A proportion of patients with severe eosinophilic bronchial asthma show inadequate effects under IL-5 antibody therapy. Switching to an IL-5 receptor antibody may promise success under certain conditions. A recent study investigated who would particularly benefit from a change.
All pulmonologists know the problem: there is a wide range of antibodies in patients with Th2-weighted bronchial asthma and now the task is to choose the right drug for the patient. It is known from studies that about a quarter of patients respond non-significantly to anti-eosinophil therapy despite actually “correct” selection criteria and the presence of eosinophils. This group is grouped together as non-responders. In responders, lung function (at least in some) and quality of life improve markedly with therapy; residual volume may also decrease; all patients have a decrease in eosinophils and a majority have an improvement in ACT.
Switching antibody therapy from omalizumab to mepolizumab may improve asthma control and decrease exacerbations. Considering that anti-IL-5 and anti-IL-5 receptor therapy with an antibody provide different starting points, the consequence is that switching may be a possible therapeutic option: With anti-IL-5 the messenger is intercepted, with anti-IL-5 receptor antibody just the receptor and by cytotoxic T cells the eosinophils are further reduced.
83% have benefited from conversion
PD Dr. Hendrik Suhling, Department of Pneumology, Hannover Medical School (D), presented a multicenter study in which several German centers participated [1]. 665 patients were included who received anti-IL-5 therapy. Of these, 70 patients were identified who were switched due to lack of response; sufficient data were available from 60 of these patients for further evaluation. Fifty participants in this group continued to receive therapy, and 10 had to discontinue it or were switched on or back. The researchers defined a baseline time point prior to antibody (AK) therapy and compared this to a time point of therapy under the first AK or just before switching to the second AK after 4 months. There was a balanced sex ratio, the median age was 54 years, the collective was slightly heavier compared to the normal population, matching 68% of the group had long-term steroid therapy with a mean of 10 mg prednisolone per day.
Therapy was more often mepolizumab than reslizumab, 40% were prior smokers, and over half had chronic rhinosinusitis as a comorbidity. The reasons for the switch were manifold, and in some cases there were multiple triggers (Fig. 1) . In particular, exacerbations were a problem, as was the need for further steroid therapy, poor exercise tolerance, and poor lung function or the assumption that this could still be improved.

Fifty of 60 patients (83%) benefited from the change. Of the 10 patients (17%) who did not continue therapy, 4 had no response to therapy, 2 experienced a decrease in efficacy, and one each experienced weight loss, coronary spasm, there was no effect on nasal polyps, and chronic urticaria developed. Two of these patients were subsequently switched back to the original anti-IL-5 antibody, two to an anti-IL-4R antibody (dupilumab), and the others had their therapy terminated without replacement.
Criteria must be defined
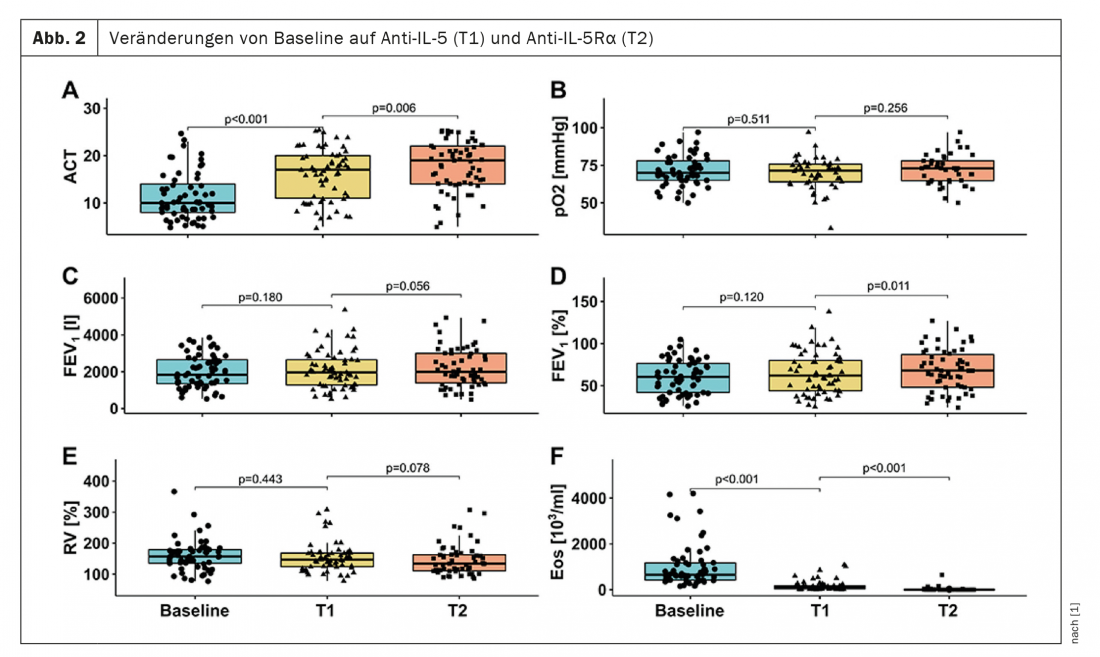
The results of the study already showed a significant improvement in the ACT under the first AK therapy compared to baseline, but this was further improved under the second AK. The eosinophils – possibly also as a reason for this improvement – could also be reduced even further after the change from AK1 to AK2. Lung function tended to improve, but only significantly under the second AK therapy. The residual volume could only be reduced by trend, the pO2 not significantly at all (fig. 2) . The steroid dose decreased again under the second AK therapy.
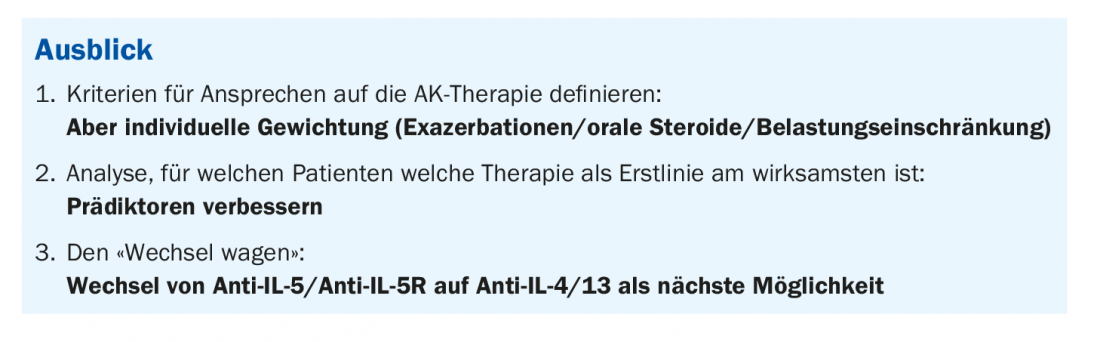
In conclusion, Dr. Suhling found that switching AK therapy increased responder rates, with nearly 90% improvement in patients. The only question that remains open is which patients will benefit from a changeover. So the change may be effective in some, but the question is whether a cut-off in eosinophils really counts. The expert considers the responder criteria to be a sensitive issue; they would have to be defined individually in order to enable therapy optimization in the future, even with objective control (box).
Source: Lecture “Switching antibody therapy in severe eosinophilic bronchial asthma from anti-IL-5 to anti-IL-5 receptor antibodies“ in the session “Free lectures of the section Allergology and Immunology“. 61st Congress of the German Society for Pneumology and Respiratory Medicine e.V., 3.6.2021.
Congress: DGP 2021 digital
Literature:
- Drick N, Milger K, Seeliger B, et al: Switch from IL-5 to IL-5 receptor α antibody treatment in Severe Eosinophilic Asthma. J Asthma Allergy 2020; 13: 605-614; doi: 10.2147/JAA.S270298.
InFo PNEUMOLOGY & ALLERGOLOGY 2021; 3(3): 27-28 (published 9/17-21, ahead of print).