CAR-T cells have solved a central problem in cancer therapy – they make tumors visible again to the immune system. The initial successes in B-cell lymphomas are now attracting a broader range of applications. Initial study results are promising.
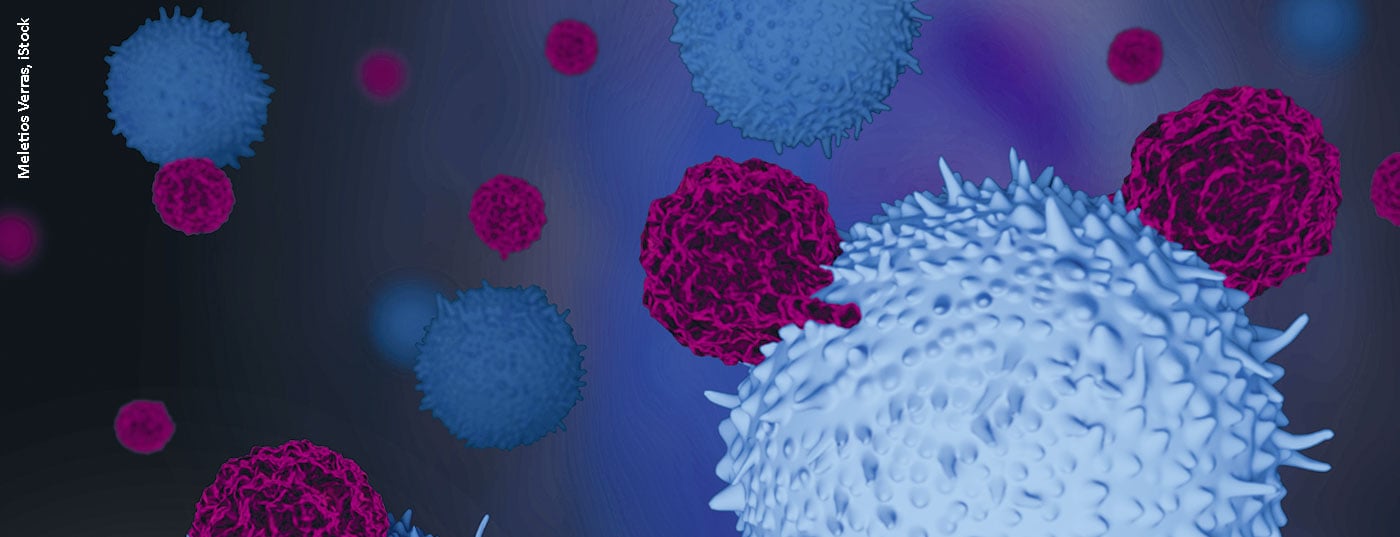
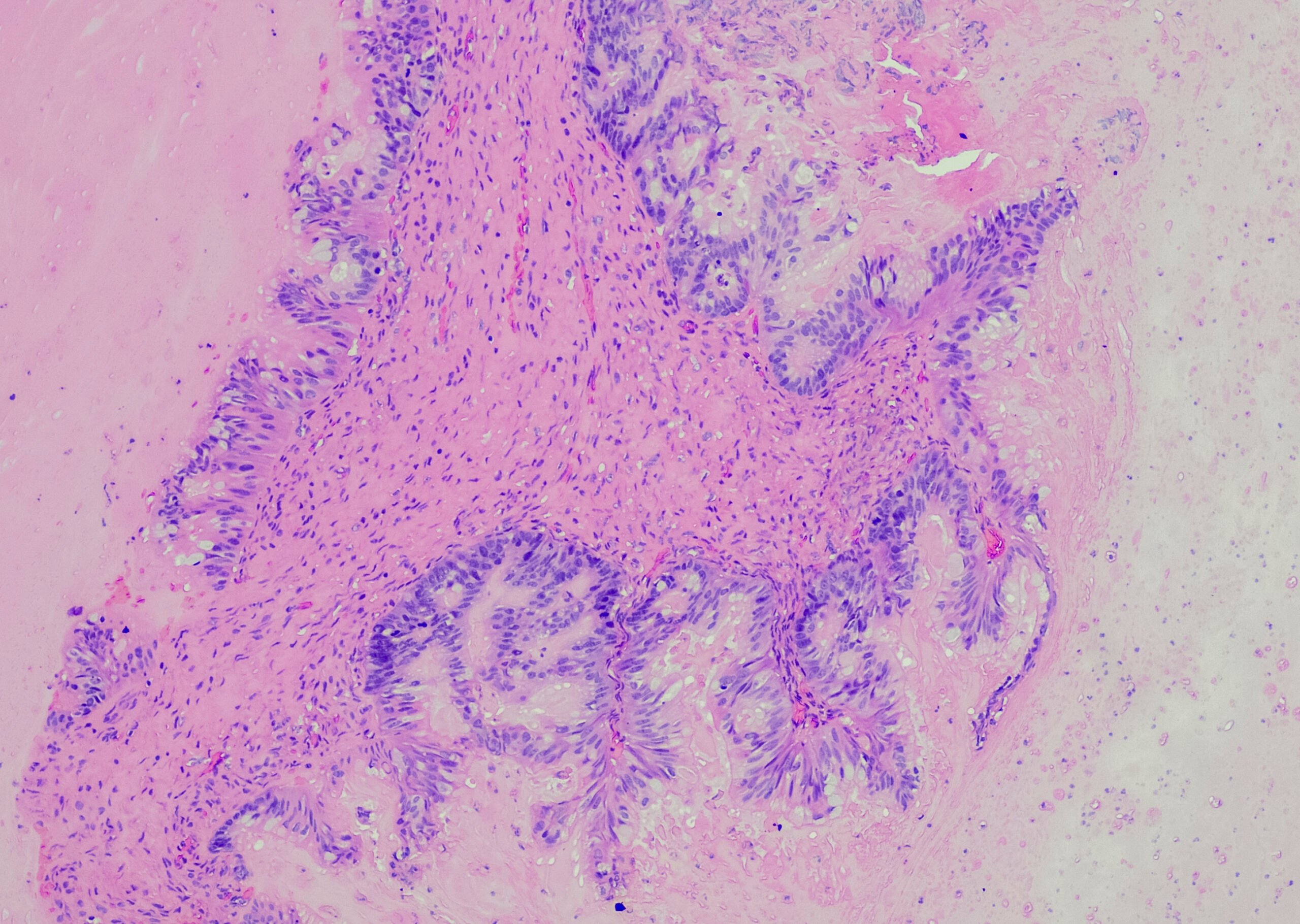
Immunotherapy with CAR-T cells (chimeric antigen receptor T cells) has received much attention in recent years. Spectacular successes have been achieved in patients with advanced tumor disease. CAR-T cells are produced in the laboratory from the patient’s own T lymphocytes. Non-hazardous viruses are used to equip them with the gene for a receptor that – like an antibody – can recognize a selected surface molecule of the cancer cells. These are then reinfused into the person concerned. The CAR T-cell preparations tisagenlecleucel and axicabtagene ciloleucel directed against the antigen CD19 have been approved to date. Both drugs are used in relapsed diffuse large B-cell lymphoma (DLBCL). 40% of patients were able to achieve complete remission in the pivotal trials despite the challenging situation. Recurrent chemotherapy came in at only 7% in a similar patient population. Even two years after treatment with immunotherapy, approximately 40% of patients were still without progression. PD Dr. med. Bastian von Tresckow, Cologne (D), assumes that a relevant proportion of this clientele can be considered cured in the long term. First registry data confirm the effective effect of the treatment also under real-life conditions. Side effects, such as cytokine release syndromes (CRS) and neurotoxicities, tend to occur less frequently than in the pivotal studies and are readily manageable with appropriate experience. Currently, several phase III trials are underway that are evaluating earlier use of CAR T-cell therapy in DLBCL, even in the first relapse,
Explore.
Earlier treatment at ALL
In pediatric hematology, CAR-T cells play a major role in relapsed acute lymphoblastic leukemia (ALL). In addition to tisagenlecleucel, the CD22 antibody inotuzumab and the bispecific antibody construct blinatumomab directed against the CD3 and CD19 antigens are also being tested here. Initial registry data are also available for the already approved CD19 antibody, in which about 40% of patients remained without progression even in the longer term. A large proportion of these without subsequent stem cell transplantation. Earlier deployment is also being considered here. According to Prof. Dr. med. Claudia Roessig, Münster (D), tandem CAR-T cells with simultaneous CD19 and CD22 specificity could be particularly suitable for this purpose in order to reduce the frequency of CD19-negative recurrences.
Focus on therapy optimization
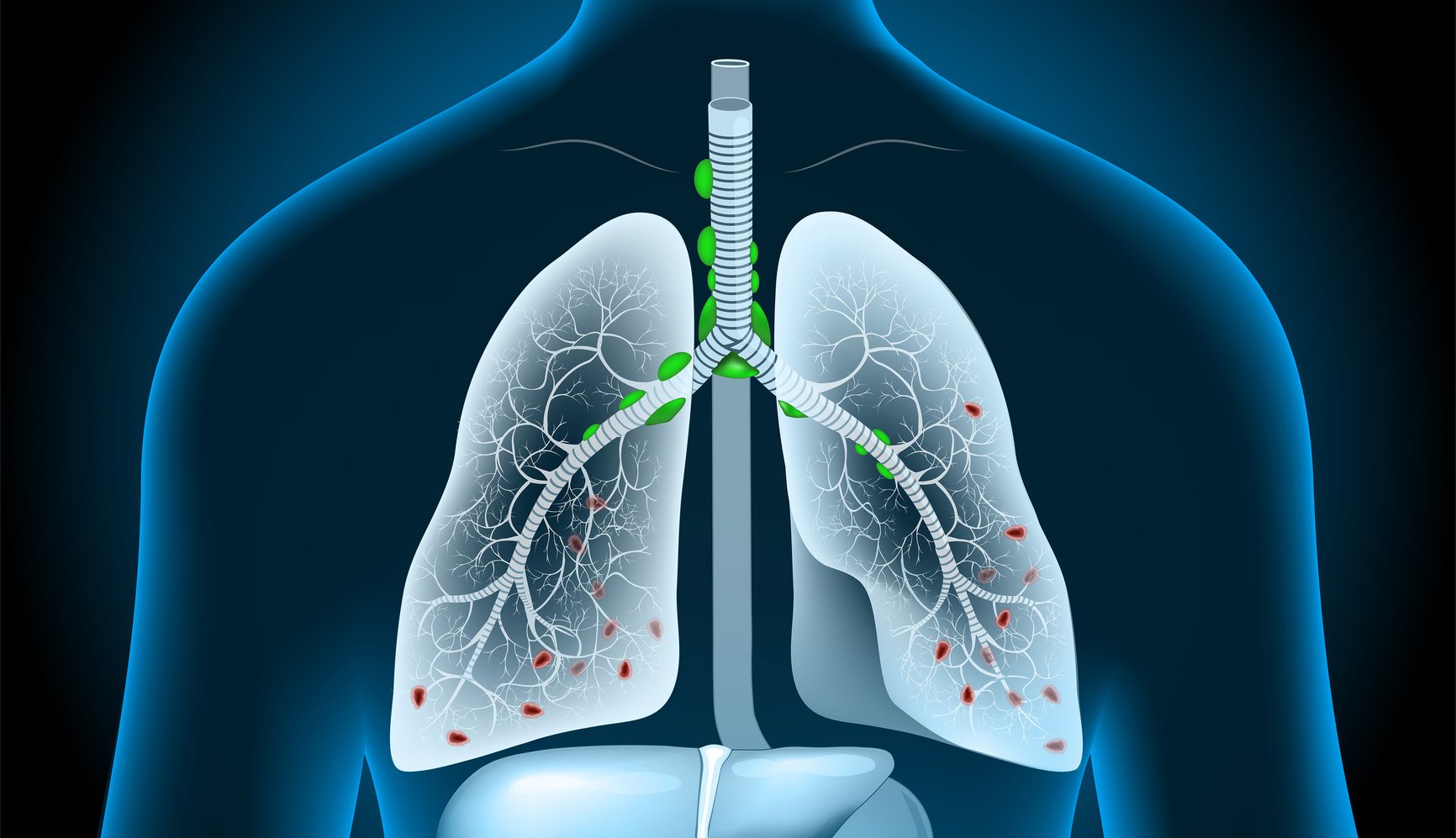
CAR-T cell research has picked up speed. Prof. Michael Schmitt, MD, Heidelberg (D), expects approval of the first CAR T-cell therapy targeting the myeloma antigen BMCA by the end of the year. In addition, other targets, such as the CD33, CD123, FLT3 and SLAMf7 are also in development. In the future, it should also be possible to treat solid tumors in bronchial or breast carcinoma with corresponding ROR1 CARs.
In addition, a great deal of attention is paid to optimizing therapy. For example, on-site manufacturing should be made possible to avoid long transport routes and manufacturing times. Issues related to improved T-cell culture, optimal conditioning and lymphodepletion are also being explored. So it remains exciting.
Source: 34th German Cancer Congress (DKK)
InFo ONCOLOGY & HEMATOLOGY 2020; 8(2): 29.