At the annual meeting of the Swiss Society of Cardiology in Zurich, a main session was dedicated to acute heart failure. New findings and studies from the pharmacological field were presented and therapeutic strategies were discussed. In cardiogenic shock, the most severe form of acute heart failure, ECMO offers a “bridge-to-decision.” How exactly this is carried out and what outcome can be expected was also the topic of the event.
“There has been great progress in the field of chronic heart failure in recent years. These are also urgently needed in acute heart failure, because mortality is unacceptably high: after three years, about half of the patients die. This is a higher value than for many types of cancer,” said Prof. Christian Müller, MD, Cardiology University Hospital Basel, by way of introduction. “Why is that? We often underestimate the severity and urgency of acute heart failure. The high mortality has at least partly to do with the fact that we undertreat patients.”
Hopeful Urodilatin and Serelaxin – how far along are they in development?
Currently investigated therapeutic strategies follow two principles: The goals are to treat as early as possible and to vasodilate. One of the new substances being researched is called Ularitide (Urodilatin). The following pharmacological effects have been described:
- Hemodynamic effect (vasodilation) on veins and arteries
- Bronchodilation
- Neurohumoral effect: decrease in plasma concentrations of renin, aldosterone, and angiotensin II. Endothelin levels also decrease.
- Renal effect: diuresis and natriuresis are promoted.
A randomized, controlled phase IIb trial called SIRIUS II [1], in which 221 patients with decompensated heart failure received either placebo or urodilatine at doses of 7.5, 15, or 30 ng/kg/min received as a continuous 24-hour infusion in addition to standard therapy showed not only a significant reduction in pulmonary capillary occlusion pressure (PCWP) at six hours and improvement with respect to dyspnea, but also an encouraging trend with respect to mortality. The phase III TRUE-AHF trial, the results of which are expected towards the end of this year, is now expected to demonstrate that cardiovascular mortality can be positively influenced with urodilatine also in the long term (co-primary endpoint). In May 2015, recruitment of 2152 patients with acute heart failure was completed. Due to the favorable benefit-response profile, the dose of 15 ng/kg/min (infusion over 48 hours) is used in TRUE-AHF.
Serelaxin is a recombinant form of human relaxin 2, which in pregnant women causes renal and hemodynamic processes that help cope with increased physical demands. Increase in cardiac output, decrease in systemic vascular resistance, improvement in renal plasma flow, and increase in glomerular filtration rate can also be used in acute heart failure. In RELAX-AHF [2], it was shown in 1161 patients with acute heart failure that intravenous administration of 30 μg/kg/d serelaxin, given no later than 16 hours after onset and then for 48 hours, was significantly superior to placebo in terms of improvement in dyspnea (but only according to the visual analog scale, not the dyspnea Likert scale). A long-term mortality benefit was also found, which gives hope for future studies: the risk of death was almost 40% lower in the Serelaxin group than in the control group after 180 days (HR 0.63; 95% CI 0.42-0.93; p=0.019). Patients also suffered less end-organ damage [3]. Currently, the RELAX-AHF-II study is ongoing.
Effective use of available substances
In addition to the development of new drugs, there are also innovative concepts for the use of the active substances already available. One possible hypothesis is that early, continuous, high-dose vasodilation improves outcome. Such a therapeutic strategy is currently being tested by the GALACTIC study at the University Hospital Basel. The aim is to elicit safety and efficacy of early, goal-directed reduction of preload and afterload with a target systolic blood pressure of 90-110 mmHg. This is achieved by means of aggressive maximal vasodilation (sublingual/transdermal nitrates, rapid titration of ACE inhibitors). Participants are patients with acute heart failure who are not being treated in the intensive care unit. In the second arm, therapy is performed according to ESC guidelines. Patients are currently being recruited [4].
Extracorporeal membrane oxygenation (ECMO)
PD Markus Wilhelm, MD, Clinic for Cardiovascular Surgery, University Hospital Zurich, spoke about extracorporeal membrane oxygenation (ECMO). This is indicated in cardiogenic shock, heart failure after previous cardiac surgery (postcardiotomy failure), and respiratory failure. As a “bridge-to-decision,” ECMO in cardiogenic shock causes short-term improvement in circulation and recovery or unloading of organs. It also allows for neurological evaluation. Finally, you have to decide between different options: In the best case, can the machine be weaned? Or does it need a ventricular assist device (VAD) resp. a heart transplant? At worst, you have to let the patient die.
In respiratory failure, veno-venous ECMO is used; in circulatory failure, veno-arterial ECMO is used. In the latter, deoxygenated blood is pumped to the oxygenator through a large cannula in the right inguinal vein (femoral vein). From there, the oxygenated blood returns directly to the main circulation without passing through the heart via a large cannula in the left inguinal artery (femoral artery). Possible complications include hemorrhage, either at the site of entry or internally (cerebral), infection, and hypo/hyperperperfusion syndromes. To avoid hypoperfusion and compartment syndrome in veno-arterial ECMO, the venous and arterial cannulae are not inserted on the same side.
Survival with ECMO in cardiogenic shock.
Dr. Wilhelm presented three studies-two of them from 2015-that addressed outcomes of ECMO in patients with cardiogenic shock (Table 1).
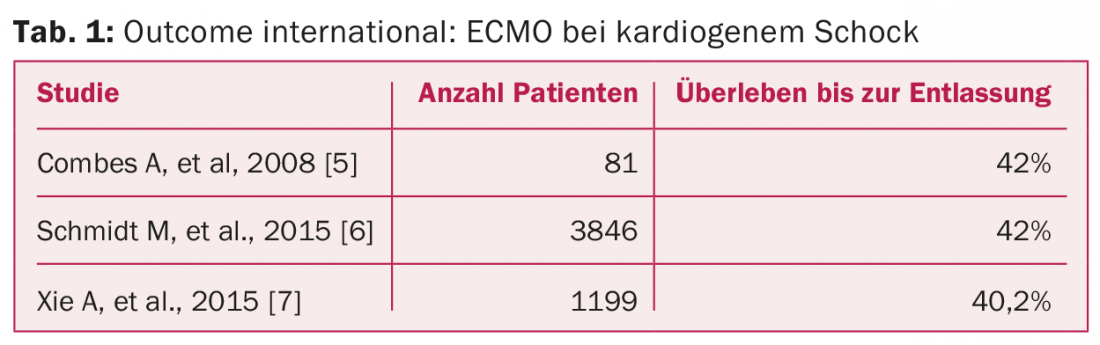
“Overall, it shows that less than half of the patients who receive ECMO survive and can be discharged from the hospital. This is consistent with our own experience at the UniversitySpital Zurich: of 57 USZ patients, 27, or 47.4%, were still alive after 30 days. Discontinuation had been possible in 16, 11 had required a VAD,” Dr. Wilhelm explained. Patient characteristics of survivors showed that they tended to be younger and had significantly lower lactate levels at baseline. After one year, 36.8% were alive; after two years, 32.2%; and after five years, 29.8% (thus, a plateau occurred). “A very important contributor to survival rates is the fact that cardiogenic shock not only consists of a profound output, but often also represents an inflammatory state,” the speaker concluded.
Source: SGK Congress, June 10-12, 2015, Zurich
Literature:
- Mitrovic V, et al: Eur Heart J 2006 Dec; 27(23): 2823-2832.
- Teerlink JR, et al: Lancet 2013 Jan 5; 381(9860): 29-39.
- Metra M, et al: J Am Coll Cardiol 2013 Jan 15; 61(2): 196-206.
- Goal-directed Afterload Reduction in Acute Congestive Cardiac Decompensation Study (GALACTIC). ClinicalTrials.gov Identifier: NCT00512759.
- Combes A, et al: Crit Care Med 2008 May; 36(5): 1404-1411.
- Schmidt M, et al: Eur Heart J 2015 Jun 1. DOI: http://dx.doi.org/10.1093/eurheartj/ehv194 [Epub ahead of print].
- Xie A, et al: J Cardiothorac Vasc Anesth 2015 Jun; 29(3): 637-645.
CARDIOVASC 2015; 14(4): 32-33











