Specific immunotherapy (SIT) is the only disease-modifying and curative form of therapy for the treatment of immediate-type allergies. In contrast to symptomatic pharmacological therapies, SIT pursues the goal of sustained immunological tolerance to the allergens. Current data suggest that an accelerated dosing regimen of subcutaneous immunotherapy (SCIT) with grass pollen allergen extracts is also effective and safe.
Immediate-type allergies (type I allergies) are associated with IgE-mediated mediator release (including histamine and cytokines). Symptoms generally appear within 30 minutes of allergen exposure. With few exceptions, the triggering allergens of the type I reaction are proteins (e.g., pollen, mites, animal dander, molds, foods, and insect venoms) [1]. Pollen allergy is the most common allergic disease in our latitudes. In Switzerland, about 20% of the population is affected [2]. Rhinitis, sneezing attacks and watery eyes are typical symptoms of hay fever. Mucus accumulated in the sinuses can also lead to jaw pain and headaches. If a diagnosis is suspected, various skin and blood tests can provide clarity in addition to a comprehensive medical history. If a pollen allergy is not treated over a long period of time, there is an increased risk of developing allergic asthma (“floor change”). Symptomatic treatment can provide relief, but does not provide a cure.
SIT is the only causal treatment option
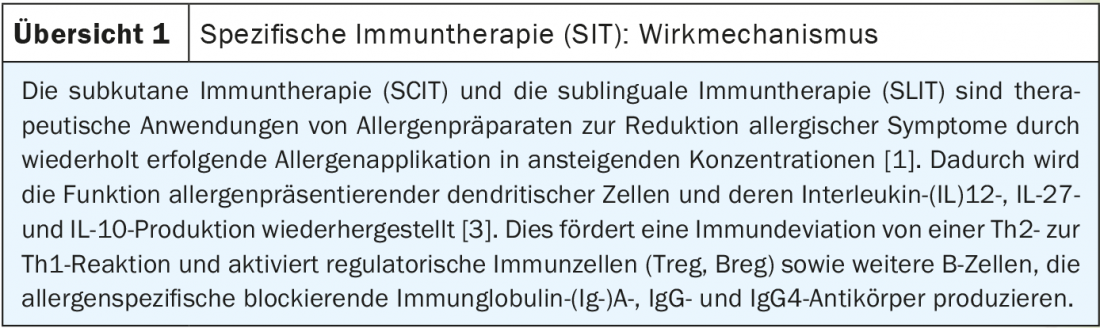
In addition to symptomatic treatment of a pollen allergy, there is the possibility of desensitization by means of allergen-specific immunotherapy (SIT). To date, this is the only causal treatment option for the therapy of type I allergies. The aim is to influence the immune system in such a way that it no longer overreacts on contact with the corresponding allergen (overview 1) . To achieve this, allergen extracts are repeatedly administered (subcutaneously or orally) in increasing concentrations. Both subcutaneous (SCIT) and sublingual immunotherapy (SLIT) inhibit early and late reactions after allergen exposure [3]. The clinical indication of SIT is given in case of proven IgE-mediated sensitization with associated clinical symptoms, whereby respective contraindications should be considered [1,3]. To this end, skin tests or provocation tests are first used to determine which allergens the body overreacts to. Intracutaneous, prick, and provocation tests for the detection of type I allergies (IgE-mediated, immediate type) usually use unmodified allergen extracts from biological source materials in solution [1].
Well documented efficacy and safety
In Switzerland, the approval of a new allergen preparation for SIT is subject to regulations issued by Swissmedic [1]. A proven positive benefit-risk ratio is crucial for approval. The recommendations and principles described by the Committee for Medicinal Products for Human Use (CHMP) are considered authoritative with respect to the current state of science (“Guideline on the Clinical Development of Products for Specific Immunotherapy for the Treatment of Allergic Diseases”) [4]. In the past decades, the efficacy and safety of SIT have been extensively documented [5]. Progress in recent years has been mainly based on better standardization of allergen extracts, development of modified therapeutic extracts, and molecular biological characterization of natural allergens [6]. In subcutaneous immunotherapy (SCIT), the allergen extract is injected subcutaneously into the skin at defined intervals over a longer period of time, sometimes in increasing doses. Several systematic reviews and meta-analyses by the European Academy of Allergy and Clinical Immunology (EAACI) support the efficacy of SCIT in allergic rhinoconjunctivitis [7]. This is operationalized by means of various scores as primary and secondary target parameters. Symptom reduction and lower medication consumption are relevant outcome parameters of successful SIT. Both measures are incorporated into the primary study objectives for pivotal trials as part of the symptom-medication scores (phase III field studies) [4,9].
SCIT in grass pollen allergy – convincing study results
In a study of the efficacy of grass pollen SCIT, Corrigan et al. show significant differences in symptom and medication scores in favor of SCIT in the first and second year of the follow-up period in placebo comparisons (26.6%, p=0.028 and 48.4%, p=0.018, respectively) [10]. In a retrospective study published in 2021 by Berge et al. 70% of the 128 patients who received SIT with grass or birch pollen allergen extracts reported symptom reduction [11]. The investigation of a possible association between allergen-specific IgE concentrations or demographic characteristics before treatment initiation and the outcome of therapy did not reveal any statistically significant findings.
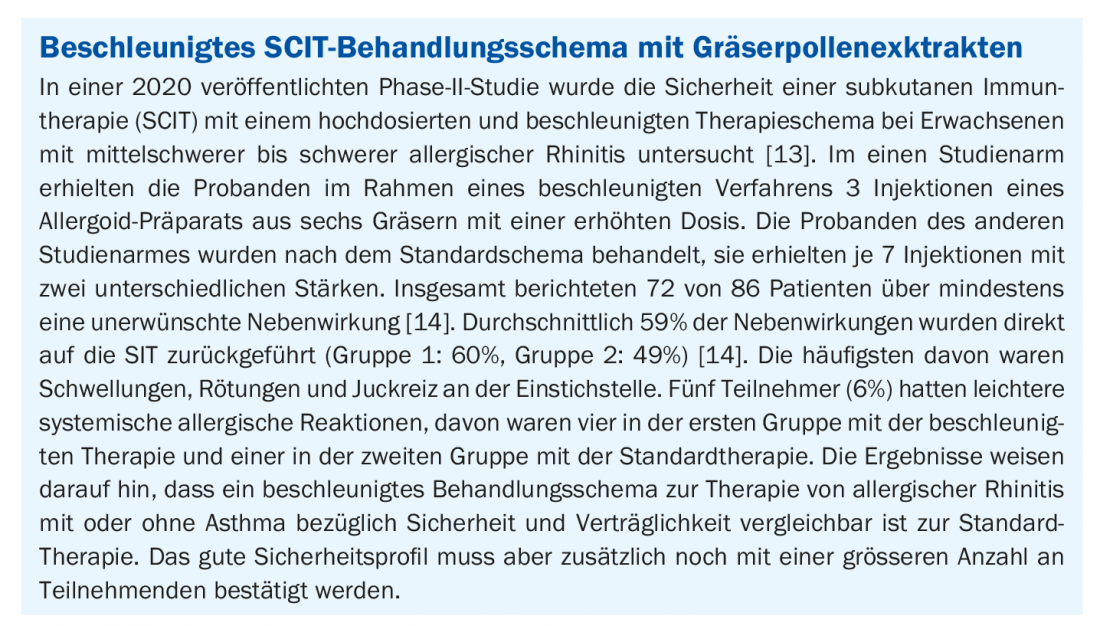
Chaker et al. succeeded in demonstrating in a study of 122 adult patients with allergic rhinitis with or without asthma that an accelerated 4-dose escalation regimen with grass pollen (starting with 200 therapeutic units) is feasible with a favorable safety profile comparable to the standard 7-dose escalation (starting with 100 therapeutic units) [12]. In both study conditions, only mild side effects were reported (grade 1 or 2 according to the World Allergy Organization). The phase II results of an accelerated SCIT therapy regimen with grass pollen extracts published last year also show a favorable safety profile(box). It is now important to await further study data from larger subject collectives.
Literature:
- Swissmedic: HD Pathway, Allergen Preparation Authorization, www.swissmedic.ch (last accessed 05/12/2021).
- Aha Allergy Center Switzerland, www.aha.ch/allergiezentrum-schweiz (last accessed May 12, 2021).
- Mahler V, Kleine-Tebbe J, Vieths S: Immunotherapies of allergy: Current status. Federal Healthbl 2020; 63: 1341-1356.
- EMA: Committee for Medicinal Products for Human Use (CHMP). Guideline on the clinical development of products for specific immunotherapy for the treatment of allergic diseases, 2008.
- Muraro A, Roberts G (Eds): Allergen Immunotherapy Guidelines Part 1: Systematic reviews. Zurich: European Academy of Allergy and Clinical Immunology (EAACI), 2017.
- Valenta R, et al: Recombinant allergens for allergen-specific immunotherapy: 10 years anniversary of immunotherapy with recombinant allergens. Allergy 2011; 66: 775-783.
- Dhami S, et al: Allergen immunotherapy for allergic rhinoconjunctivitis: A systematic review and meta-analysis. Allergy 2017; 72: 1597-1631.
- Deutsche AllergieLiga: Weissbuch Allergie in Deutschland: Springer Medizin Verlag GmbH, 4th, revised and expanded edition, 2018.
- Pfaar O, et al; EAACI: Recommendations for the standardization of clinical outcomes used in allergen immunotherapy trials for allergic rhinoconjunctivitis: an EAACI Position Paper. Allergy 2014; 69: 854-867.
- Corrigan CJ, et al; Study Group: Efficacy and safety of preseasonal-specific immunotherapy with an aluminum-adsorbed six-grass pollen allergoid. Allergy 2005; 60(6): 801-807.
- Berge M, et al: Pre-treatment allergen-specific IgE analysis and outcomes of allergen immunotherapy. Eur Ann Allergy Clin Immunol 2021 May 3. Epub ahead of print.
- Chaker AM, et al: An accelerated dose escalation with a grass pollen allergoid is safe and well-tolerated: a randomized open label phase II trial. Clin Transl Allergy 2016; 6(1): 4.
- Kopp MV, et al: Accelerated Dose Escalation with Three Injections of an Aluminum Hydroxide-Adsorbed Allergoid Preparation of Six Grasses Is Safe for Patients with Moderate to Severe Allergic Rhinitis, In: Int Arch Allergy Immunol 2020; 181(2): 94-102.
- Allergieinfo.de, www.allergieinfo.de/allergiker-infos.html (last accessed May 12, 2021).
HAUSARZT PRAXIS 2021; 16(7): 28-29