The European Society of Cardiology (ESC) recently updated its guidelines. Consequently, based on the EMPEROR-Preserved and DELIVER trials, the use of SGLT-2 inhibitors is now recommended for all stages of heart failure. Thus, in addition to HFrEF, HFmrEF and HFpEF are now class IA indications for dapagliflozin or empagliflozin. In clinical trials, the use of SGLT-2 inhibitors has significantly reduced hospitalizations due to heart failure in particular.
Heart failure is a clinical syndrome regardless of etiology – structural or functional damage to the heart sooner or later leads to heart failure. Since the European Society of Cardiology (ESC) guidelines on heart failure were published two years ago, there has been a great deal of progress with regard to drug treatment options. Some things done. In the 2021 ESC guideline, a recommendation for the use of SGLT-2 (sodium-glucose cotransporter 2) inhibitors was available only for heart failure with reduced left ventricular ejection fraction (HFrEF) [1]. Meanwhile, results of randomized-controlled trials of the efficacy and safety of dapagliflozin and empagliflozin have led to the recommendation of these SGLT-2-i in heart failure with intermediate and preserved ejection fraction (HFmrEF and HFpEF, respectively) [2]. In summary, SGLT-2 inhibitors should be considered for all heart failure patients, summarized Prof. Andreas Flammer, MD, Senior Physician, Department of Cardiology, University Hospital Zurich [5]. This update is mainly based on data from the EMPEROR-Preserved and DELIVER trials, in which the combined primary end point was met in heart failure patients with LVEF >40% [3,4].
| Abbreviations HF = heart failure HFrEF = “Heart failure with reduced ejection fraction”. HFmrEF = “HF with mildly reduced EF” (HF with medium ejection fraction) HFpEF = “HF with preserved EF” (HF with preserved ejection fraction) NYHA = New York Heart Association LVEF = Left Ventricular Ejection Fraction NT-proBNP = N-terminal natriuretic peptide type B eGFR = estimated glomerular filtration rate |
Dapagliflozin or empagliflozin in the context of the “Fantastic Four”.
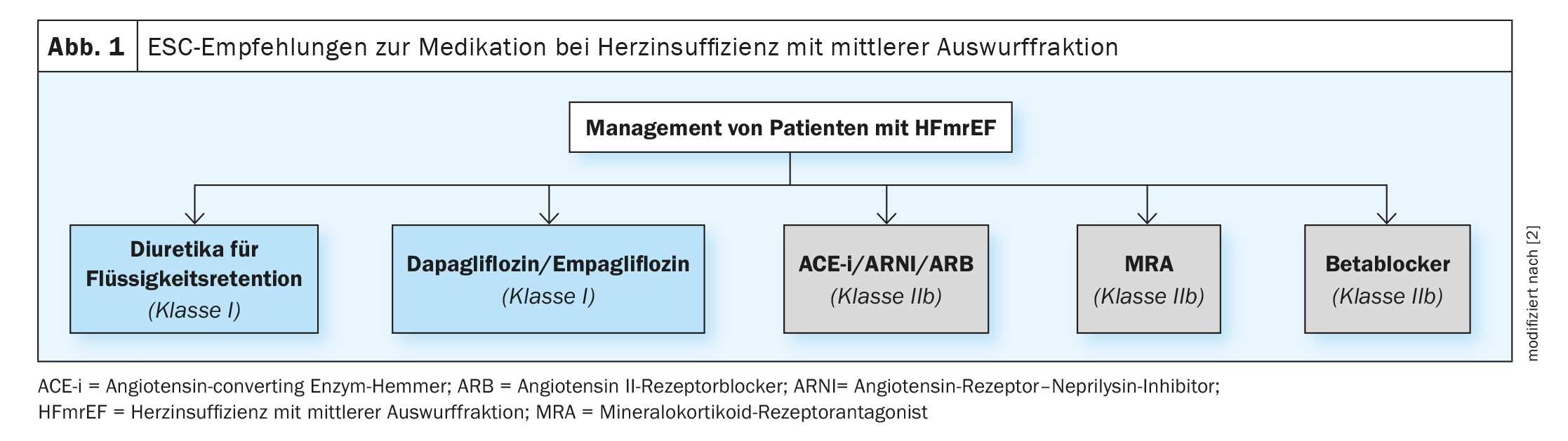
Treatment of patients with HFmrF (LVEF 41-49%) is broadly similar to HFrEF. For both HFrEF and HFmrEF, the gold standard is that one representative of each of the following combination of four is used simultaneously or in close succession [1,2]:
RAS blockers (ACE inhibitors, ARNI, ARB), mineralocorticoid receptor antagonist (MRA), beta blockers, and an SGLT-2 inhibitor (dapagliflozin or empagliflozin) (Fig. 1) . In patients with signs and symptoms of congestion, the use of diuretics is still recommended.
For an eGFR >40 ml/min, start with a four-drug combination; for an eGFR 30-40 ml/min, start with a three-drug combination (beta-blocker, ARNI, SGLT-2-i); for an eGFR 15-30 ml/min, be a little more careful, he said. Every heart failure therapy is initially accompanied by a decrease in eGFR and an increase in creatinine. However, one should not be deterred by this. A lower eGFR is prognostically unfavorable, but even patients in whom eGFR falls below 25 ml/min during therapy have a benefit from SGLT-2-i. “This is an important message,” said Prof. Flammer [5]. This finding stems in part from the DAPA-CKD trial, in which patients with an eGFR of 25-75 ml/min were treated with dapagliflozin 10 mg/d or placebo, with 11% of the 4304 study participants having heart failure. In addition to the renal composite endpoint, which was reduced by 39% in the dapagliflozin arm, the risk of heart failure-related hospitalization or cardiovascular death was also reduced by 29% (hazard ratio [HR] 0.71; 95% confidence interval [KI]: 0.55-0.92; p=0.009) [6].
Results of the DELIVER and EMPEROR-Preserved studies.
The results of the DELIVER trial on the effects of dapagliflozin (10 mg once daily) compared with placebo in 6263 heart failure patients with LVEF >40% (NYHA class II-IV) were published last year [4]. Inclusion criteria included an elevated natriuretic peptide concentration (≥300 pg/ml in sinus rhythm or ≥600 pg/ml in atrial fibrillation) [4]. The analyses showed that dapagliflozin significantly reduced the primary endpoint of cardiovascular death or worsening heart failure (HF-related hospitalization or HF emergency consultation) (HR 0.82; 95% CI 0.73-0.92; p<0.001). Dapagliflozin, moreover, improved symptom burden. Heart failure patients without type 2 diabetes also showed the benefits observed with SGLT-2-i [4]. The efficacy of dapagliflozin was also consistent in those patients who remained symptomatic despite improved LVEF. This suggests that these patients also benefit from SGLT-2 inhibitors [4,8].
The EMPEROR-Preserved trial included 5988 HF patients (NYHA class II-IV) with LVEF >40% and an elevated plasma concentration of NT-proBNP (>300 pg/ml in patients in sinus rhythm or >900 pg/ml in patients with atrial fibrillation) [3,9]. Participants were randomized to empagliflozin (10 mg once daily) or placebo. The primary end point was a composite of cardiovascular death or HF-related hospitalization. At a median follow-up of 26.2 months, empagliflozin significantly reduced the primary endpoint (HR 0.79; 95% CI 0.69-0.90; p<0.001). This effect occurred in patients with and without type 2 diabetes and was mainly due to a reduction in HF hospitalizations in the empagliflozin arm [8,9].
Congress: ZAIM Medidays
Literature:
- McDonagh TA, et al: 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. European Heart Journal 2021; 42(36): 3599-3726.
- McDonagh TA, et al: 2023 Focused update of the 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 2023; 44(37): 3627-3639.
- Anker SD, et al: Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med 2021; 385: 1451-1461.
- Solomon SD, et al.: Dapagliflozin in heart failure with mildly reduced or preserved ejection fraction. N Engl J Med 2022; 387: 1089–1098.
- “Heart failure: focus on heart, kidneys and metabolism,” Prof. Andreas Flammer, MD, ZAIM Medidays, Sept. 01, 2023.
- Heerspink HJL, et al: Dapagliflozin in patients with chronic kidney disease. N Engl J Med 2020; 383: 1436-1446.
- Vaduganathan M, et al: SGLT-2 inhibitors in patients with heart failure: a comprehensive meta-analysis of five randomised controlled trials. Lancet 2022; 400: 757-767.
- Vardeny O, et al: Dapagliflozin in heart failure with improved ejection fraction: a prespecified analysis of the DELIVER trial. Nat Med 2022; 28: 2504-2511.
- Anker SD, et al: Baseline characteristics of patients with heart failure with preserved ejection fraction in the EMPEROR-Preserved trial. Eur J Heart Fail 2020; 22: 2383-2392.
HAUSARZT PRAXIS 2023; 18(10): 28-30 (published 10/28-23, ahead of print).