation/quarantine. Looking back over the past three months (as of information 08.05.20), we can say that these measures are working, although there is a lag effect. You can’t count on contagion because the percentage of those who are immune to the virus is too small, Prof. Battegay said. “The strategy depends very much on whether effective drugs will be available,” the expert said, adding that “this could greatly reduce the wave.” The same applies to the availability of a vaccination. For a vaccination available for a very large number of people worldwide and in Switzerland, it would optimistically still take about 1 year (status of information: 08.05.20). In terms of seasonality, the virus is expected to be less active during the summer months. The measures are one thing, but a debate on values is also underway with regard to risks, protective measures, tolerable residual risks, etc. The aim of the scenarios and the strategies derived from them is to prevent a second wave. The goal of the scenarios and the strategies derived from them is to prevent a second wave.
Source: Battegay M: COVID19 Strategy – What next? Prof. Manuel Battegay, MD, Interactive panel discussion, digitalMedArt, May 8, 2020.
HAUSARZT PRAXIS 2020; 15(6): 42-43 (published 6/18/20, ahead of print).