Immunotherapy using checkpoint inhibitors has become an indispensable part of the treatment of non-small cell lung cancer. Nevertheless, there is room for improvement – and potential – in the area of predictive markers, as a study by the University Hospital of Tübingen recently published in the journal nature communications shows.
One in five non-small cell lung cancers (NSCLC) responds to checkpoint inhibitor therapy. Thus, treatment with agents directed against CTLA4, PD-L1 and PD-1 is now part of the therapeutic standard. However, identifying those patients who will benefit from high-cost immunotherapeutic treatment remains a major challenge. So far, mainly PD-L1 expression of tumor cells has been used to predict response, which is also reflected in the approvals of the different compounds. For example, first-line immunotherapy with atezolizumab in combination with paclitaxel and carboplatin is approved only for those tumors that have PD-L1 expression of ≥1%. If this criterion is not met, Nab-paclitaxel must be given instead of paclitaxel [1]. Pembrolizumab may even be used as first-line monotherapy with a tumor proportion score (TPS) of ≥50% in the metastatic, ALK- and EGFR-negative setting. If the TPS is below 50%, chemotherapy is also used [1].
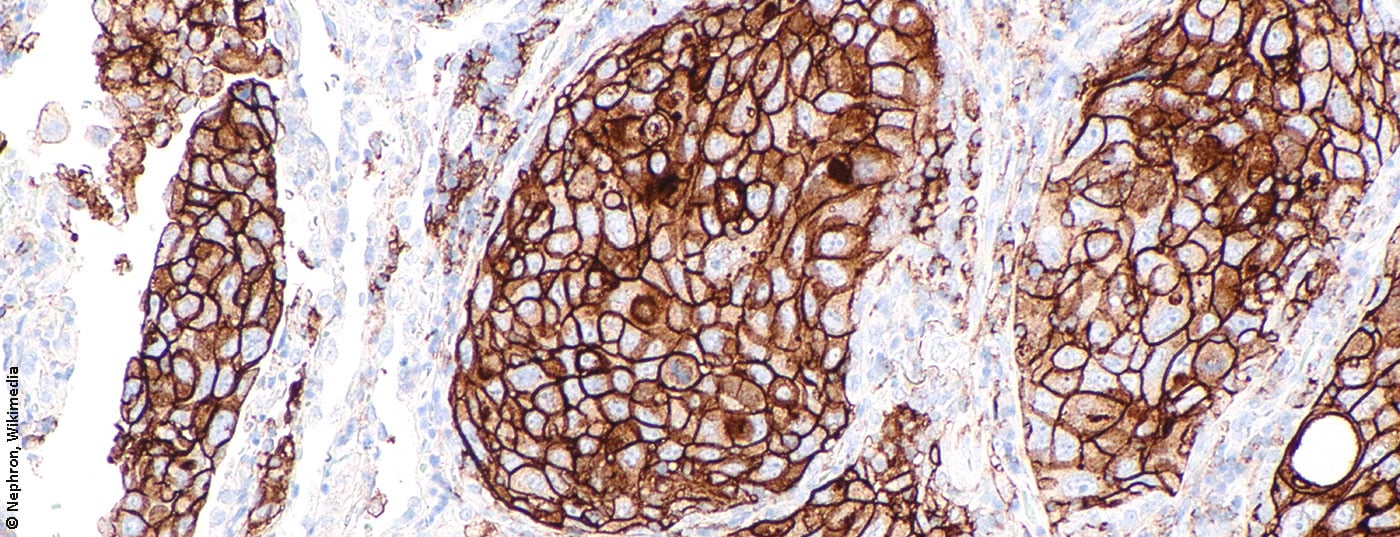
Unfortunately, immunohistochemical determination of PD-L1 expression on tumor biopsies – the previous standard – is prone to error and does not reliably correlate with treatment response, not least because of intratumoral heterogeneity, which cannot be satisfactorily mapped with a biopsy. Other markers, such as tumor mutational burden (TMB), microsatellite instability (MSI), and infiltration with CD8+ T cells, have so far failed to gain acceptance despite their superiority in some studies.
PD-L1 in platelets as a promising approach.
An alternative to immunohistochemical PD-L1 determination, which seems to better reflect the collective PD-L1 expression of the tumor and may be of higher predictive value, at least according to preclinical data, is platelet PD-L1 content. For example, in a study published in December 2021, researchers from Tübingen concluded that PD-L1 proteins are transferred from platelets to tumor cells through contact with the former – a process that is dependent on fibronectin 1, integrin α5β1, and GPIbα. The result: platelets from NSCLC patients, like tumor cells, express functional PD-L1, which, like that on the tumor surface, is able to suppress T-cell activity and thus could also play a role in immune evasion of the tumor and progression of the disease.
From this finding, the authors developed an algorithm to calculate the so-called activation independent adjusted PD-L1 payload of platelets (pPD-L1Adj.). Those patients with a low pPD-L1Adj. lived a median of 43 months, compared with only 14 months in the highest pPD-L1Adj. group. Particularly high pPD-L1Adj. was found in advanced tumor stage, lymph node involvement, metastases and heavy smokers, among others. Upon response to therapy, a significant reduction in pPD-L1Adj. was demonstrated during the course. The opposite effect – i.e. an increase in pPD-L1Adj. – was seen in those patients in whom the disease progressed during treatment. The predictive power of pretherapeutic pPD-L1Adj. regarding response to immunotherapy was superior to standard histologic quantification of PD-L1 expression. In particular, this could be due to the fact that intratumoral heterogeneity can be mapped more reliably by platelet analysis than by the assessment of individual tumor components based on biopsies. Another advantage of the potential new method is the determination of PD-L1 expression by blood sampling – i.e. without biopsy – and thus less invasiveness. Repeating the analysis depending on disease dynamics would also be easier to perform with the new method.
Whether the results from the study will be confirmed and platelets will be used to predict response to checkpoint inhibitor therapies in the future remains to be seen. The number of patients who could benefit from this is large – after all, about 1.8 million people die of lung cancer every year. Reliable markers can contribute significantly to optimizing therapy and thus reducing this number, as well as to minimizing unnecessary, potentially fatal side effects and reducing healthcare costs. The latter aspect is particularly relevant given the large number of NSCLC patients and the high cost of immunotherapies. A multicenter study is planned as the next step. We remain curious.
Source: Hinterleitner C, et al: Platelet PD-L1 reflects collective intratumoral PD-L1 expression and predicts immunotherapy response in non-small cell lung cancer. Nature Communications. 2021; 12(1): 7005.
Literature:
- Swissmedic drug information: www.swissmedicinfo.ch (last accessed 01/25/22).
InFo ONCOLOGY & HEMATOLOGY 2022; 10(1): 30.
InFo PNEUMOLOGY & ALLERGOLOGY 2022; 4(2): 40.