As with other skin diseases, research into the role of the microbiome and immunological factors is a current focus of research efforts in acne and rosacea. Since both are multifactorial inflammatory dermatoses, there are correspondingly different therapeutic approaches. For the treatment of acne, topical application of an androgen receptor inhibitor has been shown to be effective in a recent study. And in severe papulopustular rosacea, one study demonstrated the superiority of a combination of topical and systemic therapy compared with monotherapy.
At the EADV Annual Meeting in October 2020, Prof. Lajos Kemény, MD, from the Department of Dermatology, University of Szeged (Hungary), gave an update on important developments and new findings in the field of acne and rosacea – both multifactorial diseases in which inflammatory processes and the composition of the skin microbiome play an important role in the pathomechanism and for derived therapeutic approaches [1].
Low phylotype diversity of C. acnes/P. acnes
The role of the microbiome in inflammatory dermatoses is increasingly the focus of experts. While pathogenic microbiota induce increased cytokine production followed by inflammatory responses, commensal microorganisms of the skin support the innate immune system by, among other things, producing antimicrobial peptides. With regard to atopic dermatitis, the cutaneous microbiome of atopic skin has been found to be less diverse compared to non-lesional skin. With regard to acne, it is nowadays also assumed that a loss of commensal diversity of the skin microbiome plays an important pathophysiological role. Recent studies show that a loss of diversity of phylotypes of C. acnes/P. acnes is a trigger factor for activation of the immune system, which ultimately results in cutaneous inflammation [2]. Cutibacterium acnes (C. acnes) is a subtype of the genus Propionibacterium acnes (P. acnes), which also occurs on healthy skin. Both P. acnes and C. acnes strains can be classified into the following six phylotypes based on multi-locus sequence typing: IA1, IA2, IB, IC, II, and III [3,4]. Skin affected by acne is characterized, among other things, by an excessively high proportion of type IA1 compared to healthy skin. As shown in a review paper by Contassot et al. different P. acnes strains induce pathogenic and protective Th17 immune responses, respectively [5]. Accordingly, inflammatory phylotypes cause a Th17-mediated boost in cytokine production – particularly IFN-γ – followed by specific activation of keratinocytes and sebocytes, whereas protective phylotypes induce Th17 cells to produce IL10 [1,5].
Novel topical androgen receptor inhibitor reduces acne lesions
Based on these and further advances in the understanding of the pathophysiological basis, new therapeutic options may emerge in the future to complement the currently established treatment options [6]. There are several new drug candidates that are currently being investigated, Prof. Kemény said. Among anti-inflammatory agents, these include anti-IL17A, and anti-IL1-beta, as well as PDE inhibitors [1]. Another therapeutic starting point is the influence of the C. acnes colonization, which is a target of newer antibiotics such as pentobra, sarecycline, or rifampicin, as well as antimicrobial peptides, bacteriophages, or vaccines against C. acnes. Another focus of research is in the area of agents that reduce sebum production such as substances with effects on androgen-dependent sebum production or alpha-MSH, PPAR modulators, acetylcholine inhibitors, acetyl coenzyme A carboxylase inhibitors, lupeol plant extract or 5-alpha reductase inhibitors.
One example of a new therapeutic approach that is well advanced in development is a topical application of antiandrogens. Clascoterone is a novel topical androgen receptor inhibitor and is being studied for acne as a cream at 1% concentration [7,8]. The clascoterone metabolite cortexolone, formed by remodeling processes in the skin, intervenes at multiple, distinct points in the pathogenesis of acne and inhibits downstream dihydrotestosterone-stimulated signal transduction of androgen receptors. In two phase III studies in a total of 1440 acne patients in the age range 9-50 years, after 12 weeks of once-daily treatment with 1 g clascoterone cream 1%, there was a 29.8% reduction in non-inflammatory lesions compared to 18.9% in the vehicle group. For inflammatory lesions, a 46.2% reduction was measurable in the clascoterone-treated cohort over the same period, whereas a 32.7% reduction was observed in the carrier cohort. The outcome parameters used were an IGA score of 0 (lesion-free) or 1 (nearly lesion-free), symptomatology improved by at least 2 points since baseline, and an absolute change in noninflammatory and inflammatory lesions at week 12. Not only did treatment with clascoterone cream 1% prove effective, but the safety profile was also favorable [7,8].
Cathelicidin production and protease activity are increased in rosacea
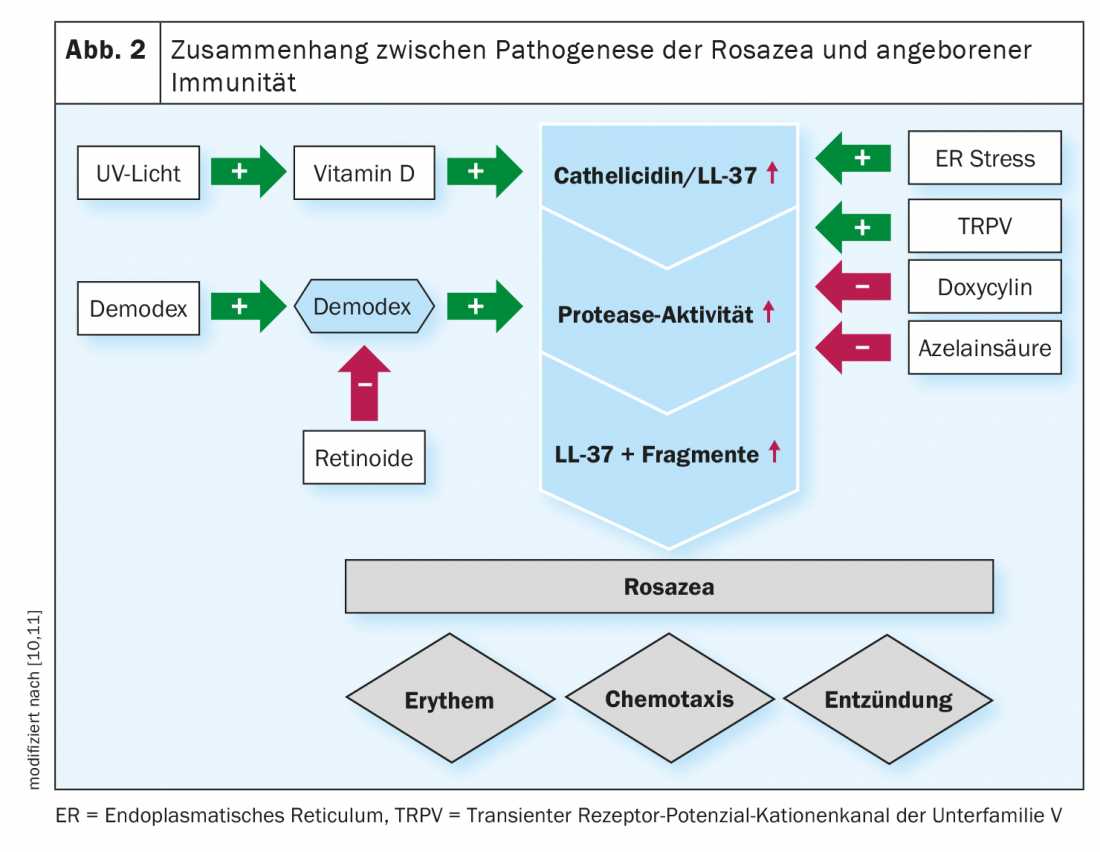
Rosacea is also a complex multifactorial inflammatory dermatosis. As known from twin studies, genetic determinants and environmental factors are approximately equally involved in pathogenesis [9]. With regard to immune dysregulation, rosacea sufferers have been found to exhibit specific patterns and cutaneous concentrations of cathelicidin peptides, more specifically cathelicidin LL-37, which are antimicrobial peptides secreted by the innate immune system. Increased cathelicidin production and protease activity are induced by Toll-like receptor 2 (TLR2), among others, and contribute to a state of inflammation (Fig. 2) [10,11]. There are also various therapeutic approaches to rosacea. The ROSCO panel’s treatment recommendations are based on a phenotype-based diagnosis starting from the premise that individualized therapy, primarily based on symptoms, is most promising. The main symptoms include “flushing”, persistent erythema, telangiectasias, papules with/without pustules, phymatous changes of the skin and ocular manifestations [10].
Management of ocular rosacea remains a challenge
It is estimated that up to 50% of rosacea sufferers develop eye involvement. Because cutaneous and ocular symptoms do not necessarily correlate, this is often overlooked [12]. Typical symptoms of ocular rosacea are associated with inflammation of the eyelid and, in addition to a foreign body sensation, include dry, burning or watery eyes and redness of the eyelid margins. Possible ocular involvement should be inquired about in each patient. Blepharitis and conjunctivitis are the most common manifestations of ocular rosacea. If the tear film is significantly disrupted, problems such as blurred vision or increased sensitivity to light may occur. The treatment of ocular rosacea usually proves difficult, the speaker explained [1]. The treatment algorithm of the ROSCO panel recommends the following approach [1,13]: Eyelid hygiene is essential in all degrees of severity. For moderate forms, the use of ciclosporin is advised, and for severe forms, cortisone-containing topical preparations. The recommended systemic therapy, regardless of severity, is doxycycline 40 mg with modified release (MR); higher doses may be considered for severe manifestations. Eyelid margin hygiene can reduce the risk of inflammation, so this is extremely important. In addition, the eye should always be kept moist, for example by means of lipid-containing tear substitutes.
Source: EADV Annual Meeting 2020
Literature:
- Kemény L: Update on acne and rosacea. Prof. Lajos Kemény, MD, EADV Annual Meeting 2020 (Virtual), Oct. 30, 2020.
- Dagnelie M-A, et al: Cutibacterium acnes phylotypes diversity loss: a trigger for skin inflammatory process. JEADV 2019; 33(12): 2340-2348.
- Teramoto K, et al: Classification of Cutibacterium acnes at phylotype level by MALDI-MS proteotyping. Proc Jpn Acad Ser B Phys Biol Sci 2019; 95(10): 612-623.
- McDowell A, et al: The opportunistic pathogen Propionibacterium acnes: insights into typing, human disease, clonal diversification and CAMP factor evolution. PLoS One 2013; 8(9): e70897.
- Contassot E, French LE: Propionibacterium acnes Strains Differentially Regulate the Fate of Th17 Responses in the Skin. J Invest Dermatol 2018; 138(2): 251-253.
- Nast A, et al: European evidence-based (S3) guideline for the treatment of acne – update 2016 – short version. JEADV 2016; 30(8) : 1261-1268.
- Hebert AA: https://aadhighlights2019.com/articles/clascoterone-topical-cream-1/read (last accessed 2/17/2021).
- Hebert A, et al. Efficacy and Safety of Topical Clascoterone Cream, 1%, for Treatment in Patients With Facial Acne. Two Phase 3 Randomized Clinical Trials. JAMA Dermatol 2020;156(6):621-630.
- Aldrich N, et al: Genetic vs Environmental Factors That Correlate With Rosacea: A Cohort-Based Survey of Twins. JAMA Dermatol. 2015; 151: 1213-1219.
- Reinholz M, et al: JDDG 2016; 14(S6): https://doi.org/10.1111/ddg.13139_g
- Reinholz M, Ruzicka T, Schauber J: Cathelicidin LL-37: an antimicrobial peptide with a role in inflammatory skin disease. Ann Dermatol 2012; 24: 126-135.
- Russ V: Rosacea: The red danger, Pharmazeutische Zeitung (Online), 15.02.2016.
- Schaller M, et al: Recommendations for rosacea diagnosis, classification and management: update from the global ROSacea COnsensus 2019 panel. British Journal of Dermatology 2020; 182(5): 1269-1276.
- McDowell A: Over a Decade of recA and tly Gene Sequence Typing of the Skin Bacterium Propionibacterium acnes: What Have We Learned? Microorganisms 2018, 6(1): 1.
- Schaller M, et al: Rosacea treatment update: recommendations from the global ROSacea COnsensus (ROSCO) panel. British Journal of Dermatology 2017; 176(2): 465-471.
- Schaller M et al: A randomized phase 3b/4 study to evaluate concomitant use of topical ivermectin 1% cream and doxycycline 40-mg modified-release capsules, versus topical ivermectin 1% cream and placebo in the treatment of severe rosacea J Am Acad Dermatol 2020; 82: 336-343.
DERMATOLOGIE PRAXIS 2021; 31(1): 39-40 (published 2/22/21, ahead of print).