Migraine is the most common severe headache that prompts patients to see a primary care physician. The suffering of those affected is often considerable. For several years, a new group of drugs has been available for preventive treatment. As recent studies have shown, the use of antibodies directed against CGRP can also break the vicious cycle of analgesic overuse headache.
Migraine is one of the most important primary headache disorders [1]. In Switzerland, more than one million inhabitants are affected. The pulsating headache attacks, which usually occur on one side, are a high burden. WHO ranks the disease as the second leading cause of years of life with disability [2,3]. On the one hand, migraine often leads to temporary disability, but on the other hand, it is also associated with other diseases such as depression and vascular diseases [4].
Recognize and correctly classify migraine attacks
The International Classification of Headache Disorders (ICHD-3) distinguishes 200 different types of headache [5]. If secondary causes for the headache can be ruled out, further delineation is possible based on the duration, type and intensity of the headache. Also classified as primary headaches are tension-type headaches and trigeminal autonomic headache disorders [5]. In particular, the distinction between migraine and tension headache is not always easy [6]. A headache diary is useful for recording when and how often the pain occurs and what accompanying symptoms accompany it. A single migraine attack is usually over after a maximum of 72 hours, but tension-type headaches can last from 30 minutes to seven days if left untreated. Pain character and intensity also differ: in migraine, the pain tends to be throbbing, pulsating, or pounding, while in tension-type headache, the pain tends to be dull, pressing, or pulling. A migraine attack usually extremely restricts normal activity, which is not necessarily the case with tension-type headaches. A very important criterion is the typical occurrence of nausea and vomiting during migraine attacks, as well as sensitivity to light and noise. Nausea and vomiting do not occur with tension-type headache, while sensitivity to light or noise is possible but not typical.

“Status migraenosus” – a vicious circle
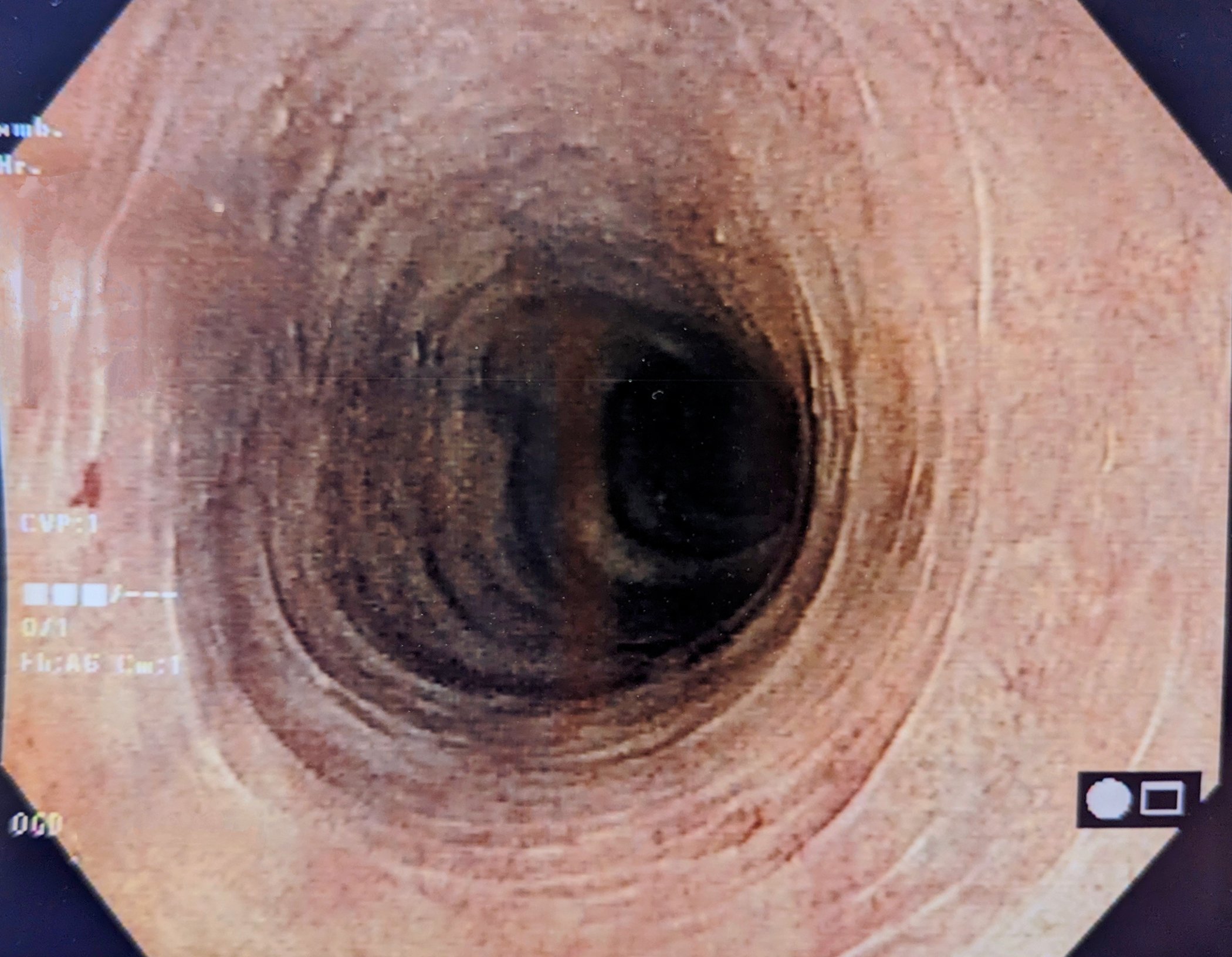
Especially in patients with frequent migraine attacks, conventional painkillers are often not effective or may even have counterproductive effects if used excessively. Because used too often, it can trigger or worsen headaches. This also applies to special migraine medications, so-called triptans, which often lead to headaches if taken more than 10 days per month. In everyday clinical practice, however, it is common for patients with migraine to have to take headache medication on significantly more days because they cannot otherwise stand the pain. However, as a result of medication overuse, the frequency of headache days increases [7]. In this context, one also speaks of “status migraenosus” [8] (Fig. 1). When the triptan level drops, the migraine returns after 12 to 24 hours. Subsequently, the patient repeats the triptan intake and the migraine pain temporarily subsides. But the effect is always less and less long-lasting. The pain-free periods continuously decrease, the pain increases irritability and tension and leads to a performance-reducing lack of drive and energy. Migraine prophylaxis with monoclonal antibodies can break this vicious circle. This is shown by post-hoc analyses of two large randomized trials with humanized monoclonal antibodies directed against CGRP “Calcitonin Gene-Related Peptide” (box) .
|
The neuropeptide CGRP as a therapeutic target. The currently available monoclonal antibodies for the prophylaxis of migraine specifically target the “Calcitonin Gene-Related Peptide” (CGRP) and thus attack a mechanism central to the pathophysiology of migraine (Fig. 2) [11]. The neuropeptide CGRP has vasodilatory and proinflammatory properties and plays a central role in triggering migraine. The antibodies have a long half-life and correspondingly a long dosing interval. They are usually injected subcutaneously. One agent is administered as an intravenous infusion. The most common potential adverse effects include injection site reactions. The first agent targeting CGRP to be approved in Switzerland in 2018 was the CGRP receptor inhibitor erenumab (Aimovig®). This was followed by the CGRP inhibitors fremanezumab (Ajovy®) and galcanezumab (Emgality®) [13]. With the Swissmedic approval of Eptinezumab (Vyepti®), another representative of this group of drugs has been available since 2021. |
Antibody prophylaxis: reduction of migraine days and analgesics.
The post-hoc analyses of the HALO trial and the PROMISE-2 trial evaluated data from patients who had medication-overuse headache-defined as taking triptans or ergot derivatives for more than 10 days per month or taking other analgesics for more than 15 days per month [7].
Subgroup analysis of the HALO study showed that in patients with frequent migraine attacks and medication overuse at the time of study inclusion, fremanezumab significantly reduced the number of headache days, with both quarterly and monthly dosing [9]. The number of study participants who no longer overused medication as a result of antibody therapy halved in the group that received the “migraine injection” quarterly (decrease of 55.2%), and decreased even further with monthly administration (decrease of 60.6%).
Eptinezumab also proved very successful in reducing migraine days in patients with frequent migraine attacks and painkiller overuse. Analysis of the PROMISE-2 study [10] found that patients who had medication overuse at study entry had an average of 16.7 migraine days and that this number reduced to 8 days 24 weeks after initiation of therapy at both treatment doses (100 mg vs. 300 mg), also a reduction by half.

Effective for episodic and chronic migraine
In a statement, the German Neurological Society (DGN) and the German Migraine and Headache Society (DMKG) state that monoclonal antibodies against CGRP (eptinezumab, fremanezumab, and galcanezumab) or against the CGRP receptor (erenumab) are superior to placebo in the prophylactic treatment of both episodic and chronic migraine [7,12].
For episodic migraine, the reduction in migraine days per month ranges from 2.9 to 4.7 days. The 50% response rate at 3-6 months ranged from 30-62 vs. 17-38% with placebo. Efficacy can be evaluated within 4-8 weeks [7,12]. For chronic migraine, the reduction in migraine days per month ranges from 4.3 to 6.6 days. The responder rate at 3 months ranges from 27-57% vs. 15-40% with placebo [7,12].
Literature:
- Swiss Headache Society (SKG): Therapy recommendations for primary headache. 2021, Edition 10.1, fully revised, www.headache.ch (last accessed Feb. 16, 2022).
- Merikangas KR, et al: Magnitude, impact, and stability of primary headache subtypes: 30 year prospective Swiss cohort study. BMJ 2011; 343: d5076; doi: 10.1136/bmj.d5076
- Global burden of disease collaborators, Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017; 390: 1211-1259.
- Bigal ME, Lipton RB: The epidemiology, burden, and comorbidities of migraine. Neurol Clin 2009; 27: 321-334.
- IHS Classification, IHCD, https://ichd-3.org/de (last accessed Feb. 16, 2022).
- Migraine: forms, symptoms, variants, Kiel Pain Clinic, https://schmerzklinik.de/service-fuer-patienten/migraene-wissen/formen (last accessed Feb. 16, 2022).
- “CGRP antibodies may provide a pathway out of analgesic overuse in migraine!”, German Society of Neurology, 11/06/2020, https://dgn.org/, (last accessed 02/16/2022).
- Kiel Pain Clinic, Status migraenosus, https://schmerzklinik.de/status-migraenosus-wenn-die-migraene-einfach-nicht-aufhoeren-will (last accessed Feb. 16, 2022).
- Silberstein SD, et al: The impact of fremanezumab on medication overuse in patients with chronic migraine: subgroup analysis of the HALO CM study. J Headache Pain 2020; 21: 114, https://doi.org/10.1186/s10194-020-01173-8
- Silberstein SD, et al: Eptinezumab for the prevention of chronic migraine: efficacy and safety through 24 weeks of treatment in the phase 3 PROMISE-2 (Prevention of migraine via intra-venous ALD403 safety and efficacy-2) study. J Headache Pain 2020; 21(1): 120. Published 2020 Oct 6.
- Dicheva-Radev S, et al: Monoclonal antibodies for the prophylaxis of migraine: efficacy and place value, www.akdae.de (last accessed Feb 16, 2022).
- Supplement to Guideline 030/057: Therapy of Migraine Attacks and Prophylaxis of Migraine, German Society of Neurology (DGN)/ German Migraine and Headache Society (DMKG), https://dgn.org/leitlinien (last accessed Feb. 16, 2022).
- Swissmedicinfo: Medicinal product information, www.swissmedicinfo.ch (last accessed 16.02.2022).
HAUSARZT PRAXIS 2022; 17(3): 38-40
InFo NEUROLOGY & PSYCHIATRY 2022; 20(2): 26-28.