Forefoot surgery with large incisions, Kirschner wires and stiffeners is outdated. Toe deformities can be corrected very well by “minimally invasive surgery” (MIS). Weil osteotomies for metatarsalgias are also possible with MIS. A blessing compared to open technology.
Until about 15 years ago, foot surgery was an area of little interest and was overshadowed by the major disciplines of hip, knee, and shoulder surgery. Any surgeon could operate on feet. This has changed radically. Foot surgery has developed at a rapid pace into its own established specialty. No other specialization in the field of orthopedic surgery has experienced such significant technological progress in recent years as foot surgery. One of the greatest challenges for foot surgery is arthrofibrosis (stiffening of a joint due to adhesions), which occurs in about 20% of cases and causes unsatisfactory results in the same way as in the shoulder, elbow and hand. Patients suffer from chronic pain, stiffness and functional limitation despite technically correctly performed operations, which impairs the quality of life and ultimately leads to disability. To reduce the occurrence of such undesirable problems, the minimally invasive technique (“MIS”) was invented. This technique was developed by a group of surgeons from Barcelona and Bordeaux. The technique is touted to lead to better outcomes, faster healing and shortened rehabilitation due to less soft tissue damage and shortened surgical time. However, there are no scientific studies to date that directly compare conventional open techniques and MIS. The aim of this article is to present the current benefits of MIS for practitioners.
Weil osteotomies (shortening of the 2nd-4th metatarsal bones).
Weil osteotomies are typically performed for metatarsalgias after conservative therapies have failed. With open surgery, these are disfiguring operations, which is why many foot surgeons no longer perform them at all – this is where MIS is a real blessing (Fig. 1). Thanks to small stab incisions, there is significantly less scarring. However, scarring cannot be completely avoided, which can pull the toes into slight extension months after surgery. One disadvantage is that in certain cases, bone healing can take longer than the six weeks usually required for open surgery. Nevertheless, as with open surgery, patients can put aside the hard-soled sandal after six weeks and put on simple sneakers. The increased pressure on the osteotomies then stimulates bony consolidation.

Morton-Neurome
In splayfoot, the development of Morton’s neuromas is common due to overloading of the metatarsal heads. In open surgery, only the neuroma is resected, the nerve is permanently disrupted, and the cause of the excess pressure is left at the metatarsalia. The chance of success is about 80%. Here, too, MIS represents a better solution. As with carpal tunnel in the hand, percutaneous neurolysis is possible, which is successful in approximately 50% of cases. If this neurolysis is combined with MIS-Weil osteotomy, the chance of success is 80-90%. The nerve remains intact and the cause of Morton’s neuroma is eliminated.
Claw and hammer toes, medial and lateral deviation
To correct claw toes, hammer toes, and lateral deviations of the toes, open surgery requires resection or stiffening of toe joints, which is still usually done today with protruding Kirschner wires (with risk of infection and dislocation; Fig.2). These also stabilize healthy joints that are not affected by the disease, which means that they too end up damaged and stiff. In addition, this shortens the toes by about 5 mm, which affects the appearance of the foot. MIS is a real advantage in these cases as well. Stitches are used to release flexor and extensor tendons and the joint capsules, which can correct about 80% of toe deformities. The scars are barely visible (Fig. 2). If this procedure proves insufficient, a percutaneous osteotomy at the base of the proximal phalanx and/or the intermedial phalanx can be used to straighten the toe. Also, for laterally deviated toes, a lateral osteotomy can be used to fold the toe in the desired direction. The stab incisions, except when made dorsally, are in an invisible area and all joints are completely preserved.

Hallux valgus surgery
Hallux valgus surgery is probably the most common forefoot surgery and must be performed with high precision. It consists of three standard steps: osteotomy at metatarsal-1 (chevron or scarf), osteotomy at the proximal phalanx, and lateral release. Since open surgery has been very successful in these cases, the bar is set high for MIS. In the percutaneous technique, in which the bone is only cut via stitches with a burr, the osteotomy at metatarsal-1 is less precise. Therefore, some surgeons perform a “mini-open” technique, in which a 1-2 cm incision can be used to perform the osteotomy with the same precision as the open technique. Akin osteotomy and lateral release can be performed well percutaneously in any case. In my experience, MIS-Hallux surgeries result in smaller scars but have not shown any functional benefit. To get to the bottom of the question of potential functional benefits of MIS, a prospective multicenter study with blinded follow-up has been conducted at the FussZentrum Hirslanden Zurich since 2014, directly comparing MIS and open surgery and preventing positive bias. To date, there are only two comprehensive literature reviews [1,2] – one of which includes 26 studies and 2197 hallux surgeries – that compare the two techniques and conclude that no better results can be achieved with the MIS technique. So MIS is not a “miracle cure.”
Lapidus arthrodesis
Large hallux valgus deformities require a correction that is more proximal, as the correction then has more leverage. Depending on the length of the metatarsal-1, an open flaring osteotomy or an MIS “closing-wedge” osteotomy may be performed. Many patients have additional hyperlaxity and require stabilization of the Lisfranc-1 joint. Since this is usually still done with a distal correction of the same type as hallux valgus surgery, a long incision from the midfoot to the middle of the big toe is necessary. Because of the large soft tissue trauma and hematoma, a scar of this size predisposes to arthrofibrosis. Here, too, the MIS offers a better solution. An incision of 1-2 cm is used to resect the articular surfaces at the Lisfranc-1 joint. The results regarding correction and healing seem to be as good as with the open technique (Fig. 3).

There is also a purely percutaneous technique in which the joint surfaces are merely abraded via a stab incision and the “sawdust” is left in the joint. In my opinion, however, such a technique is not conducive to bone healing, as it leaves a mush of soft tissue and cartilage in the joint. The same applies to arthrodesis using the purely percutaneous technique at other sites of the midfoot as well as the hindfoot (e.g. at the lower ankle joint). While there are expert opinions (evidence level 5) describing that such surgeries are technically feasible, it remains an open question whether they are clinically successful for the patient in the long term. This must be observed particularly critically because the generally applicable rules of open surgery (e.g., clean preparation of joint surfaces, compression without interposition of soft tissues, anatomic reduction) are not observed in MIS of the midfoot and hindfoot. MIS is not a miracle cure, but must first prove its benefits scientifically.
Calcaneus osteotomies
Flat feet and hollow feet typically require the heel to be pushed back into its normal anatomical position, in addition to other surgical steps. Since the operation of such a deformity consists of many partial steps and many incisions, it is surgically advantageous if the calcaneus osteotomy can only be made via a stab incision, since this spares the soft tissues. Here, MIS offers a solution as it allows the calcaneus osteotomy to be performed through a stab incision only instead of a 4-6 cm incision. However, my own experience has shown that the achievable correction is usually only about 5-6 mm. In severe deformities, greater correction can be achieved with open surgery.
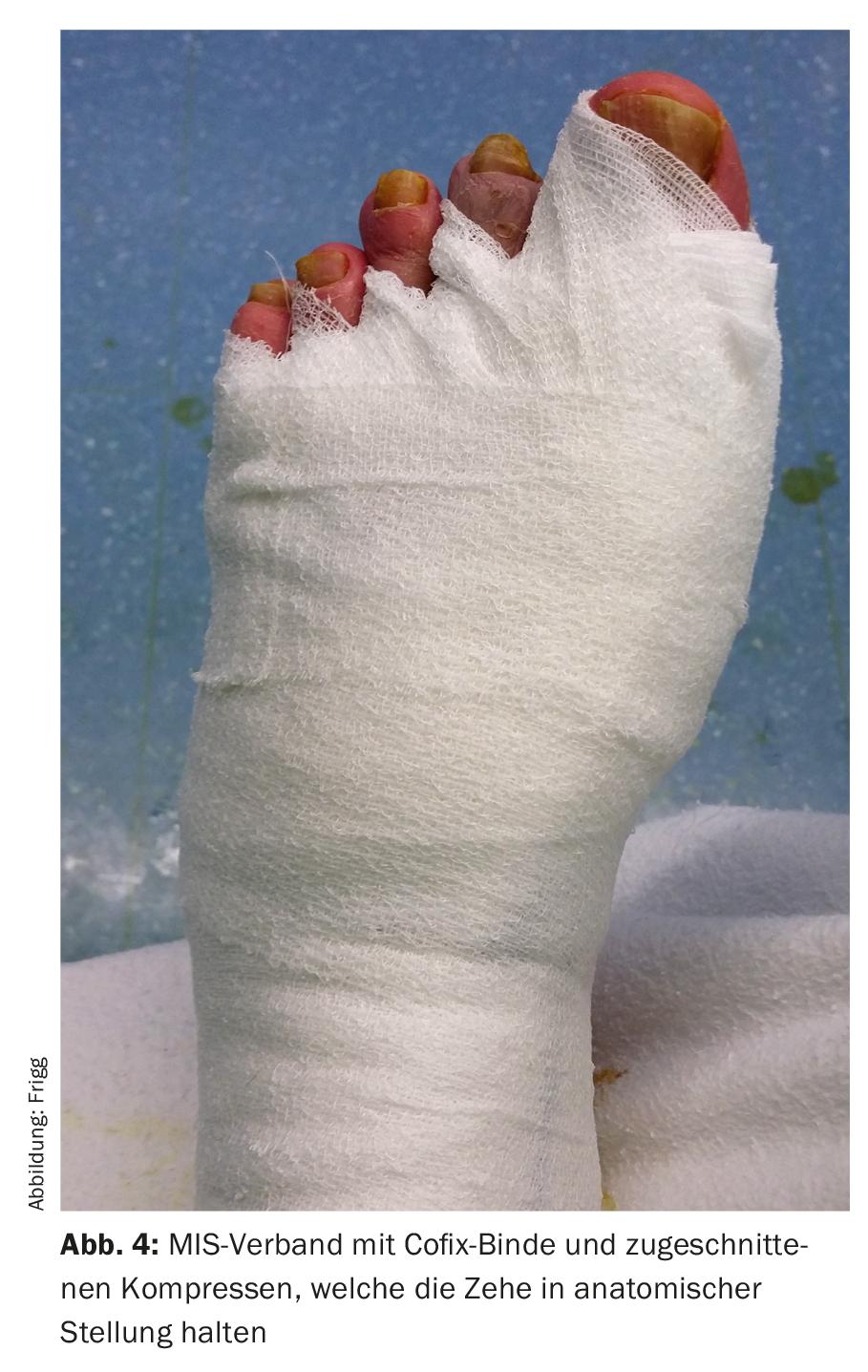
MIS Associations
While screw fixation is required for midfoot and hindfoot surgery with both conventional techniques and MIS, it is not required for forefoot surgery with MIS (except for chevron/scarf osteotomy). This means that the bones must be fixed externally with a stable bandage so that they can heal (Fig. 4). The application of these bandages determines the position in which the toes heal. The dressings must be changed approximately every week – in no case more frequently (as the osteotomies could shift with each change). We always change the dressings in practice. Proper application of dressings is a technique that must be learned, and improperly applied dressings can cause curvature of the toes.
Take-Home Messages
- Forefoot surgery with large incisions, Kirschner wires and stiffeners is outdated.
- Toe deformities can be corrected very well by “minimally invasive surgery” (MIS) with barely visible scars and better functionality.
- For metatarsalgias, Weil osteotomies can be successfully performed with MIS – a boon compared to the open technique.
- There is a 20% risk of arthrofibrosis with hallux surgery, for both open surgery and the MIS technique (so unfortunately, MIS does not work miracles).
- Changing MIS dressings should be done weekly by trained personnel, as improperly applied dressings will cause the toes to heal in the wrong position.
Literature:
- Maffulli N, et al: Hallux valgus: effectiveness and safety of minimally invasive surgery. A systematic review. British Medical Bulletin 2011; 97: 149-167.
- Trnka HJ, Krenn S, Schuh R: Minimally invasive hallux valgus surgery: a critical review of the evidence. International Orthopaedics (SICOT) 2013 Sept; 37(9): 1731-1735.
HAUSARZT PRAXIS 2017; 12(10): 24-27