Although the pathophysiological mechanisms of rosacea are not yet fully understood, there are consensus-based explanatory models. Consequently, the etiopathogenesis is multifactorial, with genetic and environmental components. The treatment should be individually adapted to the symptoms or the respective rosacea phenotype. Reducing the density of Demodex mites and anti-inflammatory effects are among the most important mechanisms of action of current drug therapies.
“The most relevant mechanisms of rosacea pathogenesis are immune dysregulation, neurovascular inflammation and an impaired skin barrier,” says Prof. Dr. Vincenzo Bettoli, MD, Università di Ferrara (I) [1]. The clinical manifestations of rosacea range from erythema and telangiectasia to papules, pustules and flushing in centrofacial skin areas. In addition, there is often periocular inflammation and sometimes cutaneous swelling and hyperplasia, known as phyma.
Multifactorial etiopathogenesis
In a retrospective observational study, 64 out of 130 rosacea patients reported having at least one family member with rosacea. This corresponds to a rate of 49.2% and supports the theory of a genetic predisposition [3]. A large twin study (n=550) showed that genetic factors explain 46% of the disease variance and environmental influences 54% [4]. A stronger association between NRS (National Rosacea Society) scores was observed in monozygotic twins than in non-monozygotic twins, which is further evidence of a genetic basis.
In a review article on the etiopathogenesis of rosacea published in 2023, the role of microbial dysbiosis, neuroimmune interactions, metabolic dysfunction and dysregulated sebaceous glands is emphasized with reference to recent study findings [2]. There are also numerous trigger factors that play a role in rosacea. These include heat, cold, spicy food, UV rays, alcohol, demodex mites and small intestinal bacterial overgrowth (SIBO) and oxidative stress [1,5]. Prof. Bettoli emphasized that there are many findings that point to the involvement of Demodex mites. With regard to diet, a secondary analysis published in 2021 concluded that although there is evidence that certain foods are associated with rosacea exacerbation, no general recommendations can be derived from this [6].
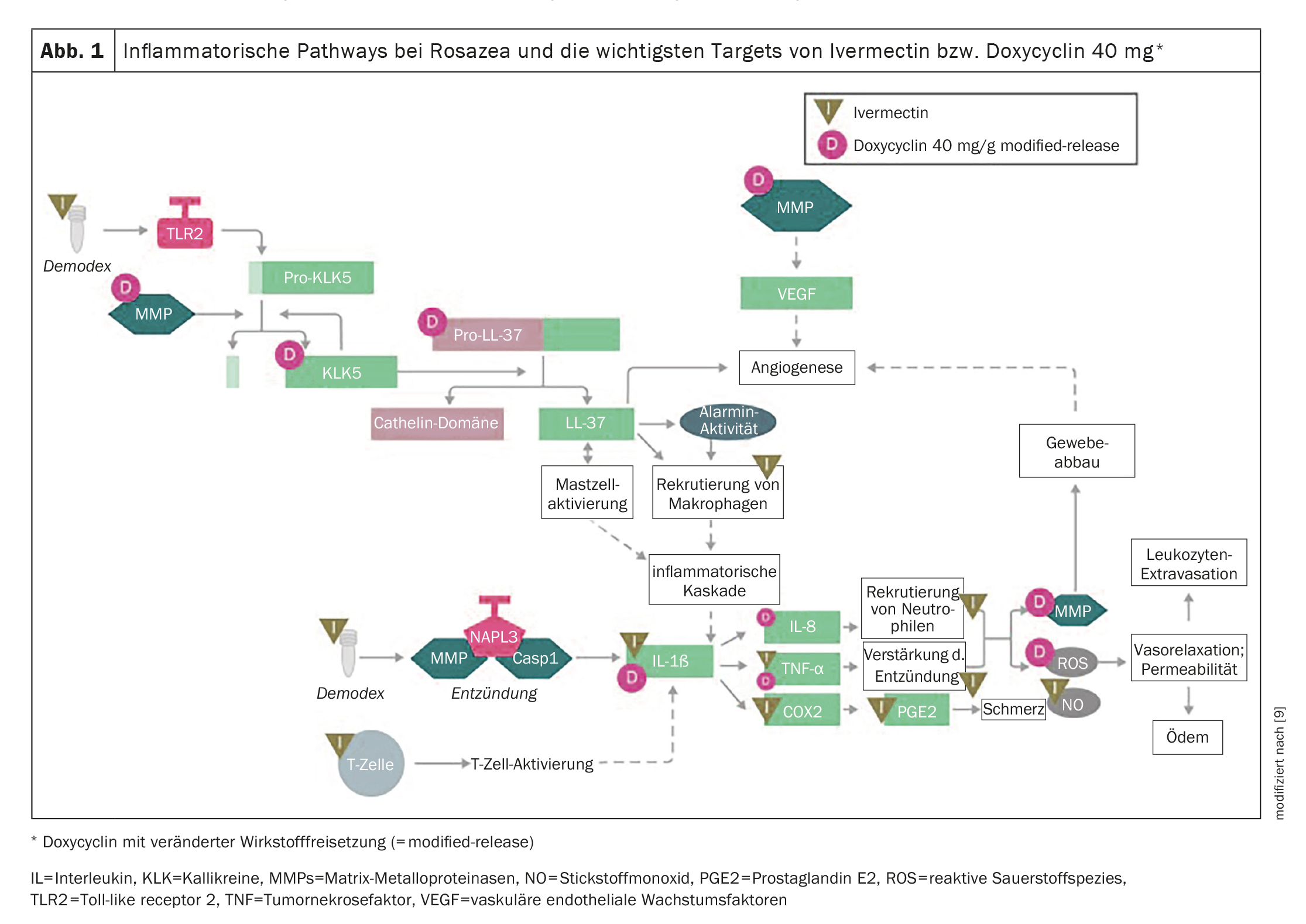
Therapeutic targets of ivermectin and doxycycline
Rosacea patients often have an impaired quality of life and low self-esteem [2]. The aim of the therapy is to achieve skin that is as free of blemishes as possible. Ivermectin (Soolantra® cream 10 mg/g) or, if necessary, brimonidine (Mirvaso® gel 3.3 mg/g) is often used for topical rosacea treatment [7]. Doxycycline (Oracea® 40 mg, capsules) is considered the “first choice” for systemic treatment [7]. The molecular and cellular targets of ivermectin (Soolantra®) and doxycycline (Oracea®) are shown in Figure 1 [1,9]. The effect of ivermectin in rosacea is probably due to two different components [5]: Firstly, due to the macrolide structure of the ivermectin molecule, an anti-inflammatory effect can be assumed and secondly, ivermectin has a neurotoxic effect and eliminates corresponding parasites in a short time. The saprophytic hair follicle mite Demodex folliculorum , which occurs in the sebaceous follicles of the face in all adults, but is up to six times more prevalent in rosacea, is a target of the antiparasitic effect. A significant improvement in the skin condition can be achieved with the reduction of Demodex mites.
Low-dose doxycycline is recommended in the guideline as the systemic treatment of first choice. According to recent findings, one molecular mechanism of action of this tetracycline is that it can inhibit the proteolytic activation of kallikrein-related peptidases that are important for the development of rosacea and the activation of cathelicidin, thereby mediating anti-inflammatory effects [8].
In general, the choice of active ingredient should be individualized according to the phenotypic characteristics of rosacea, the acuteity of the disease and the patient’s skin type [5]. The current s2k guideline recommends combining topical therapy with systemic treatment for severe, highly inflammatory forms [5]. Studies confirm the beneficial effects of combination therapy [5].
Congress: EADV Annual Meeting
Literature:
- “Pathophysiology of acne and rosacea”, Prof. Dr. Vincenzo Bettoli, MD, Session ID D1T11.1, Acne and rosacea, EADV Annual Meeting 11-13.10.2023
- Chen C, et al: Exploring the Pathogenesis and Mechanism-Targeted Treatments of Rosacea: Previous Understanding and Updates. Biomedicines 2023; 11(8): 2153.
- Dall’Oglio F, Fusto C, Micali G: Intrafamilial Transmission of Rosacea Spanning Six Generations: A Retrospective Observational Study. J Clin Aesthet Dermatol 2022; 15(2): 35-39.
- Aldrich N, et al: Genetic vs Environmental Factors That Correlate With Rosacea: A Cohort-Based Survey of Twins. JAMA Dermatol 2015; 151(11): 1213-1219.
- S2k guideline “Rosacea”, 2022, AWMF register no. 013-065.
- Searle T, et al: Rosacea and Diet: What is New in 2021? J Clin Aesthet Dermatol 2021; 14(12): 49-54.
- Swissmedic: Medicinal product information, www.swissmedicinfo.ch,(last accessed 29.11.2023)
- Kanada KN, Nakatsuji T, Gallo RL: Doxycycline indirectly inhibits proteolytic activation of tryptic kallikrein-related peptidases and activation of cathelicidin. J Invest Dermatol 2012; 132(5): 1435-1442.
- Steinhoff M, et al: Topical Ivermectin 10 mg/g and Oral Doxycycline 40 mg Modified-Release: Current Evidence on the Complementary Use of Anti-Inflammatory Rosacea Treatments. Adv Ther 2016; 33(9): 1481-1501.
DERMATOLOGIE PRAXIS 2023; 33(6): 34-35 (published on 13.12.23, ahead of print)