With regard to cardiac and renal protection, it is increasingly recommended to combine metformin initially with an SGLT-2 inhibitor or a GLP-1 receptor agonist. In contrast, sulfonylureas and DPP-4 inhibitors have become less important. However, not all patients in Switzerland who could benefit from the advantages of the new drug groups actually receive them. In this respect, experts believe there is a need to catch up – and for good reasons.
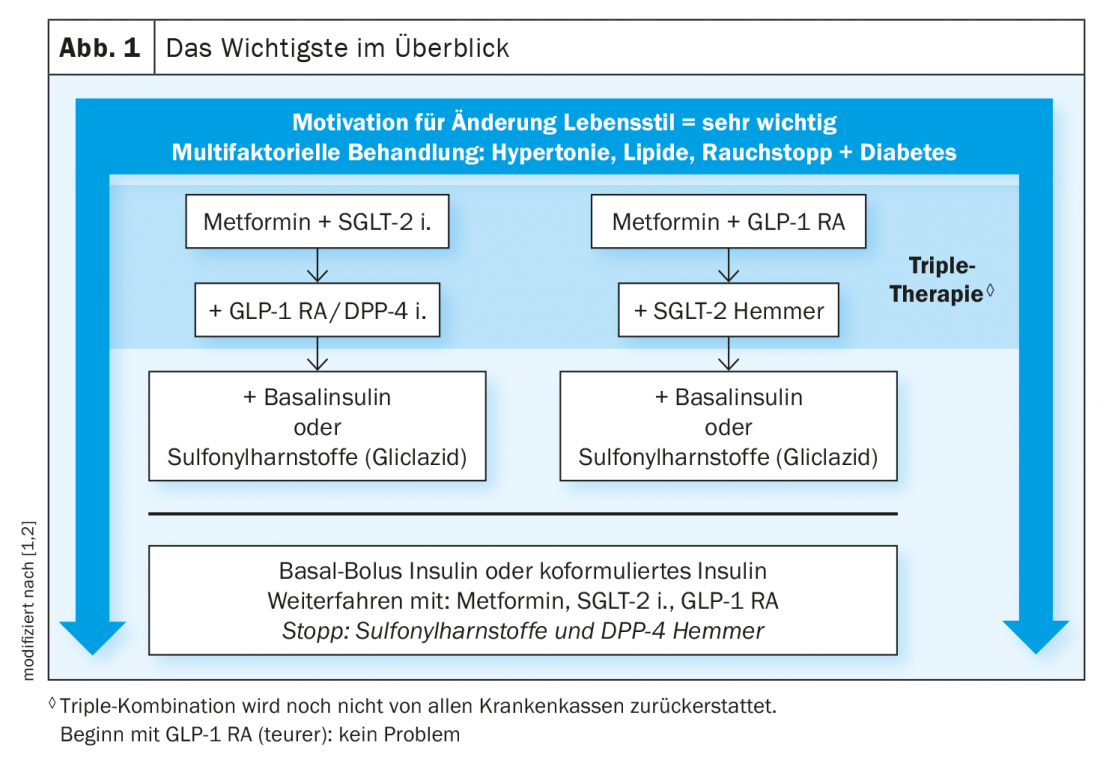
The current recommendations of the Swiss Society of Endocrinology and Diabetology (SGED) for the treatment of type 2 diabetes mellitus provide a good basis for the general practitioner to choose the best possible treatment strategy together with the patient, explains Prof. Roger Lehmann, M.D., Senior Physician, Department of Endocrinology, Diabetology and Clinical Nutrition, University Hospital Zurich. [1,2]. In the context of modern diabetes therapy, glycemic control is an important therapeutic goal, but a multifactorial risk reduction beyond this is targeted (box, Fig. 1). The most important criteria for the therapy decision can be clarified on the basis of the following four questions:
- Does the patient need insulin? This is true for about 25% of type 2 diabetics. In these cases, you can start with basal insulin or with coformulated insulin.
- Is the eGFR below 60 ml/min? This also applies to about a quarter of patients. Here, the recommendation is to prescribe SGLT-2-i or GLP-1-RA.
- Does the patient have cardiovascular disease? This has been the case for between a quarter and a third. SGLT-2-i or GLP-1-RA should also be used in these cases.
- Is heart failure present? This is fulfilled by about 10-25% of type 2 diabetics. Here, for all forms of heart failure, SGLT-2-i should be prescribed.
Although first-line therapy is still metformin, provided the glomerular filtration rate (eGFR) is above 30 ml/min, in many cases a combination with an SGLT-2-i and/or a GLP-1 RA is useful. If ineffective, a triple combination of metformin plus SGLT-2-i plus GLP-1-RA should be prescribed, the speaker advised. If this is not successful either, insulin is indicated.
Early combination with SGLT-2-i and/or GLP-1-RA recommended.
Both SGLT-2-i and GLP-1-RA – in contrast to metformin – were shown to have an additional benefit in terms of 3-point MACE and prevention of heart failure as well as a positive effect on the maintenance of eGFR in the large cardiovascular endpoint studies. Prof. Lehmann argues that type 2 diabetics in particular who have chronic kidney disease should all receive SGLT-2-i or GLP-1-RA – but currently only about half of patients with this indication are prescribed it. The official recommendation that therapy with SGLT-i can be maintained until dialysis is required has so far been made only for canagliflozin, but according to current data, this should actually also apply to empagliflozin, dapagliflozin, and ertugliflozin. “It will be some time before the official recommendations come then,” the speaker explained [1].
With regard to cardiovascular risk, he said, it is important to look not just at a ten-year period, but at the entire lifespan. The corresponding cumulative risk of a poorly controlled HbA1c over many years would be considerable.
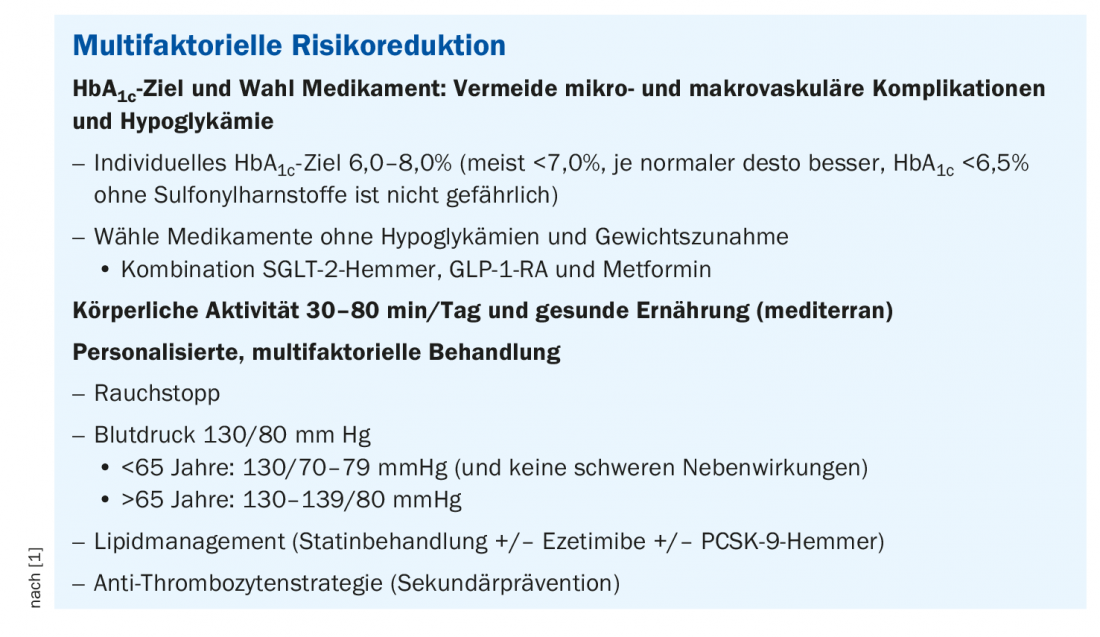
Consider individual patient characteristics
Multifactorial diabetes therapy also involves treating other important risk factors, particularly hypertension, smoking, and dyslipidemia. In type 2 diabetics over 50 years of age, a reduction in LDL of 1 mmol, a reduction in cardiovascular risk of 50-55%, the speaker said. In obese patients and generally when weight loss is desired, as well as in younger patients with long life expectancy, GLP-1-RAs are more appropriate as an initial combination to metformin. There is evidence from numerous studies that GLP-1-RA reduces the inflammation characteristic of type 2 diabetes, both cardiac and vascular [3]. “Certainly they are to be preferred over DPP-4 inhibitors,” the speaker added. The main mechanism of action of GLP-1-RA is to increase insulin, decrease glucagon, and reduce appetite. According to current data, SGLT-2-i have a small advantage over GLP-1-RA in reduced eGFR [1]. (Table 1). Other patient characteristics more suggestive of SGLT-2-i are: Suspected heart failure and older age. In patients who cannot tolerate GLP-1-RA, SGLT-2-i may be substituted if BMI is less than 28. Prof. Lehmann describes the mechanisms of action of SGLT-2-i as follows: “Glucose is filtered in the kidney and 90% of the reabsorption happens through SGLT-2 – if you inhibit that, a substantial portion of the glucose is excreted in the urine” [1]. The lower the kidney function, the less sugar is excreted and the lower the HbA1c reduction. “But the nephroprotective effect remains,” emphasized the speaker [1]. The main side effect of SGLT-2-i is genital mycotic infections, as urinary glucose excretion provides optimal growth conditions for Candida.

Caution with sulfonylureas and DPP-4 inhibitors.
The sulfonylureas, which were also previously used in Switzerland, have lost their importance in this country. This is mainly due to the weight gain shown in studies and the increased risk of hypoglycemia, explains Prof. Lehmann. Whereas the diabetes subtypes MODY 1, MODY 3 and neonatal diabetes respond very well to sulfonylureas and one can therefore consider this therapy option in the patients concerned, the speaker relativizes. It is important to note, however, that sulfonylureas should never be administered in combination with insulin, as this carries a 40-fold increased risk of hypoglycemia. DPP-4 inhibitors have also become less important. This was mainly due to a lack of additional cardiovascular benefit in the corresponding endpoint studies (CARMELINA, TECOS, SAVOR-TIMI) [1,5–7]. There are several explanations for the fact that DPP-4 inhibitors are nevertheless frequently used: on the one hand, these drugs reliably lower HbA1c; on the other hand, they can be prescribed without complications and do not lead to hypoglycemia or weight gain. However, because DPP-4 inhibitors have not shown effects on cardiovascular events, they are now considered only a second choice after metformin, the speaker explained. Because: “All patients with type 2 diabetes have a high or very high risk,” says Prof. Lehmann.
What else is important to consider? According to the “Sick Day Rules” of the SGED, the intake of metformin and SGLT-2-i should be temporarily paused if the following symptoms occur: vomiting, diarrhea, hospitalization, surgery (also e.g. before colonoscopy). This due to the risk of ketoacidosis with SGLT-2-i and lactic acidosis with metformin, respectively, according to the speaker [1,4].
Congress: FomF General Internal Medicine Update Refresher
Literature:
- “Type 2 Diabetes – An Overview,” Prof. Roger Lehmann, MD, Forum for Continuing Medical Education, Update Refresher, 5/19/2022.
- Lehmann R, et al: Recommendations of the Swiss Society of Endocrinology and Diabetology (SGED/SSED) for the treatment of type 2 diabetes mellitus, 2020; www.sgedssed.ch/diabetologie/sged-empfehlungen-diabetologie, (last accessed June 30, 2022).
- Drucker DJ: The cardiovascular biology of glucagon-like peptide-1. Cell Metab 2016; 12; 24: 15-30.
- SGED: Sick day rules, www.sgedssed.ch/diabetologie/sick-day-rules-card, (last accessed Jun. 30, 2022).
- Rosenstock J, et al; CARMELINA Investigators. Effect of Linagliptin vs Placebo on Major Cardiovascular Events in Adults With Type 2 Diabetes and High Cardiovascular and Renal Risk: The CARMELINA Randomized Clinical Trial. JAMA 2019; 321(1): 69-79.
- Green JB, et al; TECOS Study Group. Effect of sitagliptin on cardiovascular outcomes in type 2 diabetes. N Engl J Med 2015; 373(3): 232-242.
- Scirica BM, et al; SAVOR-TIMI 53 Steering Committee and Investigators. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med 2013; 369(14): 1317-1326.
- Schneider L, Lehmann R: Decision support for personalized therapy in type 2 diabetes mellitus. “Swiss Diabetes Guide. Swiss Med Forum 2021; 21(1516): 251-256.
HAUSARZT PRAXIS 2022; 17(7): 20-21