The standard therapy for treating all manifestations of reflux disease is proton pump inhibitors (PPI). Despite a high success rate, there are occasional patients with an insufficient response to therapy. In these cases, an add-on treatment with alginates has proven to be effective.
Worldwide, the prevalence of reflux symptoms is reported to be 10-25%, with large geographic variations [1,2]. For those affected, the family doctor is often the first point of contact. According to the Montreal classification, gastroesophageal reflux disease (GERD) is present when reflux of gastric contents causes bothersome symptoms and/or complications [3]. It is a multifaceted complaint (overview 1). Typical symptoms include heartburn, regurgitation and acid regurgitation. Other common manifestations include upper abdominal pain and sleep disturbances due to nocturnal reflux. Atypical symptoms include globus sensation and throat clearing. Visible inflammation of varying severity (Los Angeles grades A through D) and peptic stenosis may develop in the esophagus. In addition to the type of symptoms and the frequency, correlations to the factors nutrition and stress can also be queried during the anamnesis [4]. Influenceable risk factors include obesity and tobacco smoking, and about three quarters of all pregnant women suffer from reflux [2].

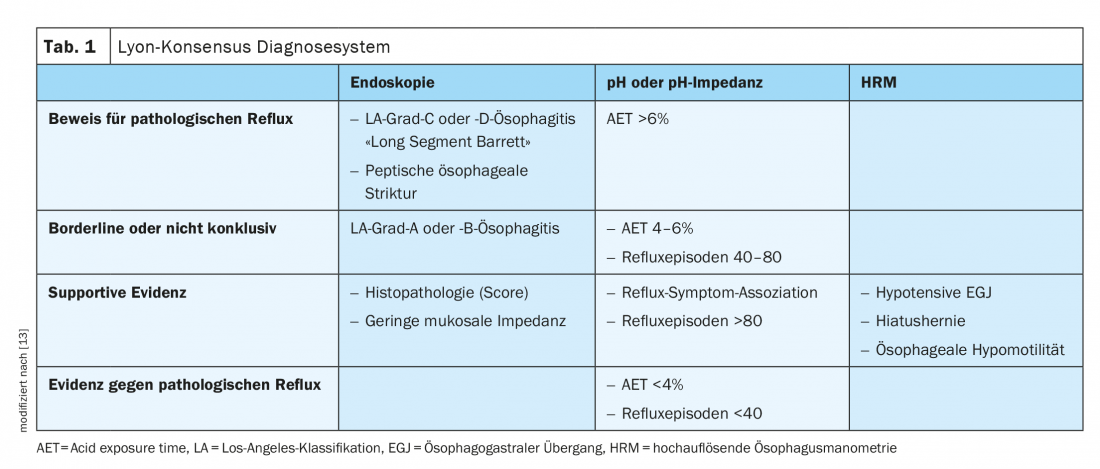
Lyon consensus as a modern diagnostic system
For the diagnostic detection of reflux disease, impedance pH-metry over 24 hours is nowadays considered the method of choice [5,6]. Impedance measurement is performed via a probe placed in the esophagus and detects any movement of contents in the esophagus including direction and pH. This technique allows accurate quantification and assignment of symptoms. A confirmed diagnosis is particularly crucial in cases of inadequate symptom control despite PPI therapy. A modern diagnostic classification including various procedures is based on the Lyon Consensus Conference (Table 1) [7]. Accordingly, the diagnosis of GERD is considered confirmed when there is severe reflux esophagitis (Los-Angeles grade C or D), peptic stricture, histologically confirmed Barrett’s metaplasia greater than 1 cm, or esophageal acid exposure of >6% of the measured time (24 h) [7]. GERD is considered excluded with acid exposure <4% and <40 reflux episodes per day [7]. Proton pump inhibitors (PPIs) are considered standard therapy for reflux disease and are used successfully to inhibit acid in the stomach. In the acute phase, PPIs are initially used in high doses; when symptoms are relieved, the dose can be successively reduced until the maintenance dose is as low as possible [8]. Numerous studies have demonstrated the efficacy of PPIs compared with placebo and their superiority to other drugs [9].
What to do if there is a lack of response to PPI therapy
Patients who continue to have symptoms despite 8 weeks of PPI 1×/day are said to have persistent reflux esophagitis. If the diagnosis is confirmed, the first step should be to check whether there is room for improvement in terms of compliance. After that, medication can be tried according to the following scheme [10]:
- Double dose PPI (1-0-1) for 8 weeks.
- Antihistamine (e.g. Zantic 300 mg)
- Reflux blocker (e.g. Gaviscon 1-2 tbl. postprandially)
- Prokinetic (e.g. Motilium 10 mg)
In patients who respond inadequately to PPI therapy, it has been shown that acid pouch, which can be effectively treated locally by alginates, often plays a significant role in this [11]. As-needed supplemental administration of alginate has been shown to reduce persistent reflux symptoms and improve patients’ quality of life [11,12].
LOPA study confirms positive effects of alginates as add-on
In patients with inadequate response to PPI treatment, an open-label, multicenter, nonrandomized, noninterventional study investigated the effects of alginates as an add-on [11]. 11 GP practices in the greater areas of North Rhine-Westphalia and Rhineland-Palatinate participated between March 2016 and October 2017. The study was registered in the German Clinical Trials Registry. Included were 155 adult patients (54% women, median age 57 years*) with at least a 1-year history of GERD and continuous PPI therapy of ≥ 1 year resulting in inadequate symptom control. Six patients were excluded from the data analysis because they either did not take the study medication or did not attend the final visit. The median duration of disease was 8 years (range, 1-50 years), and the median duration of long-term PPI therapy was 6 years.
* median = 50% of the sample above and 50% below this mark
Affected individuals were treated with an alginate as needed (up to 4 ×/day) for 14 days. Study participants took a mean of three sachets of the study drug daily. The frequency of symptoms in the week before therapy and in the second week of treatment were recorded, as well as additionally the validated GERD-Q score. Satisfaction with therapy was rated by patients at baseline and at the end of the study on a 5-point Likert scale** (1=very dissatisfied, 5=satisfied). The primary end point was defined as improvement in satisfaction by ≥ 1 point.
** 1 point: n = 45, 2 points: n = 41, 3 points: n = 16, 4 points: n = 5
In 72% of patients, alginate therapy resulted in at least 1 point improvement in treatment satisfaction. Patients with a GERD Q score >8 were found to respond more frequently to therapy (81%). The reported improvement in related to all typical reflux symptoms and sleep disturbances. The treatment proved to be well tolerated.
Take-home messages
- Therapeutic goals for GERD include symptom control, healing of esophageal lesions, and prevention of complications [14].
- Proton pump inhibitors (PPIs) are the first-line drugs for the treatment of all manifestations of GERD and result in a satisfactory therapeutic effect in about 70% of patients, but occasionally there are cases of inadequate response [14].
- A reliable diagnosis is particularly important in patients with inadequate effect of PPI treatment and often requires a combination of different diagnostic procedures as noted in the Lyon Consensus (Table 1) [7].
- Alginates are an effective add-on therapy option when PPI effects are insufficient [14]. This is shown, among other things, by the results of the LOPA study conducted in 2016/2017, in which 11 GP practices in Germany participated [11]. In this study, alginate therapy as an add-on to PPI significantly improved treatment satisfaction in 72% of patients.
Literature:
- Richter JE, Rubinstein JH: Presentation and epidemiology of gastroesophageal reflux disease. Gastroenterology 2018; 154 (2): 267-276.
- Medix: www.medix.ch/media/gl_dyspepsie_2018_20.11.20_mh.pdf
- Vakil N, et al: The Montreal definition and classification of gastroesophageal reflux disease: a global, evidence-based consensus paper. Z Gastroenterol 2007; 45(11): 1125-1140.
- Lengliger J: Gastroesophageal reflux disease. Johannes Lenglinger, MD, Inselspital Bern. FOMF Basel, 29.01.2020.
- Labenz J, Labenz C: Reflux disease: PPI not always first choice. Pharmaceutical Newspaper (Online), May 02, 2019.
- Koop H, et al: S2k-Guideline: Gastroesophageal reflux disease guided by the German Society of Gastroenterology. Z Gastroenterol 2014; 52(11): 1299-1346.
- Gyawali CP, et al: Modern diagnosis of GERD: the Lyon consensus. Gut 2018; 67: 1351-1362.
- GI-Portal.com: http://dasgastroenterologieportal.de/Behandlung_mit_PPI_Protonenpumpeninhibitoren.html
- Mössner J: The Indications, Applications, and Risks of Proton Pump Inhibitors: A Review After 25 Years. Deutsches Ärzteblatt International 2016; 113(27-28): 477.
- Halama M: Slide presentation Marcel Halama, MD, Gastroenterology Practice, Zurich. Ulcer and reflux disease. FOMF Internal Medicine – Update Refresher, 04.12.2019, Zurich
- Müller M, et al: Alginate on demand as an add-on in case of insufficient effect of proton pump inhibitors in patients with gastroesophageal reflux disease. Dtsch Med Wochenschr 2019; 144(04): e30-e35.
- Labenz J, Koop H: Gastroesophageal reflux disease-what to do when PPIs are not sufficiently effective, tolerated, or desired? DMW-German Medical Weekly, 2017. 142(05): 356-366.
- Wiest R, Tutuian R: Work-up of esophageal complaints. Swiss Gastroenterology 2020; 1: 23-28.
- Labenz J, et al: Gastroesophageal reflux disease update 2021. The Internist 2020; 61: 1249-1263.
HAUSARZT PRAXIS 2021; 16(1): 34-35