Quality of life after oncology treatments may also suffer due to altered sexuality. Onco-sexological services are gratefully accepted when initiated by the physician.
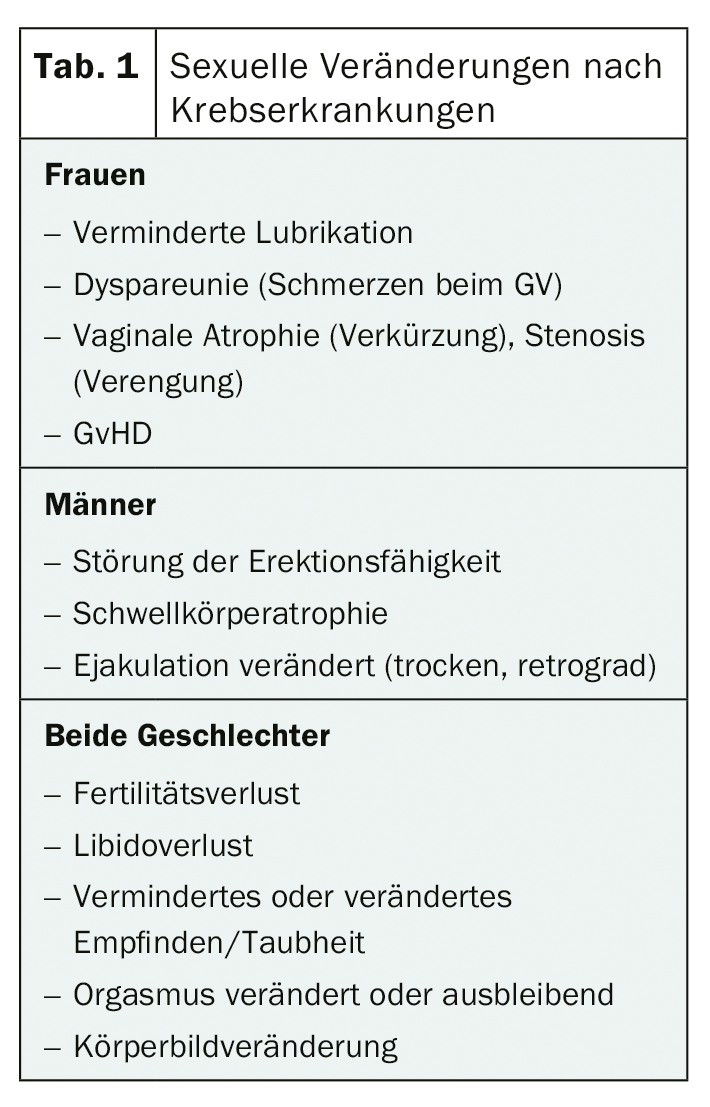
Data on the effects of disease or treatment on sexual function now exist for numerous patient groups [1,2]. The incidence of sexual impairment ranges from 20% to nearly 100%, depending on the patient population, disease diagnosis, and type of treatment. In Table 1 , an overview illustrates the most common somatic sexual problems.
In a survey by the Swiss Cancer League, 17% of patients and 16% of partners cited a need “for help to cope with changes in their sexuality” but felt largely unprovided for by their treatment providers [3]. Failure to provide care when needed may be associated with decreased quality of life [4,5], remorse regarding the treatment decision [6,7], increased psychological sequelae, and relationship problems [4,5].
Occasionally, increased sexual desire also occurs, e.g., against a background of disinhibition in CNS tumors, in the face of a shift in priorities or enactment of moral inhibitors related to carcinoma diagnosis. For a review of possible sexual outcomes after cancer, see Mamié, 2017 [8].
Psycho-social aspects
Sexual dysfunction usually does not result from a single, isolated cause, but is a complex bio-psycho-social interaction.
Body image, self-worth, identity: self-definition of one’s own attractiveness influences whether a person will show/provide him/herself sexually to a partner. Here, men are usually more sensitive to changes in their ability to function: if this is restricted, this leads to insecurity, self-esteem and identity crises and, as a consequence, not infrequently to withdrawal and depressive development. In women, corresponding processes become apparent when they see themselves as no longer attractive. Body image changes here can also lead to insecurity, self-esteem and identity crises.
Impact on partners: The stress levels of partners and especially of female partners of cancer patients are comparable to those of patients. They also have elevated anxiety and depression scores; both are associated with a decrease in libido.
Coping: in many cases, the redefinition of sexuality after cancer is associated with altered experience, altered functioning, feelings of grief, vulnerability, insecurity, and fear of failure. A common strategy for dealing with this is avoidance, but this contributes to the perpetuation of sexual symptomatology. In everyday clinical practice, therefore, sexual counseling/therapy often starts by making the consequences of the avoidant behavior visible to the person concerned and weighing up whether a confrontation with the change and the experience associated with it might be worthwhile in the service of a rediscovery of sexuality.
Sexual problems after cancer – somatic/functional solutions
The benefits of onco-sexological interventions on sexual function, relationship quality, and quality of life are undisputed [9]. There are a variety of ways to compensate for impaired sexual function on a somatic/functional level. Not infrequently, these fall short in that they are only partially effective or are not accepted by those affected. In medical/functional approaches, the psychosocial dimension should therefore be comprehensively taken care of at the same time [10].
Solution approaches psycho-social
Psychological and social factors also play a significant role in many sexual problems in oncology. Functional aids often do not fully compensate for a limitation. It therefore requires the willingness to face change for oneself and together with the partner. Acknowledging one’s own suffering from the situation and seeking professional support is the first step in successful coping. Softening strategies of avoidance, coming to terms with a changed body and reoccupying it with positive experiences can be accompanied as an important process on the path of rehabilitation by living through a wide variety of feelings such as grief, pain, shame, fear, insecurity or mortification. Qualified psychotherapeutic support, in which the feelings are acknowledged, supported by the therapist, dosed and repeatedly brought into connection with the resources, strengths and potential of the affected person, is therefore highly indicated. In couple settings, too, going through a wide variety of feelings is an important process for processing together. However, a rediscovery of sexuality after cancer is usually associated with adaptation. How should sexuality be re-lived and what tools fit in? An important force for progression is often curiosity; if this can be awakened, the avoidant, the evasive forces lose ground. For a description of the different sex therapy approaches with reference to their relevance in the oncology context, see Mamie, 2017 [11].
When and how can the topic be addressed?
There is a lack of evidence on the question of the right time – therefore the answer has to be asked individually from the patient. The American guidelines [4,12] recommend regular questioning about sexual function before, during, and after oncologic therapy and, if needed, adequate care for appropriate symptoms or referral to onco-sexologic and, if appropriate, gynecologic or urologic specialists.
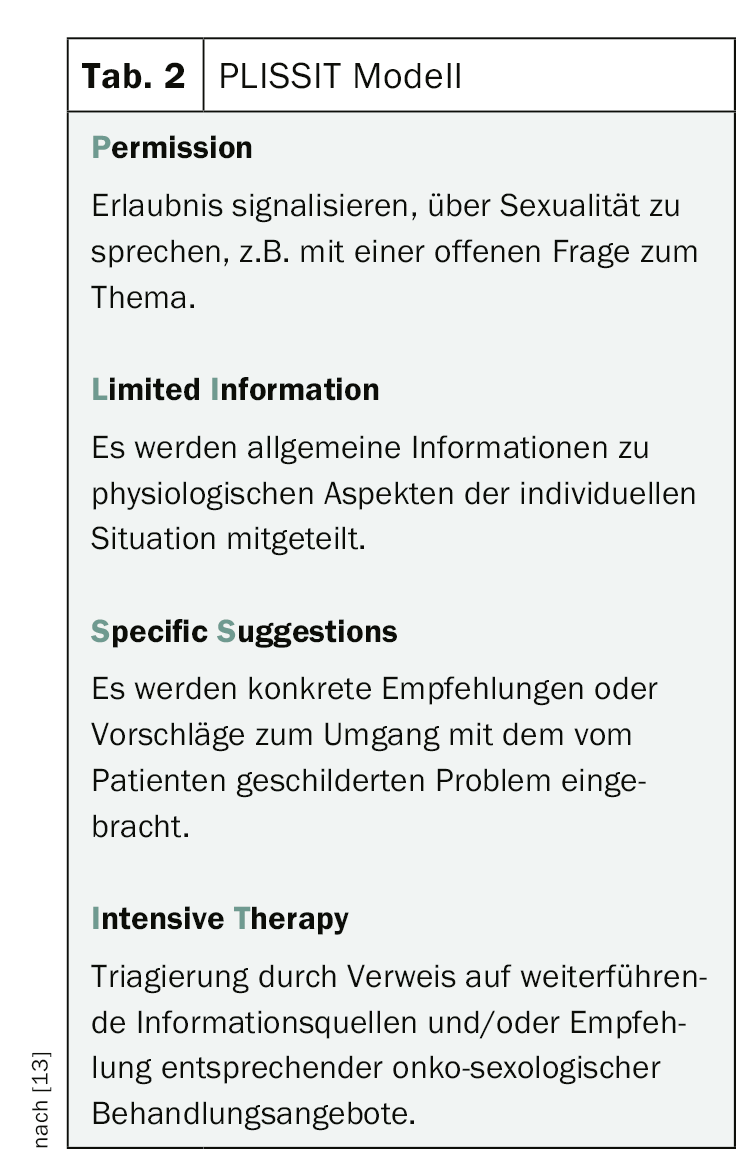
Removing a sexually relevant restriction is not important for every patient. The decisive factor for the need of support is therefore not the objective dysfunction, but the subjective suffering caused by the sexual disorder. To address the topic of sexuality, the PLISSIT model presented in Table 2 [13] can be used as a guide. Referral to an onco-sexology specialist may occur as early as the second stage, depending on the issue.
Overcoming communication barriers on the topic of sexuality
Difficulties in the area of sexuality are rarely addressed by the patients themselves. Every second to third patient is dependent on an active response by the physician [7]. Unchecked assumptions about age, gender, diagnosis, culture, or relationship status were the reasons for not responding by practitioners in an Australian study [14].
The personal recommendation of the oncologist is one of the most important predictors of the use of psycho-oncological support [15]. This also seems to be transferable to onco-sexological issues: In a French study [16], 51% of respondents expressed willingness to consult an onco-sexology specialist if recommended to do so by their healthcare provider.
Onco-Sexological Offers
Although specialists trained in sexual medicine/therapy are available throughout Switzerland, they are not always available nationwide. Travel should not be an insurmountable obstacle for patients, as an intervention will be limited to a few sessions in most cases. As the latest initiative, the Swiss Cancer League has been offering a separate mail consultation hour on the topic of sexuality after cancer as part of the cancer telephone since March 2019, thus offering those affected a low-threshold opportunity to access professionally qualified advice. The current versions of the brochures of the Swiss Cancer League (Male Sexuality 2016; Female Sexuality 2015) are recommended. They deal comprehensively and in a way that is understandable for those affected with the effects of different therapies on sexuality; psychological and relationship-dynamic aspects, however, are depicted in less depth.
Outlook
The involvement of psychooncological psychotherapists in oncology has become a matter of course. Sexuality care should also become a natural part of comprehensive oncology treatment. Integrated care of the future will offer professionals trained in sexual therapy as part of a psycho-oncological-psychotherapeutic service within oncology or as part of a care network with low-threshold opportunities for interdisciplinary information exchange. At the same time, interdisciplinary care can be provided by the sex therapist to other clinics prominently associated with sexuality, such as gynecology and urology.
Literature:
- Bober S, Sanchez Varela V: Sexuality in Adult Cancer Survivors: Challenges and Intervention. Journal of Clinical Oncology 2012; 30: 3712-3719.
- Ntekim A. (2011). Sexual Dysfunction Among Cancer Survivors. In: Goshtasebi A. (Ed.) Sexual Dysfunctions – Special Issues. Download at: www.intechopen.com/books/sexual-dysfunctions-special-issues/sexual-dysfunction-among-cancer-survivors
- Navarra S, Eichenberger C, Fluri M, et al: Psychosocial oncology in Switzerland. Krebsliga Schweiz, 2005.
- NCCN Guidelines Survivorship: Sexual Dysfunction (Male). J Nat Compr Canc Netw 2014; 12: 356-363.
- Penson D: The Effect of Erectile Dysfunction on Quality of Life Following Treatment for Localized Prostate Cancer. Rev Urol 2001; 3: 113-119.
- Guilts C, Cohen L, Pettaway C, Parker P: Treatment Regret and Quality of Life Following Radical Prostatectomy. Support Care Cancer 2013; 12: 21.
- Buddeberg C, Bitton A, Eijsten A, Casella R: Management of a taboo. Expect study: erectile dysfunction therapy from the perspective of physicians and patients. ARS Medici 2007; 14: 689-693.
- Mamié S: Onco-sexology. Switzerland. Cancer Bulletin 2017; 02: 160-162.
- Brotto LA, Yule M, Breckon E: Psychological interventions for the sexual sequelae of cancer: a review of the literature. J Cancer Surviv 2010; 4: 346-360.
- Schover LR, Canada AL, Yuan Y, et al: A randomized trial of internet-based versus traditional sexual counseling for couples after localized prostate cancer treatment. Cancer 2012; 118: 500-509.
- Mamié S: Onco-sexology 2; treatment options for sexual sequelae after cancer. Switzerland. Cancer Bulletin 2017; 03: 256-259.
- NCCN Guidelines Survivorship: Sexual Dysfunction (Female). J Nat Compr Canc Netw 2014; 12: 184-192.
- Annon JS: PLISSIT model. In: Corsini RJ (ed.). Handbook of Psychotherapy. Weinheim: Beltz, 1983.
- Hordern A, Street A: Communicating about patient sexuality and intimacy after cancer: mismatched expectations and unmet needs. Med J Aust. 2007; 186: 224-227.
- Zwahlen D: Of the gap between psychosocial distress and support utilization: results of a psycho-oncology stress screening study. Switzerland. Cancer Bulletin 2019; 02: 167-169.
- Almont T, Delannes M, Ducassou A, et al: Sexual Quality of Life and Needs for S-xology Care of Cancer Patients Admitted for Radiotherapy: A 3-Month Cross-Sectional Study in a Regional Comprehensive Reference Cancer Center. Journal of Sexual Medicine 2017; 14: 566-576.
InFo ONCOLOGY & HEMATOLOGY 2019; 7(4): 20-21.











