Diagnostic latency is burdensome for affected individuals and, in some cases, results in a “window of opportunity” going unused and a missed opportunity for effective treatment.
The saying “When you hear hoofbeats, you should think of horses, not zebras,” which translated into clinical practice means that common diseases should be considered first in diagnostic workups, is sometimes somewhat misleading, he said. Especially if the findings are unclear, one should also think about rare diseases, says Eva Luise Köhler of the Eva Luise and Horst Köhler Foundation for People with Rare Diseases [1]. In Europe, the criterion for prevalence is that no more than 5 in 10,000 people are affected. According to ICD-11 [2], 5400 rare diseases are recorded, but in reality their number is probably even higher.
Consequential diagnostic latency
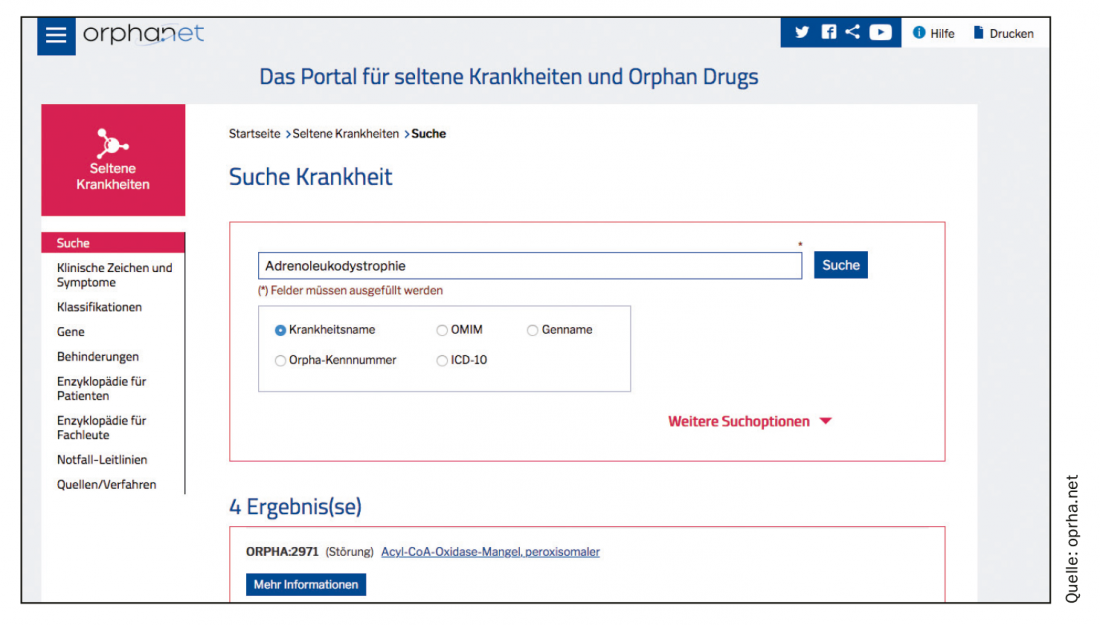
The average time to diagnosis is about seven years, although every second rare disease manifests itself in childhood or adolescence. This reflects the fact that until a rare disease is diagnosed, there is often an odyssey of different clarifications and examinations. Only with a diagnosis do you become entitled to personal and functional assistance as well as access to the best possible counseling and therapy, the speaker explained. The potential consequences of delaying diagnosis can be fatal, as she illustrates with two case studies. The first case involves a boy who develops behavioral abnormalities in various areas during the second year of school. After a nine-month assessment, the diagnosis of “atypical attention deficit disorder” is made. An MRI scan performed later on the initiative of the parents finally leads to the diagnosis of adrenoleukodystrophy [3] a hereditary neurodegenerative metabolic disease. If detected early, this disease is treatable by bone marrow transplantation. In this case, however, the diagnosis was made too late. In the second case study, the lecturer described the course of a boy’s disease, in whom retarded development and a decline in competencies in everyday life were observed at the age of three. Her concerns, communicated to the physician, were not taken seriously until epileptic seizures occurred. Based on brain wave measurement, drug treatment was performed. After the parents urged further investigations, a detailed workup was performed at a university hospital, resulting in a diagnosis of neuronal ceroid lipofuscinosis (CLN2) [4]. This disorder is a dementia disease that occurs in childhood. Treatment is also possible for this diagnosis, but its success depends on early intervention, she said.
How to avoid clarification odysseys and doctor hopping
The two case studies are exemplary of the process of delayed diagnoses – something that unfortunately occurs frequently and is characterized by certain patterns (box).A delayed diagnosis is not primarily due to a lack of expertise, but is usually also related to inefficient communication between patients/relatives and medical treatment staff (primary care providers/specialists). However, it is also a major problem inherent in the system, as time for communication and cooperation is hardly remunerated in the German healthcare system. “If physicians can only afford a few minutes for communication with patients and colleagues, the weakest in the system suffer the most,” the speaker explained. In terms of raising awareness on the topic of rare diseases, however, a lot of progress has been made in recent years, Ms. Köhler points out. For example, since 2010, Germany has had a National Action Alliance for People with Rare Diseases (NAMSE) [5], a nationwide initiative with 27 alliance partners that has developed a 52-point action plan to improve medical care for patients with rare diseases. A key element of this care plan is the approximately 30 rare disease centers that have been established nationwide over the past decade. The speaker pleaded for further expansion of the care structures of these institutions and emphasized the importance of needs-based services and public relations.
“Digital Health” as an opportunity
In this context, user-friendly and barrier-free websites are also important. The digital transformation offers numerous opportunities for the field of rare diseases, on the one hand through the possibility of optimizing uncomplicated communication (e.g. telemedicine, etc.) and on the other hand through a comprehensive and sensibly organized electronic patient file as the basis for adequate diagnosis and therapy. The documentation of medical findings and clarifications should be accessible and comprehensible. Finally, the speaker states that she is confident about the future. The topic of rare diseases is receiving increasing attention in clinical practice and research, and media interest in it has also increased. She considers the fact that rare diseases are increasingly represented in the program of important medical congresses and also find space in health policy agendas to be a thoroughly positive development.
Literature:
- Köhler EL: Recognizing rare diseases. Presentation Eva Luise Köhler, Foundation for People with Rare Diseases (D). Main Meeting, DGIM May 5, 2019.
- DIMDI: ICD-11 – 11th revision of the WHO ICD, www.dimdi.de/dynamic/de/klassifikationen/icd/icd-11
- Orphanet: Adrenoleukodystrophy, www.orpha.net/consor/cgi-bin/OC_Exp.php?Expert=43&lng=DE
- Orphanet: neuronal ceroid lipofuscinosis (CLN2), www.orpha.net/consor/cgi-bin/OC_Exp.php?lng=DE&Expert=216
- National Action Alliance for People with Rare Diseases (NAMSE), www.namse.de
GP PRACTICE 2019; 14(12): 36-37