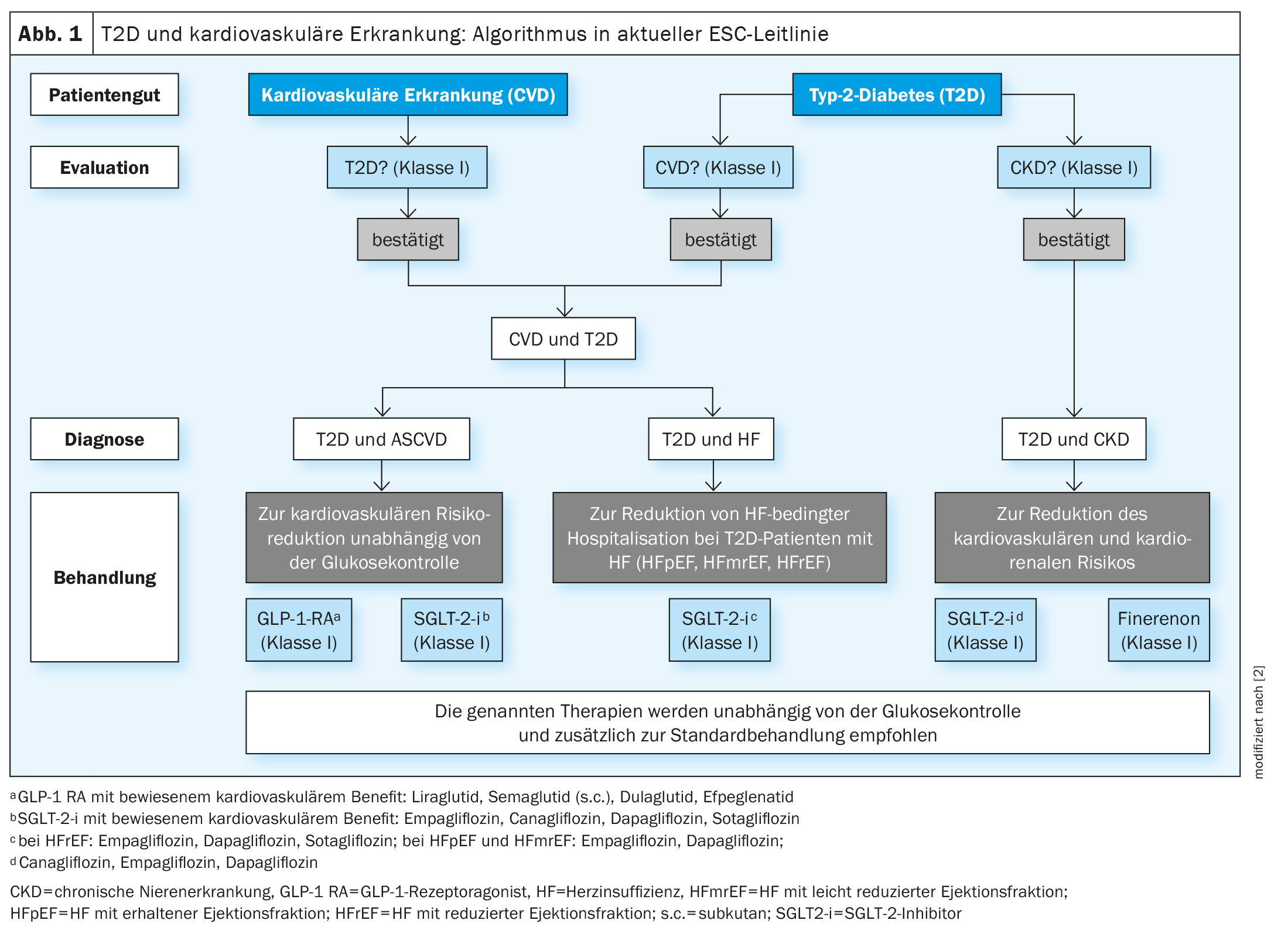
The current ESC guideline recommends blood glucose-lowering substances with a proven cardiovascular benefit for certain risk groups among type 2 diabetics. In type 2 diabetes (T2D) and atherosclerotic cardiovascular disease (ASCVD), the use of an SGLT-2-i and a GLP-1-RA is recommended, and in T2D patients with heart failure, an SGLT-2-i is recommended as an add-on. There is an evidence-based recommendation for SGLT-2-i and finerenone to reduce cardiorenal risk in T2D and chronic kidney disease (CKD).
Patient-centered, evidence-based recommendations for cardiovascular risk reduction are a focus of the ESC guideline published in 2023, reported the chairman of the guideline task force, Prof. Nikolaus Marx, MD, Director of the Department of Cardiology, Angiology and Internal Intensive Care Medicine, University Hospital Aachen [1]. The treatment recommendations are based on the cardiovascular benefit and/or cardiovascular safety of blood glucose-lowering drugs proven in clinical endpoint studies. The cardiovascular risk is classified as very high if manifest atherosclerotic cardiovascular disease (ASCVD**) or symptomatic chronic heart failure, chronic kidney disease (CKD) and/or severe target organ damage (TOD) are already present [2].
** ASCVD (atherosclerotic cardiovascular disease) includes coronary heart disease (CHD), peripheral arterial occlusive disease (PAD) and carotid stenosis.
Use risk-reducing substances at an early stage
Initially, screening and identification are crucial so that patients can then be given risk-reducing medication if necessary. Since many patients with cardiovascular disease (CVD) have undetected T2D and the risk of CVD is increased with T2D, it is advisable to screen CVD patients regularly for T2D (fasting glucose, HbA1c) or to evaluate T2D patients for the presence of CVD. The ESC guideline recommends primarily using active substances with proven cardiovascular benefit and switching or replacing substances without proven cardiovascular benefit. T2D patients with ASCVD need a GLP-1 receptor agonist (GLP-1-RA) and an SGLT-2 inhibitor (SGLT-2-i) in addition to other treatment; the guideline contains an evidence class IA recommendation for this. “We have learned that the early implementation of this risk-reducing medication is very important,” explained Prof. Marx [1]. This can reduce the cardiovascular risk independently of glucose control and in addition to standard therapy (e.g. platelet aggregation inhibition, antihypertensive therapy, lipid lowering). If the HbA1c target values are not achieved, the addition of metformin (class IIa) or pioglitazone (class IIb) can be considered.
SGLT-2-i is indicated for T2D patients with heart failure regardless of the ejection fraction (HFrEF, HFmrEF, HFpEF). “Among patients with type 2 diabetes, there are many with undetected heart failure,” said the speaker [1]. It is therefore recommended that diabetics are systematically examined for symptoms and signs of heart failure at every clinical contact. Based on data from large clinical trials, it is recommended that T2D patients with chronic heart failure, regardless of left ventricular ejection fraction, receive an SGLT-2-i to reduce heart failure-related hospitalization or cardiovascular death (Class IA). The use of SGLT-2-i and GLP-1-RA for risk reduction is independent of the HbA1c value. If the glucose-lowering effect proves to be insufficient, other substances can be added (class IIa recommendation), such as sitagliptin/linagliptin, metformin and insulin glargine/insulin degludec. The use of pioglitazone and saxagliptin is not recommended.
The ESC guideline also contains a special chapter on the management of cardio-renal risk in T2D patients with chronic kidney disease (CKD). For this patient group, the guideline recommends the use of SGLT-2 inhibitors and finerenone.
SCORE2: new 10-year risk score
For T2D patients without ASCVD or without severe end-organ damage, a new score was introduced in the ESC guideline to estimate the 10-year cardiovascular risk. The result of SCORE2-Diabetes – an extension of the SCORE2 algorithms by adding diabetes-specific parameters – predicts the 10-year risk of non-fatal myocardial infarction or stroke or death from any cardiovascular cause in type 2 diabetics over 40 years of age without previous cardiovascular disease [3,4]. Specifically, SCORE2-Diabetes integrates information on conventional cardiovascular risk factors (age, smoking status, systolic blood pressure, total and HDL cholesterol) with diabetes-related information (age at diabetes diagnosis, HbA1c and eGFR) to categorize patients as having low (<5%), moderate (5 to <10%), high (10 to <20%) or very high (≥20%) cardiovascular risk&. This 10-year risk classification can be helpful for taking preventive therapeutic measures that have not yet been implemented, such as lowering lipids or adding an SGLT-2-i and/or GLP-1-RA [2].
& without manifest cardiovascular disease
Congress: DGIM Annual Conference
Literature:
- “Cardiovascular optimized therapy of diabetes mellitus type 2”, Univ.-Prof. Dr. med. Nikolaus Marx, main session: What will change in practice with new guidelines? 130th Congress of the German Society of Internal Medicine (DGIM), 14.04.2024.
- Marx N, et al: ESC Scientific Document Group. 2023 ESC Guidelines for the management of cardiovascular disease in patients with diabetes. Eur Heart J 2023 Oct 14; 44(39): 4043-4140.
- SCORE2 working group and ESC Cardiovascular risk collaboration. SCORE2 risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe. Eur Heart J 2021; 42(25): 2439–2454.
- SCORE2-OP working group and ESC Cardiovascular risk collaboration. SCORE2-OP risk prediction algorithms: estimating incident cardiovascular event risk in older persons in four geographical risk regions. Eur Heart J 2021; 42(25): 2455-2467.
HAUSARZT PRAXIS 2024; 19(6): 28-30 (published on 26.6.24, ahead of print)