Necrotizing fasciitis is a rare life-threatening bacterial infection of the subcutaneous tissue and fascia. Prompt surgical debridement and early intensive treatment with antibiotics are critical. Vacuum therapy or the negative pressure instillation therapy method based on it can be used for wound conditioning after necrectomy.
Prompt recognition and treatment of necrotizing fasciitis and associated complications can contribute to an increased chance of patient survival, emphasized Prof. Klaus-Dieter Schaser, MD, University Hospital Dresden (D), in his presentation at the Nuremberg Wound Congress [1,2]. Necrotizing soft tissue infection can be caused by various microorganisms [3]. It is not an infection by a specific bacterium, but an interaction of multiple germs of nonspecific combination, although monomicrobial courses also occur [4]. In the extremities, necrotizing fasciitis is most commonly a result of blunt or penetrating trauma, intravenous drug use, and insect bites. However, intramuscular or subcutaneous injections, bite wounds, burns, muscle strains, or surgery can also promote the entry of germs [4]. Despite advances in treatment options, the mortality rate has remained high at 25-30% over the past thirty years, with only a recent small decrease to approximately 20% reported [5].

Rapid diagnosis required
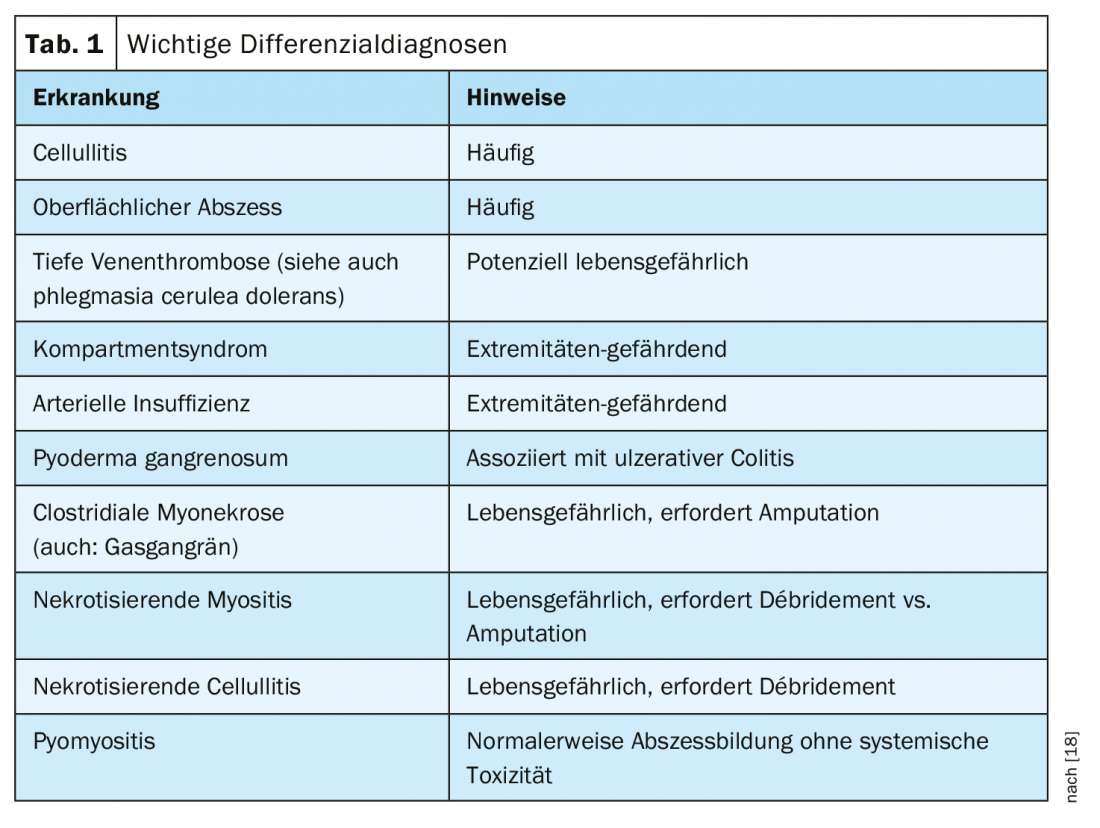
Diagnosis is primarily clinical, and LRINEC scoring (“Laboratory Risk Indicator for Necrotizing Fasciitis”) can be used [6,7] – but it is noted that this should be interpreted in the context of the clinical examination and not considered in isolation [18]. Physical examination and correct classification of clinical manifestations are the most important factors for an early diagnosis of necrotizing fasciitis [3] (overview 1) . For further clarification with an analysis of morphological characteristics, CT and MRI have proven useful [3,8]. Sonography, scintigraphy, and radiography can also be used to obtain information about the type and extent of the necrotizing infection [3]. In addition to extensive necrosis of the fascia with extension to the adjacent skin and severe systemic intoxication with decreased mental status and absence of primary muscle involvement, the following diagnostic criteria are also indicative of necrotizing fasciitis [1,9]: Absence of clostridia in wound swab, absence of causative vascular occlusion, leukocyte infiltration and focal necrosis of fascia as well as surrounding tissues, microvascular thrombosis on internal examination. There are four subtypes of necrotizing fasciitis [2] (overview 2) . Differential diagnoses include cellulitis, deep vein thrombosis, and compartment syndrome (Table 1).

Risk factors influence progression prognosis
The most important factor regarding mortality, besides the timing of surgical intervention, is the type and number of comorbidities [10]. According to some literature sources, the percentage of people affected by necrotizing fasciitis who have diabetes is over 70% [3,11]. Other comorbidities that are risk factors include [1,3]: obesity, alcohol abuse, history of intravenous drug abuse, trauma, skin lesions (chicken pox); chronic ulcers, burns, postoperative wounds, insect bites, immunodeficiencies and HIV, chronic renal failure, cirrhosis of the liver. If necrotizing fasciitis develops into rapidly progressive necrosis of the subcutaneous fat and fascia, it is a life-threatening condition [3]. If left untreated, the prognosis of necrotizing infections is poor and the course is severe [3]. Multidisciplinary treatment is essential when necrotizing fasciitis is suspected. In addition to the primary care physician, these include surgeons, radiologists, microbiologists, physical therapists, and nutritionists. In most cases, prompt, adequate surgical interventions are outcome determinant
Negative pressure instillation therapy as an innovative treatment method
Clinical stabilization can be achieved by radical mechanical debridement (local debridement is usually insufficient). This can be followed by negative pressure wound therapy with instillation (NPWTi). It is an innovative procedure, combining vacuum therapy with automated, controlled delivery and drainage of antiseptic or NaCl solutions for topical wound treatment in the wound bed [12]. Necrotizing fasciitis is one of the surgical-orthopedic indications of this method [12]. The authors of the article published in JDDG point out that the use of a VAT/NPWTi on necrotic scabbed wounds is contraindicated because increasing signs of infection may develop in addition to failure of the wound to heal [12]. In the case of bleeding wounds, sufficient hemostasis must first be initiated before applying a VAT/NPWTi. Special care should also be taken in patients with coagulation disorders.

The active principle of NPWTi: The negative pressure results in an increase in blood flow in the wound and, associated with this, a stimulation of granulation tissue neogenesis. By using less hydrophobic sponges than vacuum therapy, fluid distribution and debris removal from the wound bed is optimized. In addition to a reduction of the wound surface, there is an induction of granulation tissue as well as a reduction of the bacterial colonization of the wounds. Vacuum therapy has long been an established treatment option in wound care. The active principle is based on a hydrophobic, reticular open-cell wound foam with a defined pore size, which is introduced into the wound and fixed with an occlusive film dressing [12]. By sealing the wound airtight, vacuum therapy can permanently extract wound secretions and cellular debris, thereby cleaning the wound.
Source: Wound Congress Nuremberg (D)
Literature:
- Schaser K-D: Necrotizing fasciitis. Slide presentation. Prof. Dr. med. Klaus-Dieter Schaser. Nuremberg Wound Congress, Dec. 06, 2019.
- Morgan MS: Diagnosis and management of necrotising fasciitis: a multiparametric approach. J Hosp Infect 2010; 75(4): 249-257.
- Roje Z, et al: Necrotizing fasciitis: literature review of contemporary strategies for diagnosing and management with three case reports: torso, abdominal wall, upper and lower limbs. World J Emerg Surg 2011; 6(1): 46.
- Illg C, et al: Necrotizing fasciitis, Continuing Education, Reconstructive Surgery, www.dgpraec.de/wp-content/uploads/2019/04/CME_PlastChir_2018_4.pdf
- Bonne S, Kadri SS: Evaluation and Management of Necrotizing Soft Tissue Infections. Infect Dis Clin North Am 2017; 31(3): 497-511.
- Sarani B, et al: Necrotizing fasciitis: current concept and review of the literature J Am Coll Surg 2009; 208(2): 279-288.
- El-Menyar A, et al: The laboratory risk indicator for necrotizing fasciitis (LRINEC) scoring: the diagnostic and potential prognostic role. Scand J Trauma Resusc Emerg Med 2017; 25: 28.
- Xu LQ, et al: Multidisciplinary treatment of a patient with necrotizing fasciitis caused by Staphylococcus aureus: A case report. World J Clin Cases 2019; 7(21): 3595-3602.
- Kujath P, Eckmann C: Necrotizing fasciitis and severe soft tissue infections caused by group A streptococci: diagnosis, therapy, and prognosis. Dt. Physicians Journal 1998; 95: A 408-413. Booklet 8
- Roje Z, et al: Influence of adjuvant hyperbaric oxygen therapy on short-term complications during surgical reconstruction of upper and lower extremity war injury: A retrospective cohort study. Croat Med J 2008; 49: 224-232.
- Gurlek A, et al: Management of necrotizing fasciitis in diabetic patients. J Diabet and Its Comp 2007; 21: 265-271.
- Müller CSL, et al: On the value of negative pressure instillation therapy in dermatology. JDDG 2016; 14(8): 786-796.
- Khamnuan P, et al: Necrotizing fasciitis: risk factors of mortality. Risk Manag Healthc Policy 2015; 8: 1-7.
- Neilly DW, et al: Necrotising fasciitis in the North East of Scotland: a 10-year retrospective review. Ann R Coll Surg Engl 2019; 101: 363-372.
- Misiakos EP, et al: Current concepts in the management of necrotizing fasciitis. Front Surg 2014; 1: 36.
- Das DK, Baker MG, Venugopal K: Risk factors, microbiological findings and outcomes of necrotizing fasciitis in New Zealand: a retrospective chart review. BMC Infect Dis 2012; 12: 348.
- Settelen C, Stebler-Schärz D, Egger B: Guideline Wound Management, University Hospital Basel 2011, www.unispital-basel.ch/fileadmin/unispitalbaselch/Ressorts/Entw_Gesundheitsberufe/Abteilungen/Leitlinie_Wundmanagement/LLgesamtdokument.pdf
- University of Cinncinati: Department of Emergency Medicine, Shock Resuscitation Unit: Necrotizing Fasciitis and the Spectrum of Soft Tissue Infections 2018, September 03. www.tamingthesru.com
- Helman A: BCE 69 Necrotizing Fasciitis, Dr. Anton Helman, Emergency Medicine Cases. https://emergencymedicinecases.com/necrotizing-fasciitis
DERMATOLOGIE PRAXIS 2020, 30(2): 34-35 (published 4/22/20, ahead of print).