In Western countries, GERD (gastroesophageal reflux disease) affects approximately 20% of the population. Normally, the route leads to the gastroenterologist, but because the food pathway and the airway cross at the level of the larynx, reflux may also be of interest to pulmonologists.
There are different degrees of severity and effects of gastroesophageal reflux disease (GERD) and also different views regarding diagnosis and therapy, not least depending on where exactly the reflux occurs. The consequences of disease are classically reflux esophagitis or non-erosive reflux disease, reminded Dr. Macé Schuurmans from the Department of Pneumology at the University Hospital Zurich [1].
Symptomatically, there are esophageal syndromes and extra-esophageal syndromes. Esophageal syndromes are further subdivided into symptomatic syndromes (typical reflux syndromes, reflux chest pain syndromes) and syndromes with esophageal injury (reflux esophagitis, reflux stricture, Barrett’s esophagus, adenocarcinoma). The extraesophageal syndromes can be divided into established associations (reflux cough, laryngitis, asthma, and dental erosions) and suspected associations (sinusitis, pulmonary fibrosis, pharyngitis, recurrent otitis media).
|
Reflux symptoms among others.
|
PPI as standard therapy
Reflux may be caused by insufficiency of the lower esophageal sphincter, primarily congenital, or by inhibitory influences on the sphincter such as caffeine, alcohol, or fatty foods. Autonomic dysregulation, gastroparesis, or diabetes can also promote reflux. In addition, there are physical aspects such as obesity, constricting clothing or a tight belt. Last but not least, there are patients who are anatomically susceptible due to, for example, a hiatal hernia or systemic sclerosis.
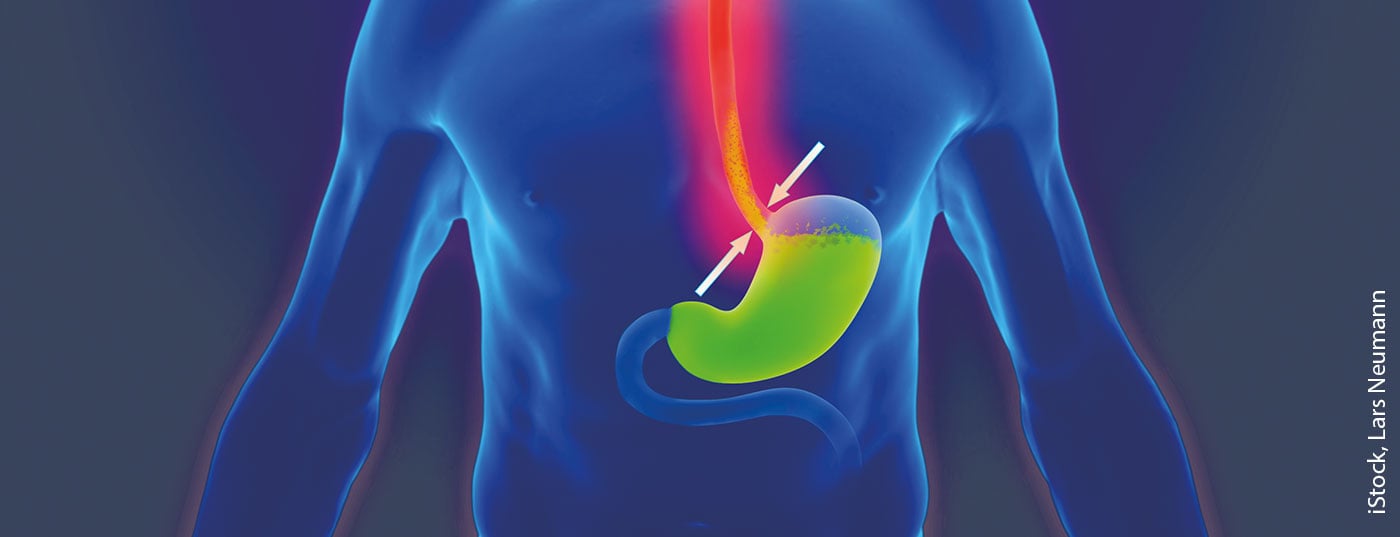
Gastroenterologists’ reflux diagnostics are esophageal manometry, esophageal pH metry, or sometimes catheter-free capsule-based pH metry. The colleagues then speak primarily of gastroesophageal reflux, whereas the phoniatrists and pulmonologists sometimes speak of laryngo-pharyngeal reflux, “because it comes up to a higher floor” (Fig. 1). Accordingly, the diagnosis is also made differently, namely with pharyngeal pH-metry.

Reflux therapy is well known, the use of proton pump inhibitors (PPI) is considered standard: pantoprazole, omeprazole, esomeprazole and others, typically taken half an hour before meals, for a sufficiently long period of time. This means that if a patient does not respond after 4 weeks, an extension to 8 weeks is quite advisable. If there is still no response, you can think about changing the product or do a course pH-metry to see if the PPI you are using also has a favorable effect on the pH. Dr. Schuurmans did not want to leave unmentioned the Nissen fundoplicatio as a surgical option for reflux treatment.
Non-specific antireflux measures
A recommended non-medicinal measure to combat reflux is to raise the bed at the head end: For a bed 2 meters long, the head end should be at least 15 cm higher than the foot end. Most people think of it as tipping up only the headboard. However, this leads to a kink in the body, possibly associated with breathing problems and back pain, for example when lying on the stomach. According to Dr. Schuurmans, however, it is more advisable to place a block of wood under the feet of the bed at the head end, for example, or alternatively between the slatted frame and its support surface. As further measures the expert mentioned:
- Eat-lie interval of at least 2 hours (so that the stomach is not too full and regurgitation does not occur then).
- No caffeinated beverages after 6 p.m. (including, for example, energy drinks or iced tea)
- Avoiding fatty foods late at night
- Weight loss (a lot of weight presses on the stomach!)
In addition to the classic, sufficiently long acid inhibition, Dr. Schuurmans recommended that the influencing factors also be taken into account, especially the aforementioned non-specific antireflux measures. However, it is not clear which of these non-drug interventions has the greatest impact because they are often either combined or not used at all in studies.
Source:
- FomF WebUp Pneumology, 7/12/2020.
InFo PNEUMOLOGY & ALLERGOLOGY 2021; 3(1): 33.