Based on new research findings, atopic dermatitis is increasingly proving to be a heterogeneous disease with a very complex pathogenesis. Great attention has recently been paid to interactions between skin microbiome disorders and the local immune system. Here, research could open up new avenues for prophylaxis and therapy. Experts spoke about current findings in Munich at the 25th Advanced Training Week for Practical Dermatology and Venereology FOBI 2016.
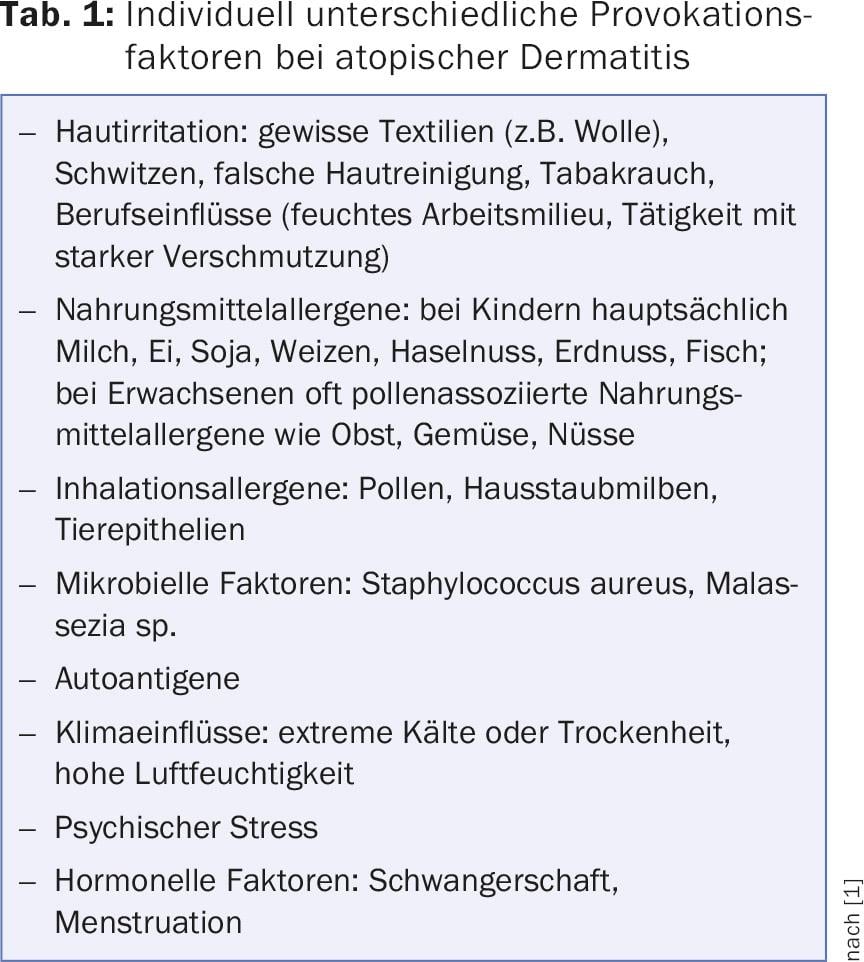
Both the initial manifestation of atopic dermatitis and renewed episodes of the disease are triggered by individually different provocation factors if there is a corresponding genetic predisposition. (Tab.1). The current interdisciplinary S2k guideline on atopic dermatitis, to which Prof. Dr. Peter Schmid-Grendelmeier also contributed as a representative of the Swiss Society of Dermatology and Venereology, recommends identifying individual provoking factors and avoiding them if possible [1]. Some parents are fixated on the idea that their young children’s neurodermatitis is triggered by food allergies, said Prof. Thomas Werfel, MD, Department of Dermatology, Hanover Medical School. A minority are actually clinically relevantly sensitized to food and exhibit allergen-associated eczema exacerbation. The lecturer particularly pointed out that after oral provocation testing, the skin must also be assessed again on the following day in order to detect a possible isolated eczema exacerbation in the absence of an immediate type reaction. In the case of grass pollen sensitization, Prof. Werfel has demonstrated that worsening of atopic eczema (flare-up reactions) can occur after inhalation pollen provocation (in the provocation chamber imitation of a summer meadow in winter). The question of whether specific immunotherapy (SIT) is worthwhile in atopic dermatitis still cannot be answered clearly, he said. Perhaps SIT is useful, but in any case it does no harm, said the speaker. According to a recent Cochrane systematic review, the efficacy of SIT in atopic eczema is weak [2]. Atopic dermatitis alone is still not considered an indication for SIT. On the other hand, there is no reason to refuse SIT in patients with atopic dermatitis if it is indicated because of concomitant allergic rhinitis.
Current treatment recommendations
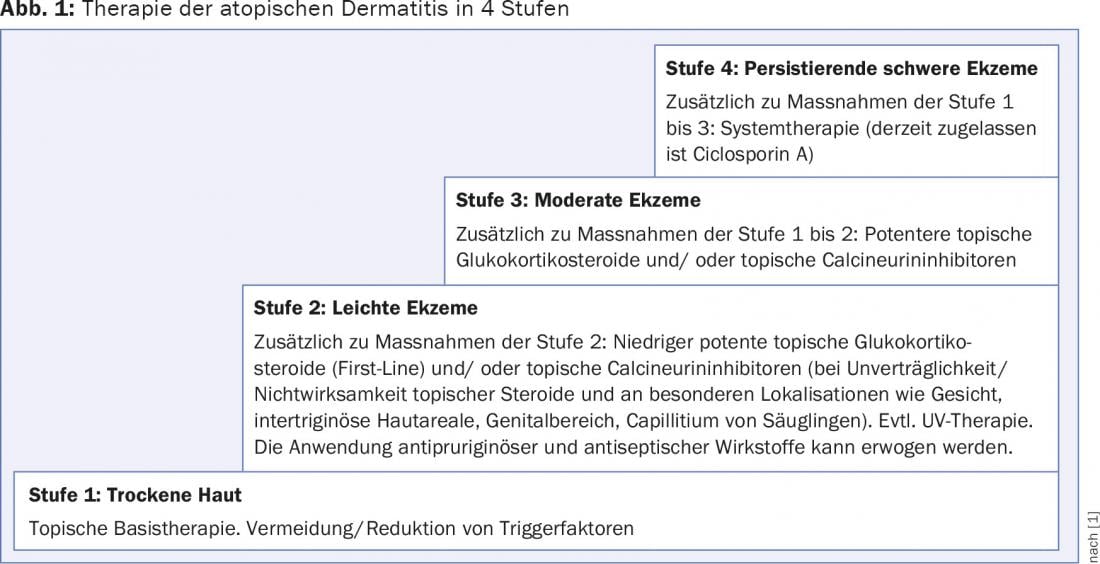
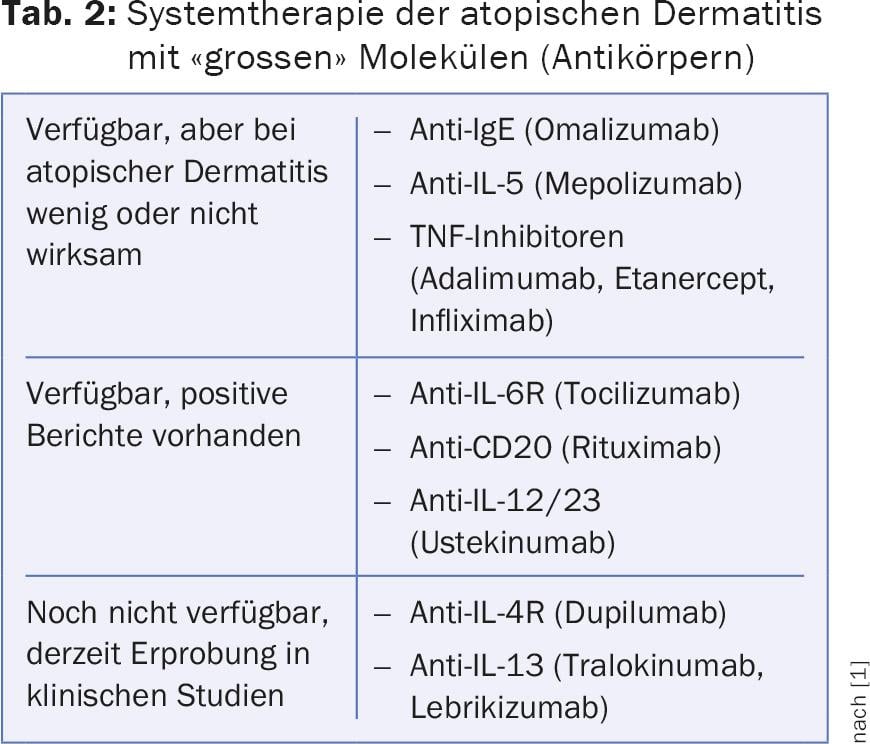
The guideline recommends a 4-stage therapy regimen adapted to the clinical manifestation (i.e., the skin condition) (Fig. 1) . In stage 1, the dry skin is treated with topical basic therapeutics. Although mutations of skin barrier protein genes are present in only a minority of patients (filaggrin mutations with loss of function in 25-30%), consistently all patients have a relative filaggrin defect in the eczema skin. This is caused by mediators of atopic inflammation (e.g. interleukin 4 and 13), which downregulate the production of skin barrier proteins. Mild to moderate eczema is usually treated topically with anti-inflammatory agents (glucocorticoids, calcineurin inhibitors) (stages 2 and 3). Systemic therapy is recommended for persistent severe eczema (stage 4). Severe forms of atopic eczema in adults are particularly difficult to manage, the speaker said. A lot is currently happening in the search for new system therapies: Numerous “small” and “large” molecules are being tested in clinical trials (Tab. 2).
Disturbances of the skin microbiome in atopic dermatitis.
In terms of numbers, we have as many bacteria, viruses and fungi in and on our bodies (1013 cells of the microbiome) as we have endogenous cells, reported Prof. Dr. Thomas Bieber, Clinic for Dermatology and Allergology, University of Bonn. Our 1013 body cells are therefore by no means alone, but live in close symbiotic company. There are 106 bacteria, viruses and fungi of 250 to 500 different species per square centimeter on the skin and they are an important part of the skin barrier. Diversity makes healthy and disturbed diversity (dysbiosis) means disease state, the speaker said. Surprisingly, the bacteria, viruses and fungi are not only located on the skin surface, but also deep in the dermis, without causing an inflammatory reaction there. It has long been known that Staphylococcus aureus is a constant companion of patients with atopic dermatitis and that episodes of impetiginization occur repeatedly in affected young children. During an acute eczema phase, the diversity of the microbiome decreases and the proportion of Staphylococcus aureus increases (dysbiosis) [3]. Studies show that local application of extracts of gram-negative germs can favorably influence the immune response of keratinocytes by binding to toll-like receptors and reduce the inflammatory response. The lecturer reported that a trend towards normalization was also observed in the disturbed microbiome after application of such an extract (contained in Lipikar Baume AP+).
Literature:
- Werfel T, et al: S2k guideline on diagnosis and treatment of atopic dermatitis – short version. Allergo J Int 2016; 25: 82-95.
- Tam HH, et al: Specific allergen immunotherapy for the treatment of atopic eczema: a Cochrane systematic review. Allergy 2016; 71: 1345-1356.
- Kong HH, et al: Temporal shifts in the skin microbiome associated with disease flares and treatment in children with atopic dermatitis. Genome Res 2012; 22: 850-859.
DERMATOLOGIE PRAXIS 2016; 26(5): 34-41











