Stable angina is characterized by reversible ischemia or hypoxia of the myocardium. At rest, sufficient blood flow is ensured in patients with stable angina pectoris. However, during physical exertion or emotional stress, blood flow cannot be adequately increased and patients become symptomatic. Typically, the symptoms manifest as a feeling of pressure or discomfort in the chest area, possibly with radiation to the neck, lower jaw, and left arm, and they are reproducible. The following article provides an overview of the treatment.
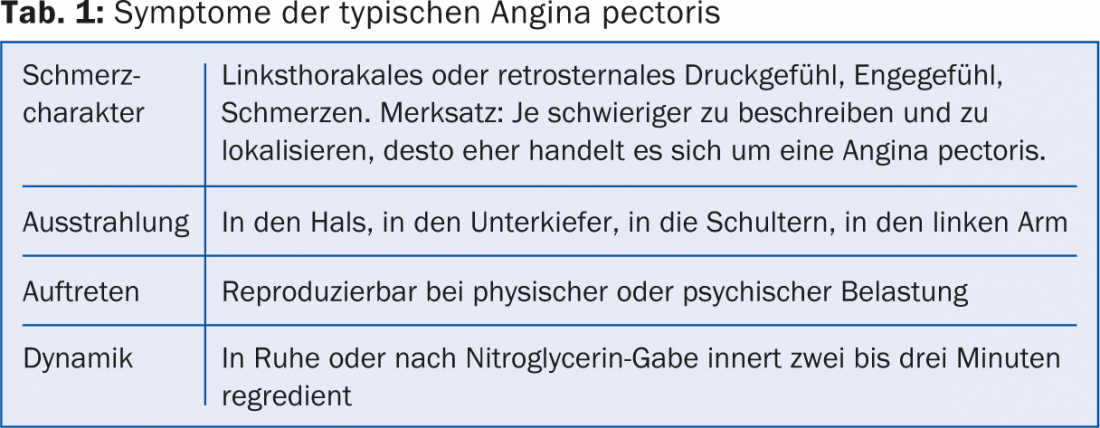
At rest, the typical angina pectoris symptoms should be completely regressed within two to three minutes. Typically, they also respond to nitroglycerin within a few minutes (tab. 1). Often forgotten is the question of whether the patient’s symptoms occur together with palpitations. In fact, arrhythmias can often cause symptoms similar to angina.
Pathophysiologically, stable angina usually underlies stenosis of the coronary vessels. However, some patients experience typical angina despite normal coronaries. Microvascular dysfunction may be present here. Increased intracardiac pressure (both left ventricular and right ventricular) may also cause angina symptoms. Vasospasm can also cause similar symptoms, but these occur more often at rest, usually in the early morning hours, and do not manifest as classic angina. In some patients, a combination of these mechanisms is present.
The incidence of stable angina is estimated to be 1% in the male population aged 45-65 years, and higher in women due to a higher prevalence of vasospasm [1]. With increasing age (from 75 years of age), an incidence of approximately 4% can be assumed in both sexes [1].
Prognosis of stable angina pectoris
Stable angina – in contrast to unstable angina – is a relatively benign condition. With adequate drug therapy, the annual incidence for myocardial infarction is only about 3, and mortality is about 2% [2,3]. The incidence is somewhat higher in high-risk patients (for example, diabetics or patients with manifest PAVK). Assessing the patient based on their risk profile is important as this may influence therapy in some circumstances. In addition to traditional cardiovascular risk factors such as arterial hypertension, nicotine use, diabetes, hypercholesterolemia, family history, and lack of physical activity in daily life, at best, the patient’s increased heart rate also worsens prognosis. The additional presence of heart failure significantly worsens the prognosis.
Clarification of patients with stable angina pectoris
The Canadian Caridovascular Society classification has become internationally established for assessing the severity of angina pectoris (Table 2).

Clinical examination is often poor in patients with angina. On the ECG, look for signs of a past myocardial infarction (for example, Q-spikes) as well as repolarization abnormalities (changes in the T-wave) that may occur due to myocardial ischemia. A chest x-ray can be performed as a supplement. This is recommended for patients with possible lung disease or suspected heart failure.
Further examinations, such as transthoracic echocardiography or a 24-hour Holter ECG examination in case of palpitations, are performed in collaboration with a cardiologist. The pre-test probability can be determined by means of a graph. Any further clarifications are based on this pre-test probability. This is determined by means of table 3.
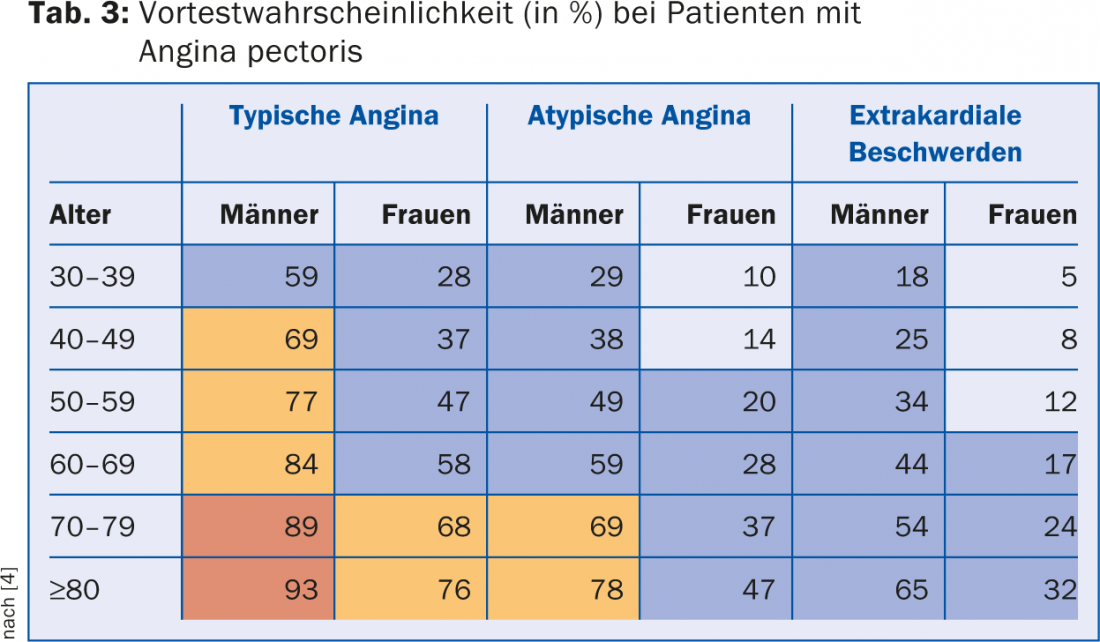
Depending on the pre-test probability, the following further steps are recommended:
- Patients with a low pre-test probability (<15%, light blue): As a rule, no further clarification is necessary here. Rather, alternative diagnoses should be considered (e.g., gastroesophageal reflux, musculoskeletal complaints). At most, a computed tomography scan may be ordered to exclude coronary stenosis.
- With intermediate pretest probability (15-65%, blue), ergometry is recommended in most patients. If a definitive diagnosis cannot be made even after this, another noninvasive test should be performed (e.g., stress echocardiography, scintigraphy, MRI). Computer tomography is also possible here. However, it is only recommended for patients who are not expected to have severe vascular calcification.
- If the pretest probability is higher (66-85%, orange), the patient may be scheduled directly for coronary angiography, or a noninvasive test may be performed. However, ergometry does not make sense here because of the low sensitivity, as too many false-negative findings would result.
- In patients with a very high pretest probability ( >85%, red), coronary angiography is recommended directly for definitive clarification.
Therapy of stable angina pectoris
The other article deals with the management of patients with stable angina pectoris in whom the diagnosis of coronary artery disease has been confirmed.
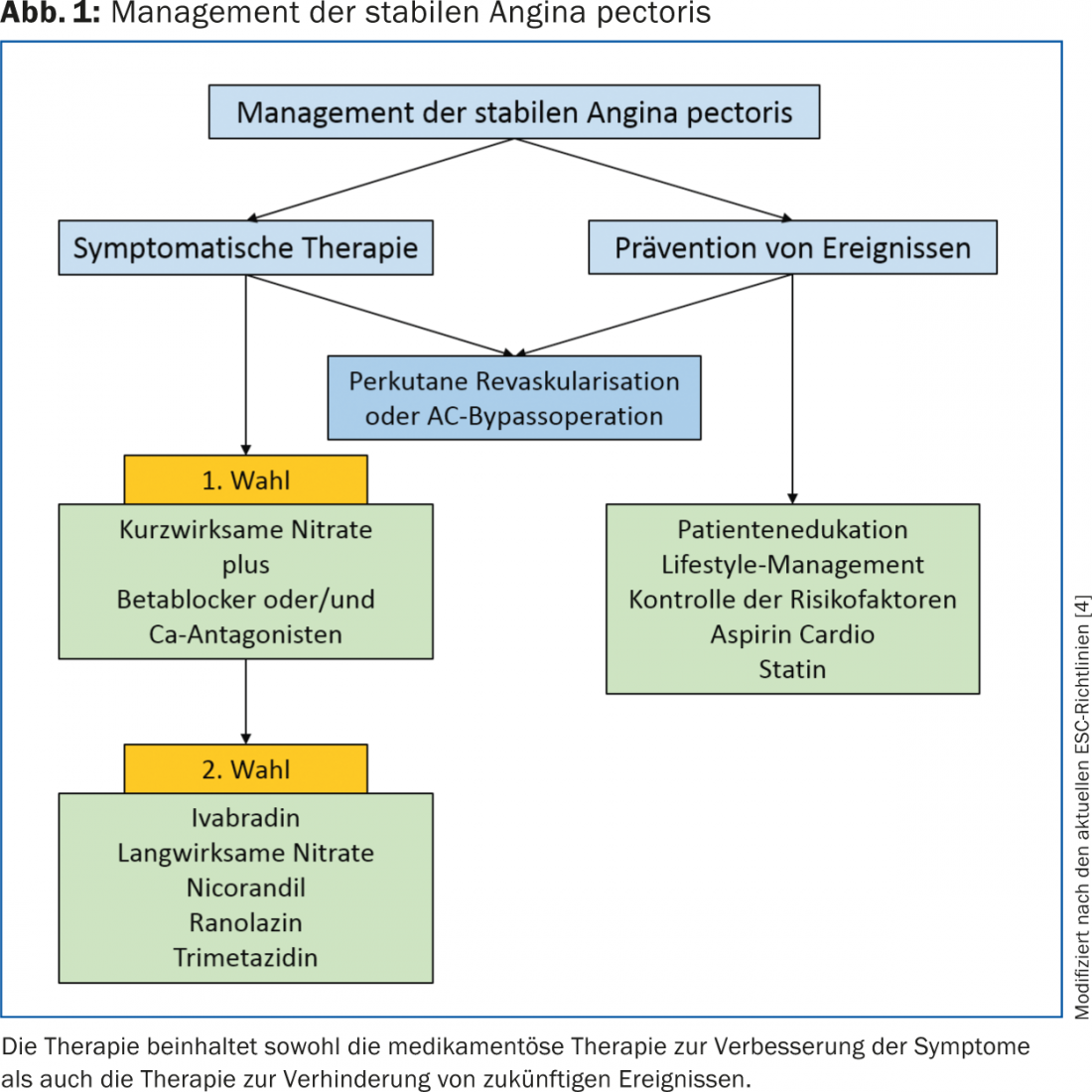
The aim of treatment is both symptomatic therapy of the symptoms and improvement of the prognosis. Therapy includes both lifestyle modification and drug therapy of risk factors (Fig. 1) [4].
A must: nicotine stop
Primarily, patients who use nicotine should be supported to stop smoking. The benefits of smoking cessation have been extensively studied; along with regular physical activity, it is the secondary preventive measure with the greatest prognostic benefit. Smoking cessation after myocardial infarction reduces mortality by 30-40% [5]. In patients after myocardial infarction, motivation to stop nicotine is usually sufficiently high. It is more difficult with patients who have never had an infarction, here only about 5-10% are abstinent after one year. Supportive behavioral therapy, nicotine replacement medications, or other medications to reduce physical dependence can increase the success rate. Nicotine replacement products can be safely administered to patients with coronary artery disease. Bupropion (Zyban®), a selective dopamine and norepinephrine reuptake inhibitor, may also be used. With varenicline (Champix®), there is evidence of a slight increase in cardiovascular mortality.
Physical training
Regular physical activity has a positive effect in several ways. Blood pressure is lowered, the lipid profile improves, and the onset of type 2 diabetes mellitus can also be delayed or prevented. Physical exercise also improves the function of the vascular wall, the endothelium. This can reduce cardiovascular events. The prognosis is improving. Generally, three times a week 30 min. aerobic training recommended.
How important is nutrition?
Complementary to smoking cessation counseling, a change in diet should be discussed with the patient. Here, attention should be paid primarily to a reduction in caloric intake, and a target weight with a body mass index of <25 kg/m2 should be aimed for [4]. It is also recommended to take polyunsaturated fatty acids (PUVA), as found in the Mediterranean diet. Two to three fruits and two to three servings of vegetables should be taken daily. Although the Mediterranean diet significantly reduces cholesterol intake, no additional benefit on cholesterol levels has been demonstrated. In some studies, moderate alcohol intake was associated with better survival. Alcohol also affects cholesterol – it has an antithrombotic effect and increases HDL cholesterol. Red wine also contains flavonoids, which have an antioxidant effect. The recommended daily dose for men is <30 g, for women <20 g, which corresponds to about one to two glasses of wine daily. Overall, the current evidence suggests that dietary modification may have a positive impact on prognosis. However, the extent to which the risk can be reduced is controversial.
Therapy of hypercholesterolemia
According to the current recommendations of the European Society of Cardiology (ESC), a target LDL of <1.8 mmol/l should be achieved in patients with known coronary artery disease. Statins are the drugs of first choice. However, this target value often cannot be achieved with a statin alone. In such cases, ezetimibe (Ezetrol®) is additionally recommended, although no prognostic benefit has yet been demonstrated for ezetimibe alone. A corresponding study is currently being conducted (Improve It study). The results are expected to be available by the end of this year. Currently, a new class of drugs is also being tested, so-called PCSK9 inhibitors. These are monoclonal antibodies against a factor that inhibits the formation of LDL receptors on the liver. Corresponding Phase II and III studies are currently being conducted. The following three questions often come up in connection with cholesterol reduction:
- How low can an LDL value be? There are people and peoples who naturally have very low LDL levels around 1.5 mmol/l. A reduction up to 1.5 mmol/l therefore appears unproblematic.
- What about patients over the age of 80? For primary prevention, a statin should certainly not be prescribed at this age. However, in the case of pronounced CHD and otherwise still good general condition, a statin seems quite justifiable. Statin is not recommended in >85-year-old patients.
- What about patients who have very early myocardial infarction? Remember: familial hypercholesterolemia is relatively common in Switzerland, with an estimated prevalence of 1/200. Therefore, family members of patients who have suffered very early myocardial infarction should be tested for hypercholesterolemia and treated if necessary [6].
Therapy of arterial hypertension
If arterial hypertension is present, it must be treated with the goal of achieving a blood pressure of <140 mmHg systolic and <90 mmHg diastolic. In diabetics, a diastolic blood pressure of <85 mmHg is recommended [4].
Pharmacological treatment of angina
Antianginosa either improve oxygen delivery to the heart or decrease the oxygen demand of the heart ( Table 4).
Nitrates: For acute symptom relief, nitrates are useful for prompt control of the patient’s symptoms. Short-acting nitrates are mostly used for short-term symptomatic therapy. The effect of nitrates is based on vasodilation of the vessels with reduction of both preload and afterload. When using long-acting nitrates, make sure that a nitrate-free interval is repeatedly observed, otherwise rapid habituation will occur. Common side effects of nitrates include hypotension and headache. The former occur to a pronounced extent in the case of simultaneous use of a PDE5 inhibitor (for example, sildenafil), which is why simultaneous use is contraindicated.
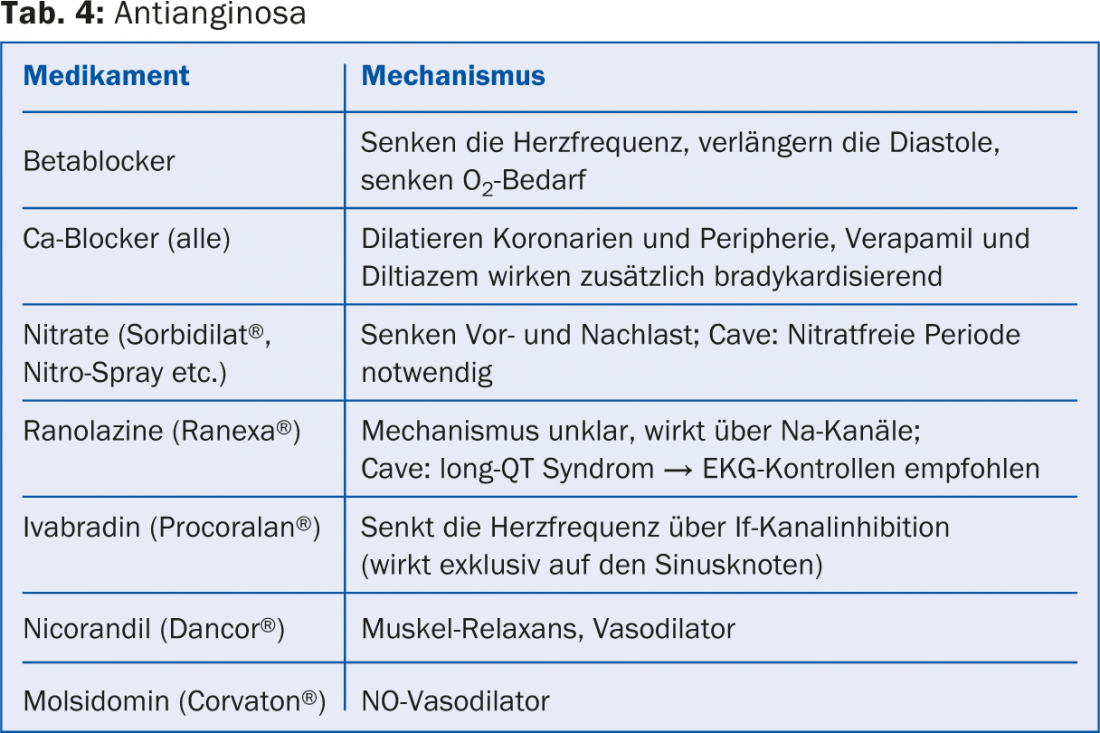
Beta-blockers: beta-blockers decrease heart rate (negative inotropy) and reduce myocardial contractility. In addition, they improve myocardial perfusion by increasing vascular resistance in non-ischemic areas and prolong diastole. In patients with St.n. Myocardial infarction and impaired systolic function, beta-blockers also reduce mortality [7]. During therapy with beta-blockers, it should be noted that concomitant therapy with verapamil or diltiazem is (relatively) contraindicated, as this may result in symptomatic bradycardia and risk of higher-grade AV block. In addition, beta-blockers are contraindicated in vasospastic angina.
Calcium channel blockers: Further therapy of angina pectoris includes the use of calcium channel blockers. Here, the mechanism of action is achieved by vasodilation and lowering of peripheral resistance. This also makes them suitable for the treatment of vasospasms. In the use of calcium channel blockers, it is important to distinguish between two subgroups of this class of drugs: dihydropyridine-type calcium channel blockers and nondihydropyridines. These two subgroups occupy different sites on calcium channels. Their distinction in clinical use is important because the group of non-dihydropyridines (verapamil, diltiazem) additionally achieves a negative chronotropic effect. With both substances, concomitant therapy with a beta-blocker should be avoided – as already mentioned above.
Ivabradine (Procoralan®): The effect of ivabradine is achieved by selective inhibition of the sinus node, resulting in lower heart rate and reduced myocardial oxygen consumption. The inotropy of the myocardium remains unchanged. Ivabradine may be used alone or in combination with a beta-blocker in patients with sinus rhythm and a resting rate of ≥60/min. be administered. Current guidelines recommend an initial dose of 2× 5 mg daily, then increasing to 2× 7.5 mg daily over the course. The exact dosing and indication is still being evaluated at the moment, as a preliminary analysis of the SIGNIFY study showed a slightly increased risk of the combined endpoint of cardiovascular death and myocardial infarction in the ivabradine group. However, in this study, the drug was used at a dose up to 2×10 mg daily. is applied [8].
Nicorandil (Dancor®): Nicorandil acts as a nitrate derivative and potassium channel opener. It may be given in addition to beta-blocker and/or calcium channel blocker therapy. The desired effect is achieved by vasodilation of the coronary vessels.
Ranolazine (Ranexa®): Ranolazine inhibits late sodium influx into cells. It reduces the patient’s angina and increases performance. The drug is approved as an adjunct to therapy with beta-blockers and calcium antagonists. The antianginal effect is best in diabetic patients [9].
Platelet aggregation inhibitors: platelet inhibitors inhibit coronary thrombus formation and may prevent infarcts [10]. The risk of bleeding is slightly increased with this therapy. In principle, all patients with known coronary artery disease should be treated with 100 mg of aspirin daily. The exception, of course, is patients who have recently been stented; these usually require dual platelet inhibition for one year. Stable patients (more than one year after the last infarction or after the last stent implantation) with indication for oral anticoagulation need only this and should not be treated additionally with antiplatelet agents.
Coronary angiography and revascularization: In stable angina, there are two primary indications for coronary angiography and possible revascularization therapy: angina that limits the patient’s daily life and angina in high-risk patients [4]. Coronary angiographies are nowadays safe procedures with a risk of a relevant complication of <0.5% and are often performed on an outpatient basis. Nowadays, if a high-grade stenosis is seen, it is usually treated with a drug-eluting stent and the patient should be symptom-free thereafter. If narrowing is present in multiple vessels, the patient may be treated with multiple stents or even an aortocoronary bypass, depending on the anatomy.
CONCLUSION FOR PRACTICE
- Therapy for stable angina includes lifestyle changes as well as drug therapy and revascularization therapy.
- Many patients require several medications at the same time, the effects of which they themselves do not immediately notice (e.g., cholesterol reduction, blood pressure reduction, etc.). Therefore, it is important that the effects of these drugs are explained to patients to improve compliance. Overall, however, the three most important measures in patients with coronary artery disease are:
1. revascularization
2. nicotine stop
3. regular physical exercise
4. regular use of medication - These measures can significantly improve both the prognosis and the quality of life of these patients.
Literature:
- Hemingway H, et al: Incidence and prognostic implications of stable angina pectoris among women and men. JAMA 2006; 295: 1404-1411.
- Boden WE, et al: Optimal medical therapy with or without PCI for stable coronary disease.NEng JMed 2007; 356: 1503-1516.
- Daly CA, et al: Predicting prognosis in stable angina: results from the Euro heart survey of stable angina: prospective observational study. BMJ 2006; 332:262-267.
- 2013 ESC guidelines on the management of stable coronary artery disease. European Heart Journal 2013; 34, 2949-3003.
- Critchley J, Capewell S: Smoking cessation for the secondary prevention of coronary heart disease. Cochrane Database Syst Rev 2004; 1: CD003041.
- Nordestgaard BG, et al: Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: guidance for clinicians to prevent coronary heart disease: Consensus Statement of the European Atherosclerosis Society. Eur Heart J 2013; 34: 3478-3490.
- Yusuf S, Wittes J, Friedman L: Overview of results of randomized clinical trials in heart disease. I. Treatments following myocardial infarction. JAMA 1988; 260:2088-2093.
- Fox K, et al: Rationale, design, and baseline characteristics of the Study assessInG the morbidity-mortality beNefits of the If inhibitor ivabradine in patients with coronary artery disease (SIGNIFY trial): a randomized, double-blind, placebo-controlled trial of ivabradine in patientswith stable coronary artery disease without clinical heart failure. Am Heart J. 2013; 166(4): 654-661.
- Kosiborod M, et al: Evaluation of Ranolazine in Patients with Type 2 Diabetes Mellitus and Chronic Stable Angina. Results from the TERISA randomized clinical trial.J Am Coll Cardiol 2013; 61(20): 2038-2045.
- Antiplatelet Trialists’ Collaboration: Collaborative overview of randomised trials of antiplatelet therapy: I: Prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. BMJ 1994; 308: 81-106.
HAUSARZT PRAXIS 2014; 9(9): 18-23