Bronchiectasis, irreversible dilatation of the bronchi, accompanies many diseases but can also be congenital. If one wants to therapeutically address the entire clinical picture with all its symptoms (bronchiectasis), one is confronted with numerous studies investigating different therapeutic options. Matthias Salathé, MD, Miami, gave an overview at the annual meeting of the Swiss Society of Pneumology.
According to Matthias Salathé, MD, Miami, several diseases can cause bronchiectasis. First and foremost is cystic fibrosis (CF). Bronchiectasis in which CF has been excluded as a cause is referred to as non-CF bronchiectasis. Non-CF bronchiectasis affects approximately 4.2 individuals per 100,000 between the ages of 18 and 34 years. Among >75-year-olds, approximately 272 per 100,000 suffer from it. Diseases that may be associated with bronchiectasis include:
- Primary ciliary dyskinesia
- α-1-antitrypsin deficiency
- Post-infectious condition after tuberculosis/mycobacterial and childhood infections, allergic bronchopulmonary aspergillosis (ABPA).
- Immunological defects
- Rheumatoid arthritis
- Aspiration, gastroesophageal reflux disease (GERD)
- Chronic inflammatory bowel disease
- Congenital defects.
Independent factors associated with a more rapid decline in lung function in non-CF bronchiectasis were primarily chronic colonization with Pseudomonas aeruginosa (p=0.005), more frequent severe exacerbations (p=0.014), and systemic inflammation (p=0.023), according to a 2007 study [1].

How can the therapy be improved?
According to Salathé, several studies of non-CF bronchiectasis show a slight benefit from inhaled tobramycin because of colonization with Pseudomonas aeruginosa. While the drug helps partially against exacerbations, it also brings many side effects. Gentamicin also appears to be effective according to a recent study [2], but only with continuous, long-term use (compared with saline, it resulted in greater resilience, fewer exacerbations with longer time to first exacerbation, and, moreover, it did not trigger the development of resistance). Similar results could be found in a smaller phase II study [3] for inhaled liposomal ciprofloxacin.
A recent study [4] also concluded that inhaled colistin is a safe and effective treatment for patients with bronchiectasis and chronic colonization with Pseudomonas aeruginosa. The primary endpoint (significantly shorter time to exacerbation compared with placebo) was not met. However, when patient adherence was included as a factor (secondary endpoint), significant values could still be observed.
Macrolides (antibiotics) are also increasingly prescribed for stable bronchiectasis. However, a meta-analysis [5] on the long-term use of macrolides emphasizes the exacerbated problem of resistance and the occurrence of gastrointestinal events in this setting. The authors conclude that based on the overall positive results (e.g., reduced risk of exacerbations, lower average number of exacerbations per person), increased research activity for use in this patient group is well warranted.
Furthermore, 7% hypertonic saline can improve lung function and quality of life in patients with non-CF bronchiectasis [6].
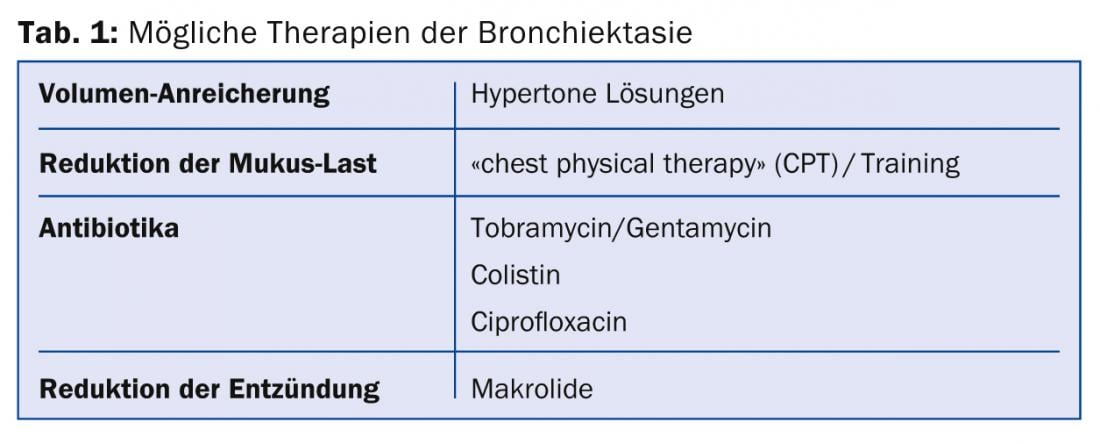
“One of the most important pillars of therapy, however, is physical training,” Salathé emphasized in conclusion. “The efficacy of pulmonary rehabilitation (PR) for bronchiectasis is supported by several studies [7,8].” An overview of the possible therapeutic options is given in Table 1.
Source: Joint Annual Meeting of the Swiss Society of Pneumology (SGP), the Swiss Society of Pediatric Pneumology (SGPP), the Swiss Society of Thoracic Surgery (SGT) and the Swiss Association of Endoscopy Personnel (SVEP), May 8-9, 2014, Interlaken.
Literature:
- Martínez-García MA, et al: Factors associated with lung function decline in adult patients with stable non-cystic fibrosis bronchiectasis. Chest 2007 Nov; 132(5): 1565-1572.
- Murray MP, et al: A randomized controlled trial of nebulized gentamicin in non-cystic fibrosis bronchiectasis. Am J Respir Crit Care Med 2011 Feb 15; 183(4): 491-499.
- Serisier DJ, et al: Inhaled, dual release liposomal ciprofloxacin in non-cystic fibrosis bronchiectasis (ORBIT-2): a randomised, double-blind, placebo-controlled trial. Thorax 2013 Sep; 68(9): 812-817.
- Haworth CS, et al: Inhaled colistin in patients with bronchiectasis and chronic Pseudomonas aeruginosa infection. Am J Respir Crit Care Med 2014 Apr 15; 189(8): 975-982.
- Wu Q, et al: Long-term macrolides for non-cystic fibrosis bronchiectasis: a systematic review and meta-analysis. Respirology 2014 Apr; 19(3): 321-329.
- Kellett F, Robert NM: Nebulised 7% hypertonic saline improves lung function and quality of life in bronchiectasis. Respir Med 2011 Dec; 105(12): 1831-1835.
- Ong HK, et al: Effects of pulmonary rehabilitation in bronchiectasis: A retrospective study. Chron Respir Dis 2011; 8(1): 21-30.
- Newall C, Stockley RA, Hill SL: Exercise training and inspiratory muscle training in patients with bronchiectasis. Thorax 2005 Nov; 60(11): 943-948.
HAUSARZT PRAXIS 2014; 9(7): 47-48











