73-year-old patient presents with intermittent acid regurgitation and worsening symptoms with additional atypical complaints that respond inadequately to medical treatment.
Background: A 73-year-old patient had been suffering from typical GERD symptoms, mainly intermittent acid regurgitation, for about 20 years. However, the complaints showed an increasingly atypical expression and for several months a volume reflux was present during anterior bending. Initially, PPI therapy was tried, followed by treatment with 120mg/d Dexilant® and 3x/d Gaviscon®, which, however, did not improve the symptoms sufficiently. An attempt to discontinue PPI therapy was unsuccessful.
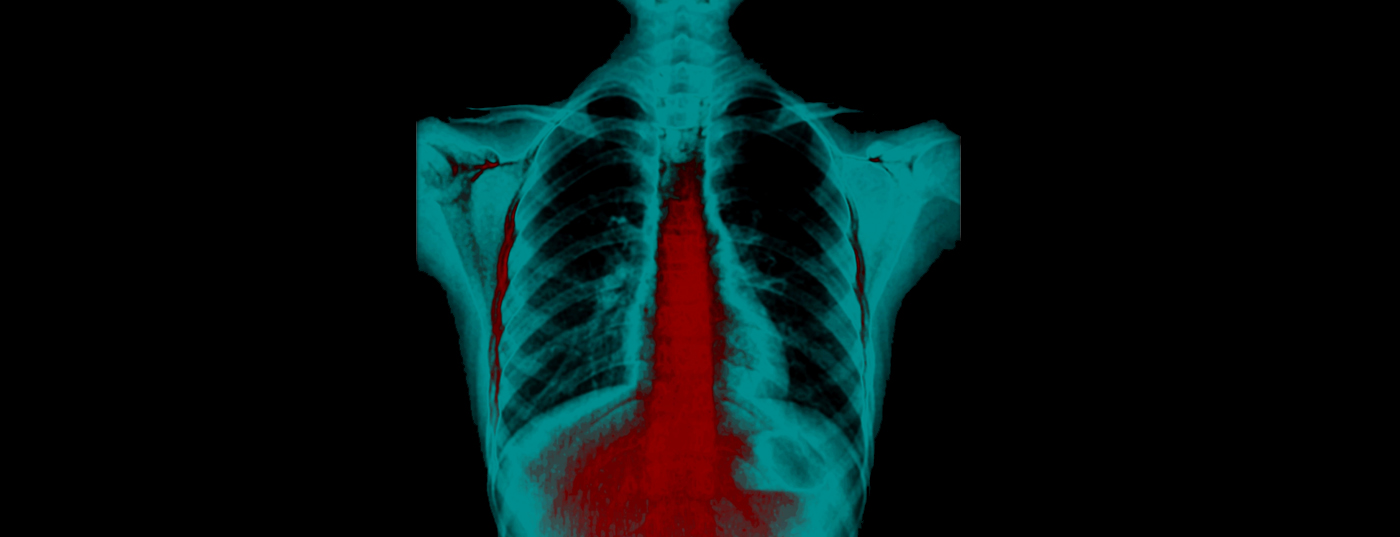
History and diagnosis: The patient presented after a renewed progression of the existing symptoms. He stated that he was experiencing increasing dysphagia with solid foods, in addition to epigastric and retrosternal pain. Further history also revealed arterial hypertension. Endoscopy and thoracoabdominal CT were performed to establish the diagnosis. A large hiatal hernia was identified.


Therapy: The patient then underwent transhiatal mobilization, posterior crurorrhaphy and Nissen fundoplication during surgery. As a result, the patient is currently symptom-free and only when alcohol is consumed is the intermittent intake of alginate.
 Comment by Yves Borbély, MD: The present case shows that in case of volume reflux, dysphagia and non-response to combination treatment with proton pump inhibitor and alginate, further clarification should be performed. If symptoms worsen after a frustrated discontinuation attempt, surgical treatment may be indicated.
Comment by Yves Borbély, MD: The present case shows that in case of volume reflux, dysphagia and non-response to combination treatment with proton pump inhibitor and alginate, further clarification should be performed. If symptoms worsen after a frustrated discontinuation attempt, surgical treatment may be indicated.