Which nutritional concepts are most effective in terms of prevention and treatment of obesity and long-term weight maintenance? What can pharmacotherapies do for weight loss and what are the critical factors for success? These were the questions addressed at the Diabetes Congress 2022 of the German Diabetes Society (DDG) in Berlin in connection with the discussion of new therapies for the treatment of severe obesity.
Excessive and continuous consumption of high-carbohydrate and high-fat foods and beverages leads to obesity and thus to an increased risk of developing insulin resistance type 2 diabetes or cardiovascular disease. However, according to Prof. Dr. Annette Schürmann of the German Institute of Human Nutrition (DIfE), positive effects can be achieved through longer breaks in food intake, i.e. interval fasting. If food intake is reduced to a time window of 4-10 hours daily, the main result is that insulin no longer needs to be released continuously. Lipid metabolism is boosted and more fats are burned. Another important effect is the optimization of the circadian rhythm, which is often disturbed in obesity.
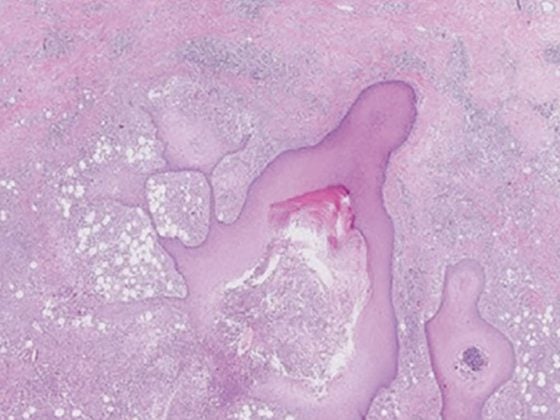
Overall, intermittent fasting can cause body weight to reduce, as well as the fat mass of the body, especially visceral fat. And even without weight reduction, fasting has a beneficial effect on high blood pressure, as well as blood lipid levels, inflammatory processes, oxidative stress and sleep quality. In addition, fasting improves glucose levels and insulin resistance, as well as β-cell function. According to Schürmann, the effect on the liver is also interesting. Glucocorticoids increase. Macrophages secrete less TNFα. Hepatic macrophage glucocorticoid receptor regulates ketogenesis during fasting. Via its activation, PPARα-regulated genes are activated and TNF is inhibited. Apparently, fasting overall is an alternative to restrictive calorie reduction.
Studies on intermittent fasting
The positive effects mentioned were shown, among others, in a study in which one of two participating groups of participants received three meals in a time window of 12 hours, while the other group also ate three identical meals in a shorter time. An additional positive effect was that the subjects felt less desire to eat snacks in the evening as they fasted longer. Another study investigated the effect of intermittent fasting on subjects with metabolic syndrome over three months. Participants initially ate as usual for a period of 14 hours, with only 10 hours without food intake. Subsequently, the time windows were swapped in favor of a fasting period of 14 hours. In addition to weight reduction, the participants in this study also showed a reduced waist circumference and decreasing glucose peaks. According to Schürmann, a 14-hour fasting period could therefore be a suitable additional treatment for patients with metabolic syndrome.
Basically, the type of interval fasting can be designed differently. For example, by intermittent fasting every 2nd day, by a “5 to 2 diet” where calorie intake is reduced to daily 500-600 kcal two days a week, or by fasting mimicking, a calorie reduction to 750-1090 kcal 5 days a month. Forms such as “time restricted eating”, in which no food is eaten for 14 or 16 hours, can be integrated well into everyday life. According to studies, however, it is not worthwhile to further increase the time window for fasting, as this hardly improves the parameters.
If weight reduction is the primary goal, all forms of intermittent fasting require that an energy deficit be achieved for this purpose. And possible side effects such as feelings of weakness, headaches, and dry mouth should not be concealed, Schürmann says.
High protein diet to prevent muscle loss
Losing body fat often means losing muscle mass, said Prof. Dr. Knut Mai of Charité Berlin. However, muscle mask was metabolically valuable tissue. However, there is no loss of muscle mass in weight loss achieved under high-protein diets, he said. Basically, proteins boost energy expenditure, also by promoting thermogenesis after eating, and they provide a lasting feeling of satiety. Patients with type 2 diabetes showed, among other things, improved glucose metabolism and improved liver fat values. There were hardly any differences with regard to the use of proteins of animal or plant origin.
Pharmacotherapy for obesity
Obesity is a disease that affects about 20 million people in Germany. According to the Federal Office of Public Health (FOPH), around 42 percent of the adult population in Switzerland is overweight, and 11 percent of them are obese. Lifestyle changes don’t always help. Prof. Dr. Arya M. Sharma explained why we should also use drugs in obesity with a view to type 2 diabetes. Biological predisposition, food production, social conditions, eating behavior, urban development, psyche and lack of exercise are among the causes of the disease. According to Sharma, it is primarily genetic predisposition that determines susceptibility to obesity. Restrictive food intake either does not help at all in the long term or only with great discipline, as the body is geared to regain lost weight. Surgical interventions offer good chances for sustainable weight reduction, but there is a lack of capacity for this in the case of widespread diseases. A treatment gap that drug therapy can fill.
However, as Bernd Schultes, Metabolism Center St. Gallen, explained, even surgery often does not grant permanent weight reduction. The results are highly individual. 20-25 percent of sufferers failed to lose enough weight even with gastric bypass. Here, too, drug therapy is seen as a source of hope. Because bariatric surgery patients have been largely excluded from pivotal trials of obesity medications, there are limited data in this regard, although they suggest that the effect is similar to that seen in non-operated patients. As in Germany, only a few drugs have been approved for the treatment of obesity in Switzerland to date. Currently, orlistat and liraglutide are primarily used. Semaglutide 2.4 mg, a GLP-1 receptor agonist, is considered a hopeful candidate. The 20% weight loss possible with this drug is close to the bariatric surgery range of 15-35% weight loss. In Switzerland, Rybelsus with the active ingredient semaglutide was approved for the first time by Swissmedic on March 24, 2020 for the oral treatment of adults with inadequately controlled type 2 diabetes mellitus as an adjunct to diet and exercise.
Congress: DDG 2022
CARDIOVASC 2022; 21(3): 30-31