Chemical peels have been used for centuries to rejuvenate the skin. Scientifically, however, one deals with the method only since the last century. Basically, a distinction is made between superficial (penetration depth of 0.06 mm), medium-depth (0.45 mm) and deep peels (0.6 mm). Peels act irritatively by lowering epidermal pH (superficial, fruit acid, glycolic acid, etc.), via keratolysis (superficial, salicylic acid) or protein denaturation (medium-deep to deep, TCA and phenol).
Before the botulinum era, aesthetic correction of facial features and/or wrinkles was the domain of plastic reconstructive surgery. With botulinum, we were able for the first time to treat wrinkles with a minimally invasive method – a milestone in aesthetic corrective treatment and, in principle, also the birth of aesthetic dermatology. In the meantime, there are a variety of different apparative, but also medicinal, physical and chemical treatment options for the improvement resp. Harmonization of the aesthetic unit “face”. It is useful to classify the different options of wrinkle treatments according to their respective spectrum of action:
- Mimic wrinkles: Botulinum
- Wrinkles due to a lack of volume: filler
- Wrinkles due to altered skin structure: chemical peeling, ablative laser.
As simple as the classification is, it is astonishing that this principle is all too often disregarded. Instead of the indicated discrete volume augmentation of the midface, the face is blocked into a mask using botulinum or the lips are pumped up into grotesque caricatures. In the vast majority of cases, this mistreatment is due to a lack of training, sometimes even a lack of training, on the part of the attending physician. As in any field of medicine, it is essential in aesthetic dermatology to perform an accurate analysis of the problem and establish a treatment plan prior to treatment. The therapy depends on the clinic [1]! In professional hands with the correct indication, botulinum and hyaluronic acid injections, especially when used in combination, can achieve amazing aesthetic results – or conversely, avoid disfiguring comic-like results.
However, in the case of changes in the skin structure, we will not get anywhere with botulinum or fillers. If the treating physician is confronted with superficial pigmentary changes (lentigo solaris or senilis), with actinically damaged skin (superficial actinic elastosis or actinic keratoses) or with deeper structural changes of the skin (pronounced actinic elastosis, large pores, acne scars), he must treat the skin itself and not the underlying structures (augmentation in case of lipatrophy or muscle relaxation in case of mimic wrinkles). When it comes to the skin, chemical peeling comes into play.
What is chemical peeling and how does it work?
Chemical peels have been used for centuries to rejuvenate the skin, but only came into the focus of science since the last century. As early as 1600 BC herbal poultices in the sense of keratolytic solutions were used by the Egyptians for rejuvenation. In 1882, Paul G. Unna treated scars using salicylic acid, TCA, resorcinol and phenol. In 1942, phenol and resorcinol were applied in combination for the first time by J.J. Ellers and S. Wolff [2]. However, the real breakthrough of deep peeling is due to Thomas J. Baker and Howard L. Gordon. In 1961, they described a modified phenol solution with septisol and croton oil [3]. The latter is of crucial importance for the deep effect of the peeling. The Baker-Gordon solution is still used today worldwide as a standardized phenol peeling solution, in some cases adapted. Especially in the 1990s, medium-depth and deep peeling first received competition from ablative laser resurfacing. CO2 laser resurfacing really boomed after its introduction, but it was rejected because of the considerable acquisition and maintenance costs, the long downtime and the not inconsiderable risk of milia or other damage to the skin. Scarring abandoned by majority in favor of fractional laser. Fractional laser treatment has also been somewhat quieter recently due to insufficient results (even after multiple applications).
Chemical peels, on the other hand, ranked 4 among noninvasive aesthetic treatments in the U.S. in 2014, after botulinum resp. Hyaluronic acid injections and epilation with laser resp. IPL devices. In 2010, chemical peels still took the fifth place after laser resurfacing, which could be an indication that ablative laser might be replaced by the different peeling methods [4]. We distinguish between the peeling methods:
- Superficial peels with a penetration depth of 0.06 mm
- Medium depth peels with a penetration depth of 0.45 mm
- Deep peels with a penetration depth of 0.6 mm.
Depending on the substance, chemical peels damage the epidermis or the dermis with subsequent regeneration of the destroyed skin structures by de novo synthesis of the dermal connective tissue, respectively. epidermal regeneration. Which skin structures a peel reaches depends on various factors, but essentially on the chemical properties and the method of application. Basically, different methods of chemical peels can be distinguished:
- Irritative effect due to lowering of the epidermal pH (superficial, fruit acid, glycolic acid etc.)
- Keratolysis (superficial, salicylic acid)
- Protein denaturation (medium-deep to deep, TCA and phenol).
Superficial peels
By lowering the epidermal pH, protein structures are altered in addition to irritative inflammatory processes. This results in a loosening of the cell cohesion between str. corneum and granulosum with corresponding increased desquamation. The change in pH also impairs intercellular enzymes, which in turn leads to an amplification of the inflammatory cascade and supports desquamation. The induced inflammation stimulates collagen synthesis in addition to glycosaminoglycans. The latter occurs via induction of IL-1A on keratinocytes and fibroblasts with initiation of cell proliferation [5].
Due to the principle of action with lowering of the pH value, the superficial peelings usually have to be neutralized after a certain retention time. The extent of irritation and thus the success of the therapy depends on the choice of substance (alpha hydroxy acids, salicylic acid, glycolic acid, etc.), the concentration of the substance (20-70%), the method of application (preparation of the skin, application pressure, number of passes) and the time spent on the skin until neutralization. Superficial peelings are generally uncomplicated in application and can therefore be delegated. In order to achieve a sufficient effect, these peel procedures should be repeated approximately four to six times at weekly intervals. As aesthetic effects, improvements of cell atypia (initial epidermal tumors) and especially pigmentary shifts (lentigines, poikiloderma) can be observed after completion of the serial treatment. In addition, there is a visible and also palpable improvement of the skin structure with compact, smooth and shiny epidermis. The indication for performing superficial peelings is to refresh the skin and its structures. To achieve a lasting effect, these peels should be performed once or twice a year, depending on the skin condition. However, even with the relatively easy-to-apply superficial peelings, basic knowledge and experience in handling the various peeling solutions are extremely important in order to avoid complications such as irregular results or hyperpigmentation. The following principle also applies to superficial peelings: the therapy depends on the clinic.
Medium depth and deep peels
Unlike the superficial peels, where the exfoliation and regeneration of the epidermis are the main focus, the medium-depth and also deep peels act by de novo synthesis of the dermis and extracellular matrix [6]. Thus, medium-depth and deep peels are invasive medical measures. The clinically detectable effects are based on denaturation of extracellular and cellular structures. In the process, protein structures are completely abolished and, in isolated cases, even cell necrosis is induced. In the dermis, medium-depth and deep peels cause degradation and rebuilding of all structural components with induction of inflammatory wound healing cascades. This in turn leads to a pronounced and, above all, long-lasting immune response [7]. The latter has clinical relevance, as the inflammatory reaction persists for weeks post interventionem and thus long-lasting redness of the treated area persists. The clinical effect is thus persistently improved even weeks to months after the actual treatment. This fact is important in patient education: it should be pointed out that the clinical effect is not yet complete after complete epithelialization has occurred and will continue to improve (“Erythema is not our enemy, it is our friend!”). Aesthetic effects are expected to be the reduction of scar tissue, restitution of firm and elastic skin structure and rejuvenation of the overall skin appearance.
Basically, all peels that act down into the str. papillare are referred to as medium depth. Deep peels destroy into the medial str. reticulare. If the str. reticulare is exceeded, there is a risk of scarring [5]. It is important to note in this context that the re-epithelialization of dermal peels originates from the hair follicles. Particular caution is therefore required when treating areas of skin outside the face that are poor in sebaceous glands. Here, delayed wound healing is to be expected due to reduced re-epithelialization. In clinical practice, this means that deep phenol peels should be limited to treatment of the face and scalp. For the treatment of the neck, upper body, arms or back of the hands, TCA solutions 15-25% are used.
Recipes and application of chemical peels
Especially in the case of superficial peels, we have a wide range of ready-to-use preparations at our disposal. In addition to the various peeling solutions (AHA, salicylic acid or glycolic acid), manufacturers offer entire complete packages with appropriate pre- and post-treatment. Inexperienced users are advised to gain their own experience with such commercial finished products before starting to treat patients with individualized magistral formulations in different concentrations. Magistral prescriptions are expertly prepared by the local pharmacist according to specifically issued prescription. Abroad, pre-produced TCA solutions in various concentrations are also available from major distributors. Phenol solutions are not commercially available in Switzerland and must always be prepared by magistral formulation.
Superficial peels: there are numerous superficial peels ranging from alpha hydroxy acids (AHA), to salicylic acid (SA), to Jessner’s solution (Table 1) .
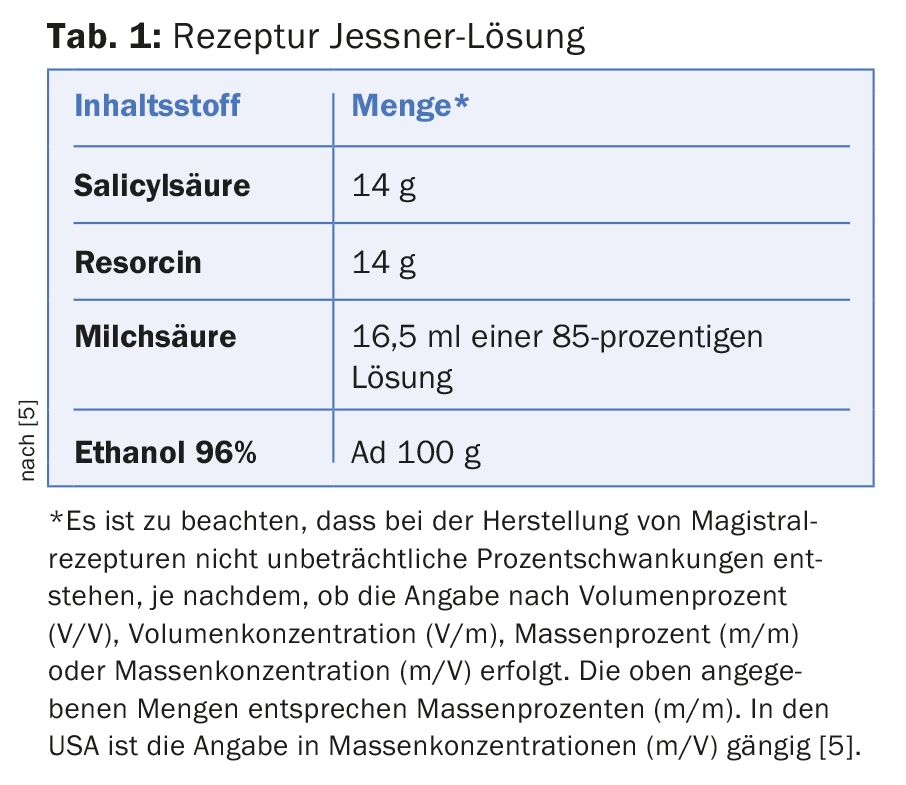
AHAs were originally isolated from fruits (mandelic acid, lactic acid, citric acid, tartaric acid), which is why they are also called fruit acid peels. AHAs are relatively weak acids and come in concentrations of 20-70%. AHA peels usually need to be neutralized to stop the process. Since AHAs are hydrophilic, preceding degreasing of the skin area to be treated is crucial for a good result. Salicylic acid has not only an irritant exfoliative effect, but also a keratolytic effect. Depending on the concentration (10-30%), it acts very superficially or somewhat deeper, but never medium deep. Jessner’s solution can be used as monotherapy for superficial exfoliation. As a direct pre-treatment for medium-deep TCA or deep phenol peels, Jessner’s solution is particularly suitable, as its pre-irritation of the skin surface results in significantly better penetration of the subsequent TCA or phenol peels. In the Jessner solution, three substances with different effects are combined. The lactic acid causes epidermolysis, the salicylic acid keratolysis and the resorcinol a slight denaturation. Due to this denaturation, neutralization as we know it from the AHAs is not possible.
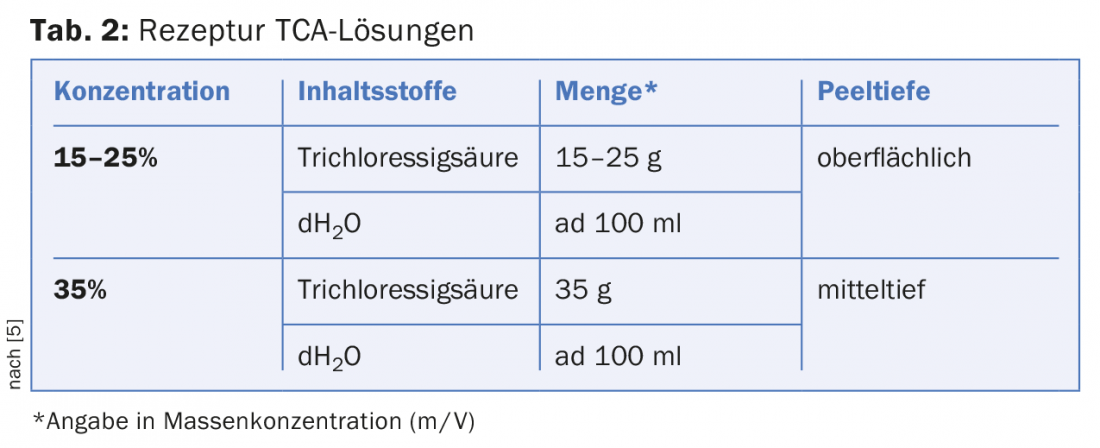
Medium-depth peels: Here, the trichloroacetic acid (TCA) solutions are particularly worthy of mention (Tab. 2) .
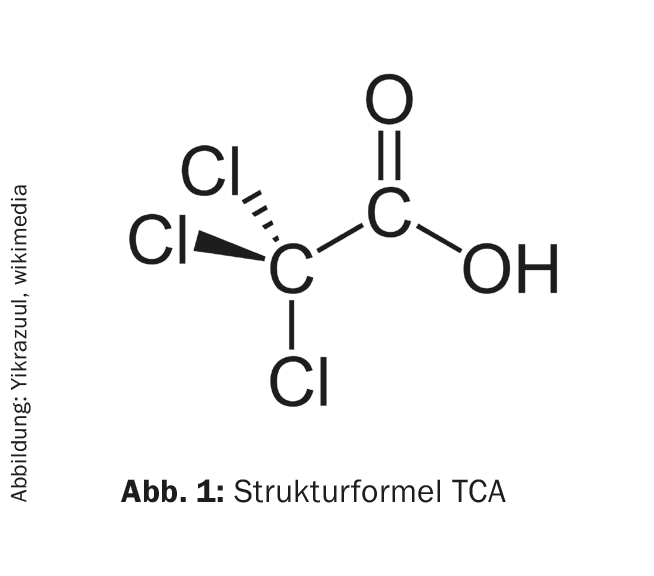
TCA (“trichloroacetic acid”) solutions are a triply chlorinated carboxylic acid (Fig. 1) .
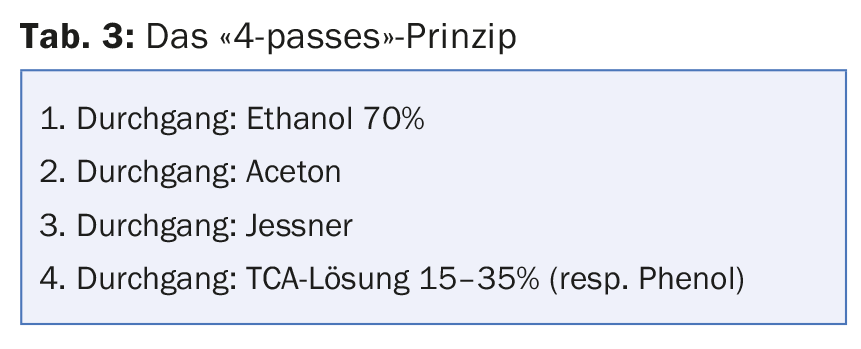
The effect of TCA is based on its ability to coagulate proteins. The protein denaturing effect of TCA, however, depends mainly on the application method. Before peeling, it is mandatory to thoroughly degrease the skin. The triple pretreatment (Tab. 3) directly before the application of the TCA with gentle but continuous pressure only produces the desired results. Or vice versa: a superficial peeling can also be achieved with a 35% TCA solution, apply the solution without pressure and without preparing the skin.
Depending on the concentration, TCA peels are classified as superficial or medium-depth peels. To avoid scarring, a higher concentration than TCA 35% (e.g. TCA 50%) is not recommended. If a deeper peeling is indicated, it is recommended to resort to the phenol peeling. In order to achieve effective results, TCA and phenol peels are practically always applied as combination peels (with Jessner solution).
As with the Jessner solution, TCA solutions cause protein precipitation, which manifests itself in a white discoloration of the treated area after about two minutes after application, the so-called frosting. The more compact and white the frost, the deeper the peeling performed (Fig. 2).

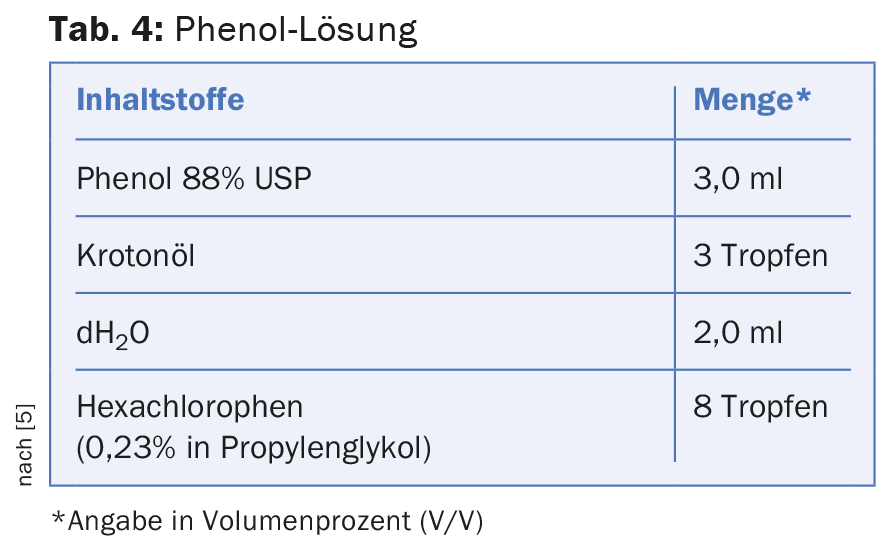
Deep peels: Actually, only the phenol peel is used for deep peels (Tab. 4) .
Phenol is a hydroxy-substituted derivative of benzene and a weak acid (Fig. 3).
Theoretically, higher concentrations of TCA solutions are also conceivable, but they are not recommended due to the risk of scarring. The reason for this is the different chemical modes of action of the two preparations. In the case of the TCA solutions, the penetration depth can be increased considerably under certain circumstances by the increase in concentration and by the type of application (combination peels, application pressure, number of treatment passes). If these parameters are increased arbitrarily, there is an immediate risk that the str. reticulare will be exceeded, resulting in scarring.
In the Baker-Gordon phenol peel, the formula is always identical. This allows a relatively accurate prediction of the penetration depth of the peeling solution and thus a predictive final result. Of course, complications such as scars etc. can arise from improper application, such as too high an application pressure or too many passes, but also in particular from a change in the way the phenol solution is applied. Since the very intense and compact frosting occurs very quickly during phenol application, the risk of inadequate multiple passes is low resp. the risk of the phenol solution diffusing into deeper layers due to excessive concentration is considerably smaller than with higher-concentration TCA solutions.
Formulations containing phenol are not emulsified and must therefore be stirred constantly during use. The addition of croton oil is responsible for increasing the penetration depth of the phenol peel, which is why numerous modifications of the Baker-Gordon solution described above exist (from one drop to twelve drops of croton oil, use of septisol instead of hexachlorophene, addition of olive oil or glycerol, etc.). However, most studies have been performed with the classic Baker-Gordon solution, so this remains as the recommendation guideline.
Phenol penetrates rapidly and is also absorbed percutaneously with the potential risk of systemic absorption. The potentially lethal dose of phenol is reported to be 10-15 g. Less than 1 g of phenol is needed for a full-face phenol peel. Due to these differences in quantity, the systemic side effects so often cited, such as arrhythmias, renal or hepatic affections, are also extremely rare and negligible in everyday clinical practice when peeling is performed correctly [5]. The absorption of phenol can be critical if too large quantities are applied to too large an application area in too short a time. Prior to phenol peeling, patients must be evaluated for intact cardiac, hepatic, and renal function. In addition, phenol peeling should not be performed without anesthesia stand-by with monitoring of baseline functions. Exceptions can be made in experienced hands at most for very small treatment areas (e.g. perioral region).
In the second part of the series, the peeling indications shown in Figure 4 will be discussed in detail.

It also addresses patient selection and care, and provides helpful tips for avoiding complications. You can be happy!
Mark your calendar!
SGEDS course at the Methininserhof practice:
Chemical Peel Course (TCA & Phenol)
Saturday, 31.10.2015
Registration and information on SGEDS membership at www.sgeds.ch
Literature:
- Kreyden OP, et al.: Swiss Group of Esthetic Dermatology and Skincare (SGEDS): The satisfied patient in aesthetic dermatology. Consensus paper on patient satisfaction in botulinum toxin A treatment. Dermatologist 2015 Feb; 66(2): 131-136.
- Coleman WP, et al: A history of dermatologic surgery in the United States. Dermatol Surg 2000 Jan; 26(1): 5-11.
- Baker TJ, Gordon HL: The ablation of rhytides by chemical means. A preliminary report. J Fla Med Assoc 1961; 48: 541.
- Statstics Cosmetic Surgery National Data Bank. www.surgery.org/sites/default/files/2014-Stats.pdf
- Schürer NY, Wiest LG: Bildatlas Peeling, Grundlagen, Praxis, Indikationen. KVM Publishing. ISBN 978-3-940698-74-2.
- Baker TJ, et al: Long-Term histologic study of skin after chemical face peeling. Plast Reconstr Surg 1974: 53(2): 522-525.
- Glogau RG, Matarasso SL: Chemical peels: trichloroacetic acid and phenol. Dermotol Clin 1995; 13: 263-276.
DERMATOLOGY PRACTICE 2015; 25(5): 32-37











