Salivary gland carcinomas are a rare form of malignancy, however, with high heterogeneity. Therefore, molecular profiling should be used for therapy stratification. Depending on the subentity, different pharmacological interventions may be effective. Nevertheless, surgical intervention is still the treatment of choice.
Salivary gland carcinomas are among the rare tumor diseases with their point of origin in the large glands. Basically, they can appear anywhere there is mucosal tissue, including the lateral margin of the tongue, the palatal arch, or the oral mucosa. Different etiologies are discussed, such as ionizing radiation, occupational causes, or viruses. The tumors are divided into two groups, depending on the outgoing cells into luminal, ductal or acinar cell or albumin cell, myoepithelial cell or basal cell. Mucoepidermoid carcinoma is the most common tumor of the salivary gland and accounts for up to 50% of all cases. Different subtypes are distinguished, with deeper-grade types having mainly glandular and cystic structures whose surface epithelium contains mucos-producing cells. The higher grade the carcinoma becomes, the more lymphoid cells show up. There is a high correlation between infiltration with lymphoid cells and a worsening of prognosis.
Clarification steps in case of suspicion
Often, asymptomatic nodes are located in the cheek area, the angle of the jaw, under the lower jaw, or on the palate. An initial sign of malignancy can be attributed to pain, facial nerve paresis, lockjaw, enlarged ipsilateral lymph nodes, or skin invasion. Following palpation findings that are insufficient on their own, nerve function should be assessed and imaging should be performed. Cytology by fine needle aspiration is the most important cornerstone in diagnostics.
Surgical principles
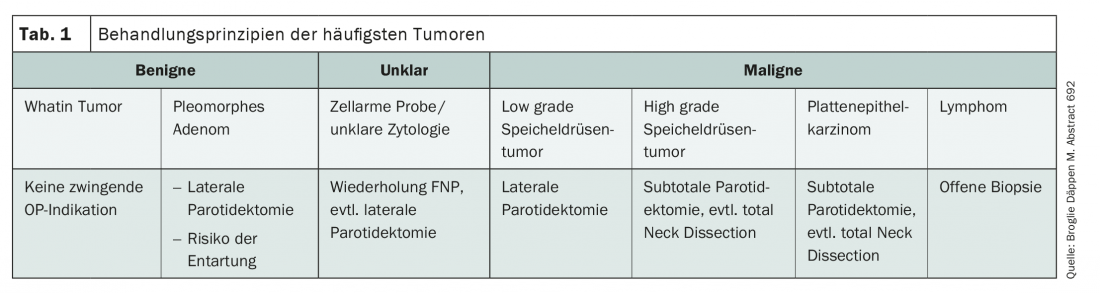
Surgery is the treatment of choice for salivary gland carcinoma. However, the indication and extent of surgery depends on tumor extension, cytology and grading (Tab. 1) . With regard to the nerves, a functional, non-tumor affected facial nerve should be preserved whenever possible. Resection with reconstruction should be performed if the nerve is tumor-involved or walled.
Heterogeneous clinical picture
Salivary gland carcinomas show great heterogeneity in their clinical behavior. Pharmacologically, one can take advantage of this and intervene accordingly. Androgen receptor blockade with a combination of bicalitamide and LHRH agonist, although studied only in small numbers of cases as with all treatment options, has achieved an impressive response rate of 50-65%. Her2 blockade with a combination of docetaxel and trastuzumab showed a 70.2% response in a phase II trial, resulting in a median overall survival of just under 40 months. This treatment should be applied accordingly in patients with Her-2 overexpression. Another option is to use T-DM 1 with an outstanding response rate of 90%. Even though it is very rare, it is still worthwhile to ask the pathologist about the presence of an NTRK fusion product. This is because NTRK inhibition has been shown to result in a high proportion of remissions, which is ultimately reflected in overall survival. For adenoid cystic carcinoma, results from a single-arm study of lenvatinib can be used. In this study, the VEGF tyrosine kinase inhibitor showed remission in 15% of patients and stable disease was achieved in 75%. The median progression-free survival was 17.5 months. These results were confirmed by another study with the tyrosine kinase inhibitor axitinib. The 6-month progression-free survival rate was 73%, and the median progression-free survival of 10.8 months was significantly higher than that of the observation group at 2.8 months.
Chemo-immunotherapy in focus
The introduction of checkpoint inhibtors (CPI) has led to an enrichment of the therapy landscape. In combination with chemotherapy, immunosurveillance can be improved or stimulated. Outcomes in ENT tumors could be improved if sequential therapy with chemotherapeutic combinations that can lead to tumor tissue priming is followed by sequential CPI treatment.
InFo ONCOLOGY & HEMATOLOGY 2020; 8(5): 34 (published 10/19/20, ahead of print).