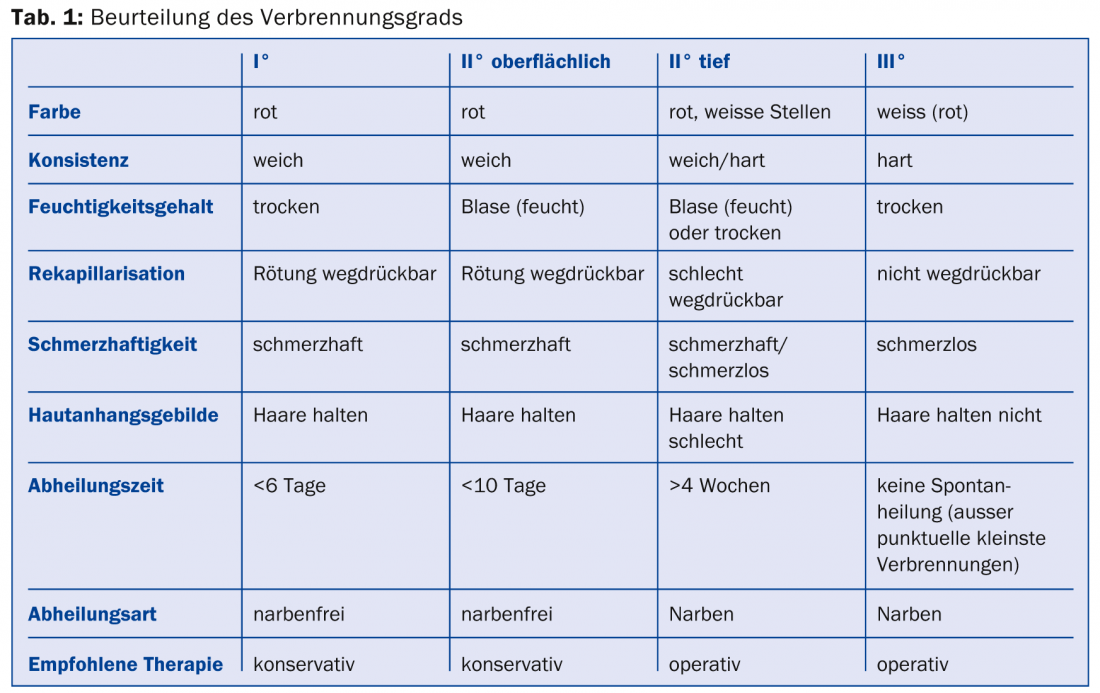
To assess the severity of the burn/scald, one needs an estimate of the area extent and depth of the burn after debridement. The degree of burn is determined by the following criteria: Color, consistency and moisture content of the wound, recapillarization and painfulness of the wound bed and adherence of skin appendages. Small thermal injuries of superficial degree can be treated on an outpatient basis in the office. Wound areas that have not healed after 10-14 days should be presented to the specialist. Scalds may re-deepen and require re-evaluation 24 hours post-traumatically. Burns involving less than 10% of KOF should not be cooled with cold (15-20°C) water for more than 10 minutes.
The causes of burns can be of various types: thermal, chemical or electrical. Overall, burn injuries are common. In this case, the small-surface thermal injuries predominate – mostly contracted in the household or during leisure time. Nevertheless, in Switzerland approx. 1000 people per year [1] hospitalized due to their burn injury. Approximately 180 people are severely burned and must be admitted to a burn intensive care unit due to the extent and severity of their injuries. In Switzerland, there are two such highly specialized centers: in Lausanne and in Zurich. When exactly patients should be referred to such a center or hospital and which burn areas can be easily treated as outpatients in the family practice will be elaborated in the following.
For adequate assessment of a burn wound, knowledge of the damaging noxious agent is crucial on the one hand, and the exposure/contact time on the other. To assess the severity, it is necessary to accurately determine the area extent and depth of the burn. The rule of nine is still suitable for determining the affected burned body surface area in adults (Fig. 1).
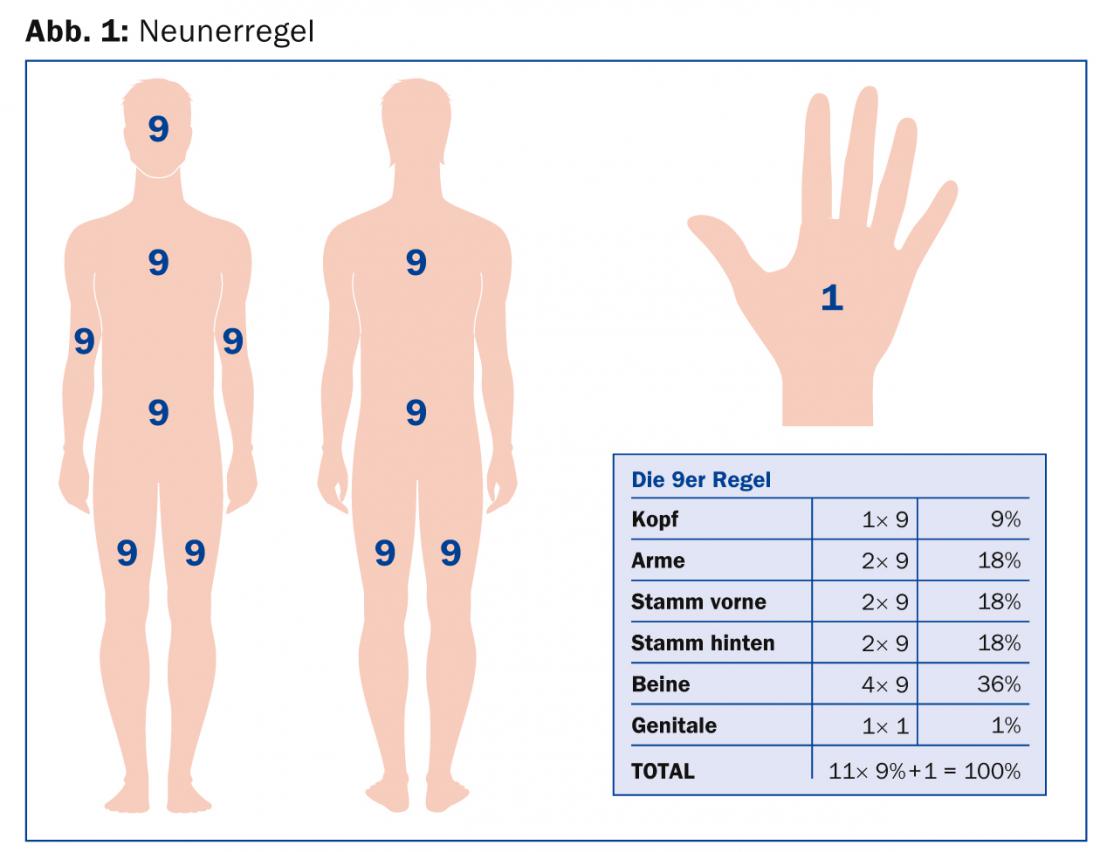
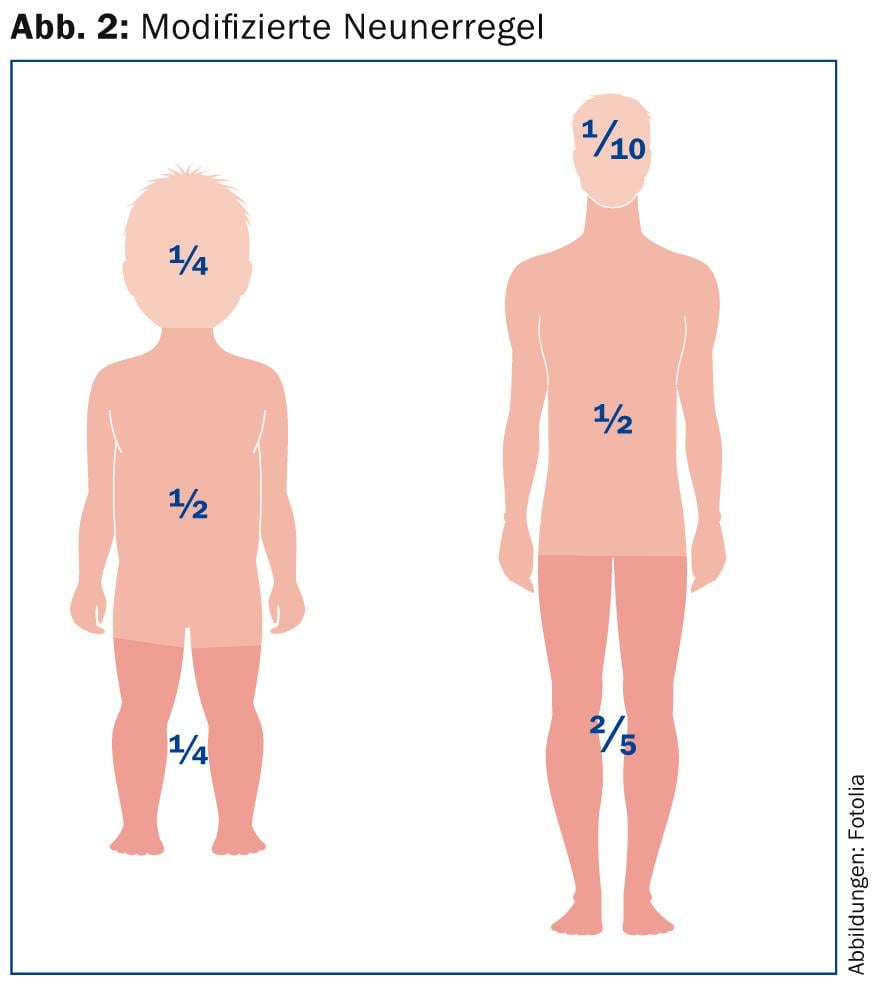
In the case of young children, this rule must be modified, since children have different body proportions with a much larger head in relation to the legs (Fig. 2) . As a simple aid to calculating the affected burnt body surface, the patient’s palm together with the fingers can be used; this corresponds to approximately 1% of the body surface [2,3]. In general, only skin areas where blistering or deepithelialization has occurred should be included in this calculation. Areas with erythema in the sense of a first-degree burn are not to be considered for the calculation of the areal extent.
To assess the degree of burn, the color, consistency and moisture content of the wound, the recapillarization of the wound bed, the painfulness and the adherence of skin appendages are determined (Table 1).
Initial supply
With the aim of preventing the burn wound from “deepening”, these wounds were cooled as standard in the past. However, as a result of the cold stimulus, there is also vasoconstriction and deteriorated perfusion of potentially survivable skin areas [4]. The risk of hypothermia in patients should also not be underestimated, which may subsequently lead to a poorer prognosis [5]. Thus, cold water therapy is the subject of discussion and there are now initial studies regarding local warm water treatment (37°C). In animal experiments, it was shown that local warm water application at 37°C was more effective than treatment with 17°C cold water. Secondary burn damage from a circumscribed local burn (approximately 15% KOF) was delayed, but not prevented, compared with untreated animals. On the surface, the burn damage after hot water application is significantly smaller than after cold water application [6].
However, the analgesic effect of cold water treatment is undisputed. As a conclusion for practice, second-degree burns involving less than 10% of KOF can be cooled with cold (15-20°C) water for ten minutes.
The resulting blisters on the wound should be opened for adequate assessment of the wound bed. However, this must be done under sterile conditions or with sterile instruments and should therefore be avoided at the emergency site.
The garments or other materials adhering to the wound are left in place and cut around in the case of more extensive burns. The burned areas themselves are covered with a sterile, non-adherent gauze dressing. The application of externals such as ointments or powders should be avoided. The application of so-called burn dressings containing gel or oil can also no longer be recommended due to a secondary cooling effect with a consequent risk of hypothermia for the patient. For transport to a hospital, the patient should be protected from cooling down by means of a warming blanket. Tetanus prophylaxis is mandatory either in the practice or in the hospital.
Infusion therapy
Not every burn requires volume therapy. The limit is at least 15% burned body surface in adults and at least 10% in children [2]. If this is the case, two large-lumen access points should be established at the accident site, if possible through unburned areas. If necessary, burned areas may also be used; these are considered sterile. Infusion should be done with crystalloids, preferably Ringer’s lactate solution. To calculate the amount of fluid to infuse, use the Baxter formula: 4 ml/kgKG/%vKOF/24 h.
The first half of the fluid amount is given in the first eight hours after trauma. For smaller burns, the patient must be encouraged to drink to provide the increased volume requirements per os. Patients requiring intravenous volume therapy should be transferred to a hospital.
Transfer criteria/Triage
The following criteria are critical for transfer to a burn center:
- Burn extent >20% of KOF, however, due to existing infrastructure, it may be appropriate to already transfer patients with burns between 10-20% to the burn center
- Inhalation trauma, regardless of burn extent
- High-voltage current or lightning strike injuries, regardless of burn extension.
- Burns with significant secondary injuries, regardless of burn extent
- Infants and elderly patients (>60 years) with burn extension over 10% of KOF.
- All patients with cardiovascular problems, diabetes mellitus, immunodeficiency, or immunosuppression with medications with burn extent greater than 10% of KOF
- II° and III° burns of the hands, face, neck and genitals.
Local treatment
Once the wound has been cleansed and the blisters have been ablated, different local therapies take place depending on the results of the wound assessment.
Superficial burns/scalds: If, after opening the blister, a reddish, moist, painful wound bed with redness that can be pushed away is evident and the accidental event is not a scald, then a dressing with a non-adherent, fluid-transporting material, e.g. with Mepitel® – a silicone-coated, transparent and flexible polyamide net – can be applied immediately. An absorbent dressing is applied over this with sterile compresses. This semi-occlusive dressing can be left in place for up to ten days unless the patient complains of pain or there is a suspected wound infection. Since this therapy regime does not expose the burn wound to air, pain is reduced and the thickness of the dressing does not allow bacterial contamination. If the accident mechanism is based on scalding, the burn wound must be reevaluated 24 hours posttraumatically. Scalds are far more profound than burns afterward, and a wound that is judged to be second-degree superficial immediately posttraumatically may meet the criteria for profound damage the very next day. For this reason, a dressing with Ialugen Plus® ointment or gauze is applied here, but it must be changed daily. Ialugen Plus® contains silver sulfadiazine and hyaluronic acid. On contact with wound secretions, silver sulfadiazine dissociates and the silver acts on the surface, whereas the sulfonamide penetrates into the eschar. Silver sulfadiazine has bacteriostatic and bactericidal activity, somewhat better for Gram-negative than Gram-positive germs. Hyaluronic acid has a modulating effect during the inflammatory phase of wound healing and accelerates the formation of granulation tissue and re-epithelialization. If the burn wound remains superficial, it can be changed to a Mepitel® dressing – if it is post-burn, surgical therapy should be evaluated.
For burns on the face, the use of Hexacorton® spray is particularly suitable. The foam is applied several times a day. At first, this is a damp, rather unsightly affair. However, the applied foam subsequently forms a dry scab over several days and thus provides good protection against wound infections. It is hardly permeable for bacteria and water vapor, so that bacteria already present on the wound and those that are located in the depth at the hair follicles do not find a breeding ground and cannot grow in the dry environment. The burn wound therefore heals unaffected by mechanical and infectious disturbances under the protective scab, which gradually falls off itself after ten days.
Deep burns: In pediatric and adult surgery, Suprathel® – an alloplastic absorbable skin substitute consisting of polylactic acid – is often used for middermal burns, i.e. burns that are too deep for grade 2a and too superficial for grade 2b. This can be left on the burn wound until it heals. As the epithelialization of the wound progresses under Suprathel®, this alloplastic skin substitute is “shed” and can be successively cut off at the edges.
Deep burns require surgical necrectomy, most commonly by tangential excision. The gold standard of wound coverage is then still split skin. In grade 3 burns, there is loss not only of epidermis but also of dermis. This can only be replaced by means of full-thickness skin, which, however, can only be obtained for small areas, or by means of flap plasty. If the dermis, which is responsible for suppleness, resistance, heat regulation and elasticity, is missing, the scarring typical of deep burns occurs with the well-known aesthetic and functional deficits. For this reason, it is sometimes necessary to resort to synthetic dermis equivalents such as Integra®. Integra consists of bovine collagen fibers and glycoaminoglycans. Over a period of three weeks, the patient’s own fibroblasts and endothelial cells sprout into this scaffold. The resulting neodermis can be covered with autologous split skin.
If more than 50% of the KOF is burned, further therapeutic concepts have to be applied because there is not enough autologous split skin available. Allogeneic donor skin and autologously cultured keratinocytes offer temporary and permanent skin replacement, which is time-consuming and technically complex to produce.
Current developments
Thanks to recent developments, it is now possible to prepare a keratinocyte suspension directly intraoperatively from a skin biopsy for smaller wound areas (ReCell®).
A phase I trial is underway at the Children’s Hospital Zurich on the use of autologous skin grafts grown from a patient-derived skin biopsy. At the University Hospital Zurich, stem cell research and the use of keratinocyte cultures, which are produced according to GMP criteria in collaboration with the Swiss Center for Regenerative Medicine, are now increasingly being used for adults.
Aftercare
Transplanted skin areas require consistent compression therapy using compression garments during the first postoperative year to reduce hypertrophic scar healing. Since the sebaceous glands are not transplanted in wounds covered with split-thickness skin, the covered areas tend to become very dry, and thermoregulation is also disturbed. Regular care of the skin with lipid-replenishing ointments (e.g. Bepanthen®) is therefore essential. In addition, the skin must be protected with a sunscreen cream with SPF 50.
For functionally limiting scars, which are, for example, unstable and repeatedly tear or show a contracture, various therapeutic measures can be considered. In our specialized scar consultation hours, the various forms of therapy such as silicone-containing patches, cortisone infiltrations, percutaneous collagen induction, stem cell therapy, laser treatment and surgical corrections are discussed with patients and offered by specialists.
For outpatient controls
Plastic surgery consultation scheduling: 044 255 27 38
For transfers to the burn intensive care unit or information about the duty physician for plastic surgery: 044 255 15 25
Literature:
- Raffoul W, Berger M: Burns: from scalding to electrical trauma – definitions and treatment. Switzerland Med Forum 2006; 6: 243-251.
- Enoch S, Roshan A, Shah M: Emergency and early management of burns and scalds. BMJ 2009; 338: b1037.
- Agarwal P, Sahu S: Determination of hand and palm area as a ratio of body surface area in Indian population. Indian J Plast Surg 2010 Jan; 43(1): 49-53.
- Jakobsson O, Arturson G: The effect of prompt local cooling on oedema formation in scaled rat paws. Burns Incl Therm Inj 1985; 12(1): 8-15.
- Lönnecker S, Schoder V: Hypothermia in burn injured patients-influences of prehospital treatment. Surgeon 2001; 72: 164-167.
- Tobalem M, et al: First-aid with warm water delays burn progression. JPRAS 2013; 66: 260-266.
HAUSARZT PRAXIS 2015; 10(3): 32-36











