After the medical efficacy of thrombolysis was scientifically proven, great efforts were made in the USA, Canada, Australia and most European countries to improve the infrastructure for the earliest possible, interdisciplinary, interprofessional and stage-appropriate treatment of cerebral stroke. The focus is on improving the rescue chain and forming stroke units and stroke centers, as well as establishing and expanding suitable facilities for neurorehabilitation. For prevention, patient education regarding healthy lifestyle is central. In terms of medication, for example, attention must be paid to good blood pressure control and anticoagulation for atrial fibrillation.
Brain stroke is the third leading cause of death and the most common cause of permanent disability in adulthood. According to estimates, about 16,000 cerebral strokes occur in Switzerland every year. In addition to the tragedy of each patient’s fate, cerebral stroke also leads to immense costs, since without therapy almost half of the patients remain disabled.
Given the short time between symptom onset and effective recanalization by intravenous thrombolysis and/or endovascular therapy, the processes in the prehospitalization phase and in the acute phase in the hospital must be well organized. Every minute is precious and any loss of time should be avoided at all costs. Numerous studies have shown that the majority of time is lost in the prehospitalization phase. Delays often occur when patients, family members, or passersby fail to recognize or take brain stroke symptoms seriously. That is why information campaigns are of central importance. In Switzerland, these are coordinated primarily by the Swiss Heart Foundation, which has done excellent work in recent years – for example, in the context of the cerebrovascular accident campaign and the HELP campaign. Unfortunately, there is still no legal framework for government-funded vascular disease education campaigns.
It is also not uncommon to experience delays due to complicated multi-level alerting paths. As a Bern study has shown, the least time is lost in the prehospitalization phase when the alert is made via 144 [1]. Therefore, if a stroke is suspected, 144 should be dialed immediately. In hospitals, infrastructure, processes and staff availability must be well organized to avoid unnecessary loss of time after arrival at the emergency department. Complete recording and regular analysis of the duration from symptom onset to imaging and therapy in the acute phase are among the most important tasks of stroke centers and stroke units.
Stroke Units and Stroke Centers
The concept of stroke units (SU) is that specialized physicians assess the patient with suspected stroke as early as possible so that diagnosis and targeted therapy can be initiated immediately. Patients receive interdisciplinary care from neurologists, neuroradiologists, specialized nurses, internists, anesthesiologists, intensivists, neurosurgeons, and cardiologists, vascular surgeons, and angiologists, as needed, on a unit that admits only or primarily patients with acute cerebrovascular disease. In addition, trained physical and occupational therapy and speech therapy teams must also be available.
In addition to specialized acute treatments, the focus is also on early clarification of the cause of stroke and targeted prevention. Particular importance is also attached to information: The clinical picture must be communicated to patients and relatives in a way that they can understand. Numerous English, Scandinavian and American studies have shown that this interdisciplinary specialized treatment of stroke patients significantly reduces mortality and the ongoing risk of disability. Hospitalization times, the risk of admission to a nursing home and overall costs have also been impressively reduced because the degree of disability of patients at discharge has been reduced overall.
Treatment in an SU is effective for all severities and all ages of patients with stroke [2–4]. It has also been shown that a spatially defined stroke unit is superior to a functional SU (i.e., treatment by a stroke team caring for stroke patients on different wards in the hospital).
A Stroke Center (SC) includes a stroke unit and offers the full spectrum of modern stroke medicine around the clock (interventional neuroradiology, vascular surgery, neurosurgery, cardiology, etc.). The focus is on acute endovascular treatment of stroke, acute carotid revascularization, and decompressive hemicraniectomy.
Certification of stroke units and stroke centers
On January 8, 2012, the decision-making body of the Intercantonal Agreement on Highly Specialized Medicine (IVHSM) awarded the mandate for certification of stroke centers and stroke units to the Swiss Federation of Clinical Neuro-Societies (SFCNS)/Brain Stroke Commission. This mandate is based on the decision of the IVHSM decision-making body of June 21, 2011. SFCNS is the umbrella organization for clinical neuroscience. In appointing the SFCNS Brain Stroke Committee, much emphasis was placed on including representatives from the various specialties (neurology, neurosurgery, neuroradiology, internal medicine, intensive care medicine).
The primary goals of certification are to ensure quality in the care of stroke patients in Switzerland based on professional considerations and to ensure comprehensive care of stroke patients in networks. The certification criteria are based on scientific evidence and take into account the guidelines of the European Stroke Organisation (ESO) and the Swiss Stroke Society (SHG).
In addition to professional competence and infrastructure, special emphasis is placed on the networking of service providers, the organization of the rescue chain, and institutional treatment and monitoring guidelines during the certification process. A national stroke registry (Swiss Stroke Registry) is under development and will identify gaps in care in addition to quality control.
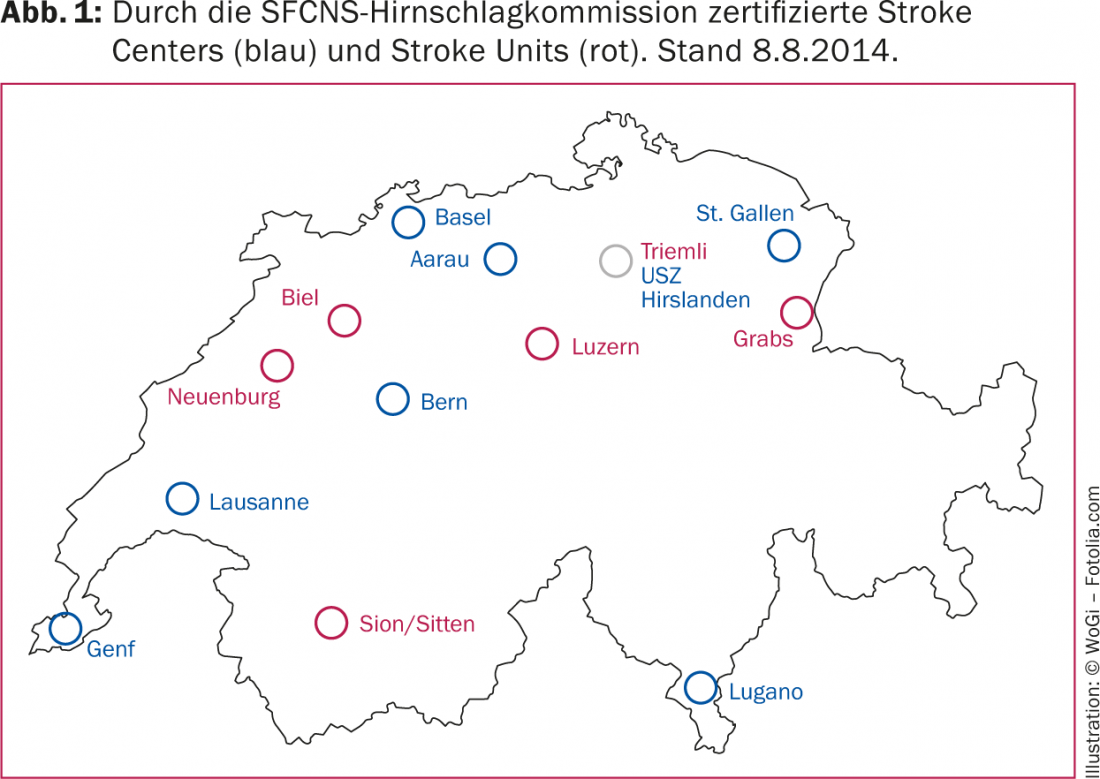
In addition, the SFCNS Brain Stroke Committee was charged with documenting coordination in continuing education and research. In the meantime, eight stroke centers and six stroke units have already been successfully certified in Switzerland (Fig. 1). Numerous other hospitals are in the process of certification or have applied for it. In most regions with certified stroke centers and/or stroke units, a significant improvement in the care structure has been observed so far. Detailed information about the certification process can be found at www.sfcns.ch.
Networking
The SFCNS Brain Stroke Commission and the Swiss Brain Stroke Society recommend that Swiss stroke units and stroke centers form regional networks of stroke care in mutual consultation [5]. It is important that all stakeholders (primary care providers, emergency physicians, emergency medical services, regional hospitals and rehabilitation clinics) are involved. Teleradiology and telemedicine offer the possibility to closely network even geographically remote regions with a stroke unit and/or a stroke center and to provide them with good care. This network formation is regionally advanced to different degrees in Switzerland and represents one of the most important interdisciplinary tasks for the future.
Prevention
When we discuss cerebrovascular care, prevention should definitely not be neglected. As non-drug measures, the focus is on: a healthy lifestyle with regular physical activity (e.g., three times 30 minutes/week), a balanced diet with abundant consumption of fruits and vegetables and avoidance of high-salt diets, no nicotine consumption, and avoidance of excess weight. Medicinally, optimal management of blood pressure and anticoagulation for atrial fibrillation can substantially reduce the risk of ischemic stroke. Additional therapies with statins and antithrombotics play an important role, especially in cases of pronounced atheromatosis of brain afferent arteries and after a stroke. As already mentioned, education of the population about the symptoms of stroke and appropriate behavioral measures (“time is brain”) are of great importance, so that thrombolysis can be applied early and in time. Education should not be limited to older patients or at-risk groups, as young adults with low risk profiles are also affected.
Outlook
There are high hopes that new thrombolytics and more modern endovascular therapy concepts as well as multimodal cerebrovascular imaging will further improve the prognosis of stroke patients. To ensure that all patients can benefit from these advances, the goal should be to provide level-appropriate and comprehensive stroke care. Currently, numerous stroke units are being established in Switzerland, often in close collaboration with an established stroke center. Regional hospitals without stroke units and primary care providers will also be included in the networks. The Swiss Cerebrovascular Registry will identify gaps in care and has great potential to become an important tool in quality control and health services research in the near future.
Literature:
- Agyeman O, et al: Time to Admission in Acute Ischemic Stroke and TIA. Stroke 2006; 37: 963-966.
- Stroke Unit Trialists’ Collaboration: Organised inpatient (stroke unit) care for stroke (Cochrane Review). The Cochrane Library 2009; 1.
- Seenan P, Long M, Langhorne P: Stroke units in their natural habitat: systematic review of observational studies. Stroke 2007; 38: 1886-1892.
- Fuentes B, Diez-Tejedor E: Stroke units: many questions, some answers. Int J Stroke 2009; 4: 28-37.
- Lyrer P, et al: Stroke units and centers in Switzerland: guidelines and requirements profile. Schweiz Med Forum 2012; 47: 918-922.
CARDIOVASC 2014; 13(5): 18-20











