At this year’s SGIM annual meeting, the update presentations were again very popular. And rightly so, because once again the audience learned a lot of interesting facts about the latest developments in various fields of internal medicine from proven specialists.
Rheumatology
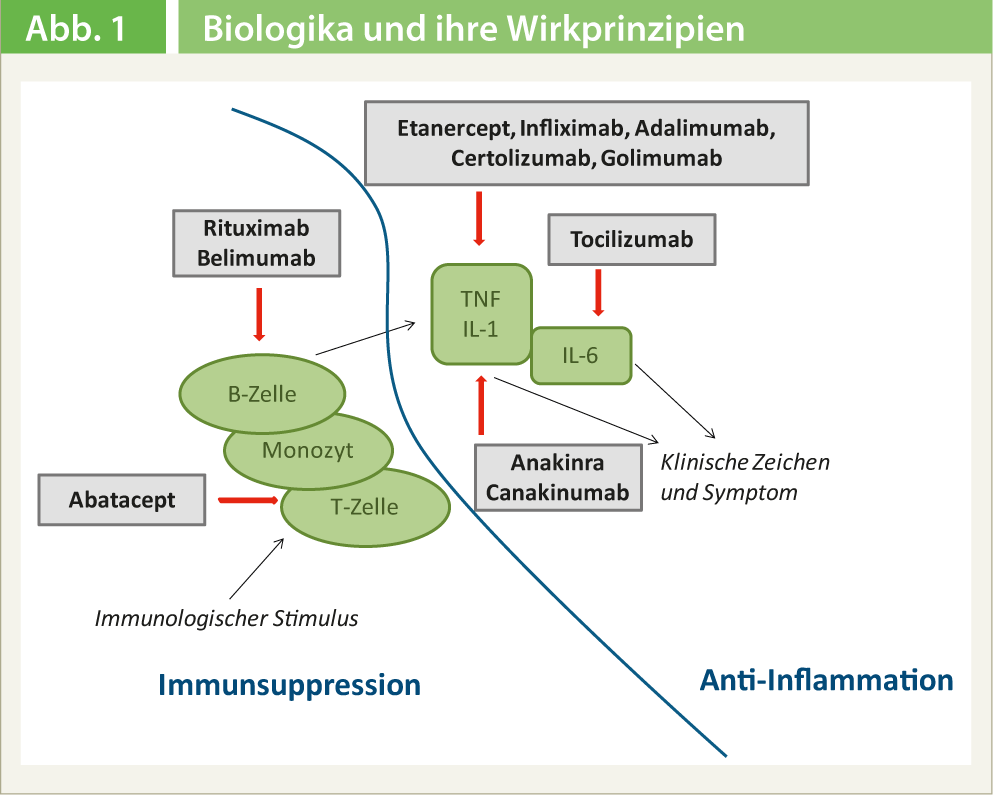
Prof. Dr. med. Peter M. Villiger, Bern, focused in his presentation on the use of monoclonal antibodies in rheumatic diseases. The different strategies of action of biologics are shown in Figure 1 and their use in rheumatology is summarized in Table 1.
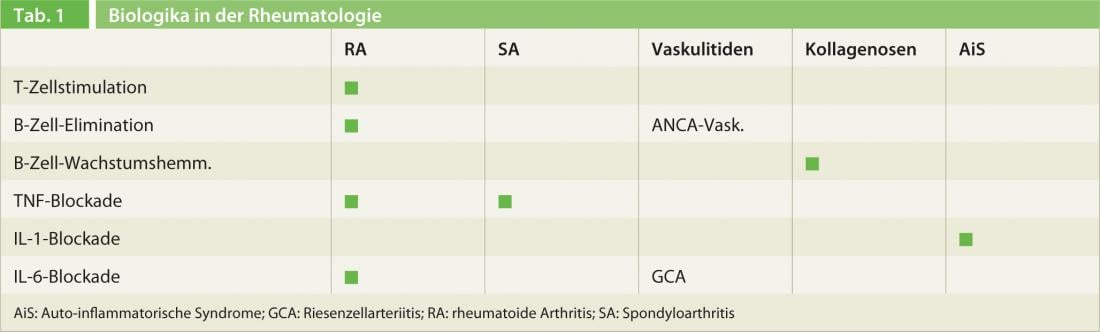
In rheumatoid arthritis (RA), TNF and IL-6 blockade, inhibition of T-cell stimulation, and B-cell elimination have been shown to be effective. However, methotrexate is still the gold standard: “No therapy can avoid methotrexate. The combination of a biologic with methotrexate leads to a significantly higher efficacy of the biologics treatment,” Prof. Villiger emphasized. Data from the “Swiss Clinical Quality Management in Rheumatic Diseases” [1], which follows around 7000 patients throughout Switzerland, show among other things that, contrary to frequently expressed fears, the incidence rate of malignancies is not increased under biologics.
“ Spondyloarthritis is now increasingly divided into an axial and a peripheral form, and the name ankylosing spondylitis will disappear altogether over time,” Prof. Villiger explained. Spondyloarthritis is classified according to the ASAS (“Assessment of SpondyloArthritis international Society”) criteria [2, 3]. Of the biologics, only the TNF inhibitors are suitable for spondyloarthritis, but these show very high efficacy. There are no significant differences between the various agents, and unlike RA, the combination with methotrexate does not confer any advantage in the axial forms.
In vasculitides, IL-6 inhibition is a very efficient mechanism of action for the treatment of giant cell arteritis. However, this is currently an off-label therapy. A Phase II study to formally confirm the previous results is currently underway at Inselspital in Bern. “If you have >50-year-old patients with suspected giant cell arteritis (BSR >40 mm/h u/o CRP >20 mg/l), please contact me (peter.villiger@insel.ch) so that we can include the patients in the study if necessary,” Prof. Villiger urged the audience in Basel. In ANCA-associated vasculitides – here, too, the nomenclature has been changed: Wegener’s disease is now called granulomatosis with polyangiitis (GPA) and Churg-Strauss is now called eosinophilic GPA – the B-cell eliminator rituximab is suitable for both induction of remission and maintenance of remission. “It is important that treatment is adapted to the disease activity and organ involvement pattern. Not every patient needs biologic therapy. In organ- or life-threatening forms, cyclophosphamide is still used initially,” Prof. Villiger pointed out.
For the treatment of collagenoses, in addition to the known modes of action (B-cell elimination and T-cell stimulation), there is a new substance, belimumab, which neutralizes an important B-cell growth factor. “Studies show that with this substance a substantial saving of steroids is possible,” the expert emphasized. In autoinflammatory syndromes, the IL-1 blockers anakinra (1× daily) and canakinumab (duration of action 8 weeks) show excellent efficacy.
Geriatrics
Adding to the “frailty” defined by Linda Fried over a decade ago [4, 5], a recent article in the Lancet is seminal in the clinical assessment of this vulnerability in elderly patients [6]. In addition to physical reserves, central nervous, endocrine immunological and nutritional factors and physical activity are also considered here. “In a frail patient, it is often the case that the quality of life and functioning in everyday life are still guaranteed as long as everything goes well. But when a stressor occurs, even if it is only a banal urine infection, the manifold symptoms of frailty manifest themselves in such a patient,” explained Prof. Reto W. Kressig, MD, Basel.
One of the greatest challenges in geriatric medicine continues to be dementia, which affects one-third of all people over the age of 85. Despite intensive research, there is still a lack of drugs that would be able to stop the disease. One difficulty is that cerebral changes begin long before the first signs appear, so efforts are underway worldwide to develop tests for early detection. Prof. Kressig and colleagues have succeeded in showing the earliest signs of a decline in brain performance with the aid of gait analysis [7]. “There are interesting new developments in the field of nutritional supplements. Apparently, a significant improvement of memory can be achieved by the intake of certain nutrients,” Prof. Kressig further explained [8, 9]. A large EU study, in which three Swiss centers are also participating, is currently investigating the role of vitamin D, omega-3 fatty acids and regular physical activity for the health of seniors. In the Basel area, people are being sought for this study who are at least 70 years old and still live independently at home (interested parties can contact do.health@fps-basel.ch).
Another important nutrition-associated age change is sarcopenia. Between the ages of 30 and 80, total muscle mass physiologically decreases by about 30%, primarily affecting the fast type 2 muscle fibers. A good supply of protein can effectively counteract this muscle atrophy, which, among other things, significantly increases the risk of falling. Here it has been shown that not only the total amount of protein consumed daily is decisive, but predominantly the distribution over all three meals. “Ideally, older people consume 25-30 g of protein in the morning, at noon and in the evening,” Prof. Kressig concluded.
Gastroenterology
For the treatment of patients with severe, refractory chronic constipation or severe irritable bowel syndrome (IBS), there are three promising new compounds that have recently been approved or are close to approval. Lubiprostone (Amitiza®), a prostaglandin analog, activates chloride channels and secretion in the colon, leading to an increase in stool frequency. Prucalopride (Resolor®) is a serotinin receptor agonist and increases intestinal motility and peristalsis [11]. Linaclotide (Constella®) stimulates the secretion of cGMP (cyclic guanosine monophosphate) and thus also the secretion of fluid in the intestine, resulting in an impressive acceleration of intestinal transit [12]. “In IBS, it also seems possible to achieve very good results with well-done hypnotherapy [13]” added Prof. Michael Fried, MD, Zurich.
With regard to screening for colorectal carcinoma, three recently published controlled studies – one of them from Switzerland – show that a single sigmoidoscopy or colonoscopy can reduce the risk of colorectal cancer. colonoscopy not only the incidence of colorectal cancer, but also mortality can be massively reduced [14–16]. Waye et al. studied what the long-term outcome is after polypectomy and found that thanks to polypectomy, mortality from colorectal cancer can be reduced by more than 50% [17]. “It is finally time for colonoscopy screening in Switzerland!” demanded Prof. Fried.
As several studies have shown, withdrawal symptoms appear to occur after discontinuation of proton pump inhibitors (PPIs). If healthy subjects are given a PPI for 28 days, the majority develop reflux symptoms after discontinuation that take several weeks to resolve [18]. The reason for this is that acid inhibition disables the feedback mechanism. “PPIs should therefore be dosed as low as possible and always phased out slowly,” the expert said.
The question of whether Helicobacter pylori should be eradicated in functional dyspepsia remains controversial. “Based on several recent studies, which showed a significant improvement in symptoms with an NNT of 8-12, I think an eradication attempt should be made [19]”, Prof. Fried opined. According to the Maastrich Consensus Report, eradication should always be performed in the presence of iron deficiency anemia of unclear cause, idiopathic thrombocytopenic purpura, or vitamin B12 deficiency. It is also known that eradication can improve the absorption of drugs (thyroxine, L-dopa).
Pneumology
Because lung cancers detected early are associated with significantly longer survival than those diagnosed in the late stages [22] – which is unfortunately the case with the majority of diagnosed lung carcinomas – it is hoped that screening will trigger a so-called stage shift, i.e. find many more carcinomas in early, localized stages that can be treated curatively. In the National Lung Screening Trial (NLST) [23] with over 50 000 subjects, CT screening was shown to reduce mortality by 20% compared to conventional chest X-ray, as significantly more stage I tumors and significantly fewer stage IV tumors were found with the more sensitive CT. Based on these results, various American societies recommend CT screening for smokers over 55 years of age or ex-smokers with at least 30 packyears with a level of evidence B. “Should screening for this risk population therefore also be recommended across the board in Switzerland?” asked Prof. Malcolm Kohler, MD, Zurich. In his opinion, the results of further ongoing studies should be awaited beforehand, as it is not clear how high the proportion of overdiagnosis was in the NLST, how often screening should be performed, what the cost-effectiveness is, and what the side effects of this screening are. Further, he said, one must ask whether we would even be able to perform 1 million additional CTs per year. “In summary, CT screening may reduce lung cancer mortality, but we do not yet know enough about it, which is why Swiss experts do not (yet) recommend nationwide CT screening,” Prof. Kohler maintained.
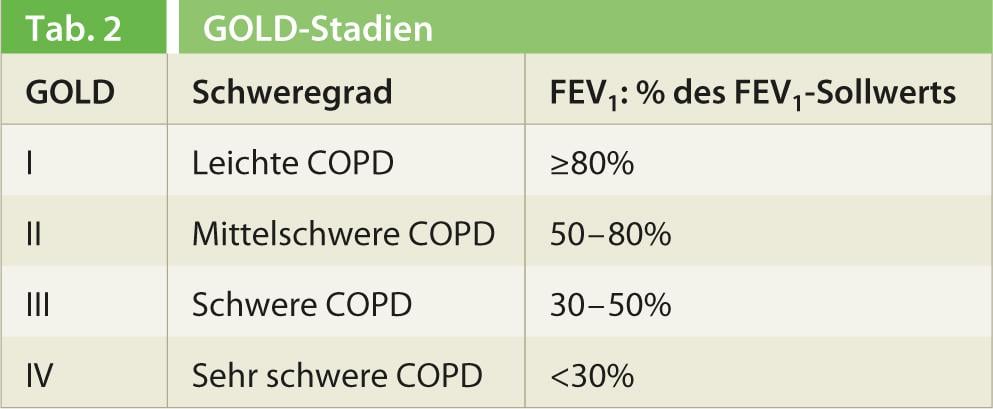
According to the new GOLD (“GlobalInitiative for Chronic Obstructive Lung Disease“) guidelines published in 2013, all patients with dyspnea, chronic cough, or sputum production who smoke or have smoked should be considered for COPD and evaluated by spirometry. An FEV1/FVC quotient <0.7 after bronchodilator is probative of COPD if there is an appropriate history. “When you see a COPD patient, you should always address four questions,” Prof. Kohler opined:.
- What are the patient’s symptoms?
- What is the respiratory flow limitation (spirometry)?
- What is the risk of exacerbation?
- What comorbidities are present?
The COPD Assessment Test (CAT) and the modified “MRC Breathlessness Scale” are suitable for recording symptoms. Based on respiratory flow limitation, COPD is classified into four GOLD stages(Table 2). An exacerbation is any deterioration that requires a change in treatment. The most important predictor of exacerbation is previous exacerbations (≥2/J). Comorbidities such as CHD, bronchus carcinoma, osteoporosis, metabolic syndrome, depression, and muscle atrophy are common in COPD and substantially worsen the prognosis. Taking the above parameters into account, COPD patients can be divided into four risk groups (Tab. 3) and given the appropriate treatment in accordance with the guidelines. “Use algorithms for treatment, such as various companies will distribute in the near future, or read the Swiss guidelines that have just been published [24]”, Prof. Kohler advised.

Literature list at the publisher
Source: 81st Annual Meeting of the SGIM, May 29-31, 2013, Basel.











